Your 2026 Medical Coding Audit Checklist for Compliance & Clean Claims

Medical coding is where clinical care becomes revenue, and when coding is inaccurate or non-compliant, denials, delays, and audit exposure follow quickly.
The challenge is that coding is becoming more complex.
In a recent Black Book survey, 85% of HIM professionals said most coding discrepancies stem from system complexity, and with ICD-11 approaching, 80% worry errors will increase without stronger audit controls.
This is why a structured medical coding audit checklist is essential.
With rising claim volumes and fast-changing payer rules, organizations need an audit process that is consistent, repeatable, and able to keep pace with regulatory and documentation changes.
This guide explains what to review in a coding audit and why each step matters for accuracy, compliance, and reimbursement outcomes.
At a glance:
- A medical coding audit checklist creates a consistent, defensible way to verify documentation accuracy, correct code selection, and payer compliance.
- It reduces denials by ensuring diagnoses, procedures, E/M levels, and modifiers are fully supported and aligned with ICD-10, CPT/HCPCS, and payer rules.
- The strongest checklists cover documentation completeness, code specificity, medical necessity, payer policy requirements, and high-risk denial indicators.
- Audit reliability improves when the checklist is tailored to specialties, payer mix, past denial trends, and current regulatory guidance.
- Effective programs pair the checklist with regular audit cadence, CDI collaboration, provider education, and clear corrective action plans.
- AI tools like RapidClaims strengthen accuracy by catching coding and compliance issues in real time, improving clean-claim rates and reducing denials.
What Is a Medical Coding Audit Checklist?
A medical coding audit checklist is a structured list of criteria used to evaluate whether clinical documentation and assigned codes are accurate, compliant, and aligned with payer rules. It creates a consistent way for coding, HIM, and revenue cycle teams to review charts, identify discrepancies, and correct issues before they lead to denials or audit exposure.
At its core, the checklist ensures three things:
1. Documentation supports the codes assigned. Auditors confirm that diagnoses, procedures, and E/M levels are fully backed by the provider’s notes and meet medical necessity requirements.
2. Codes follow the latest standards and payer policies. This includes ICD-10, CPT, HCPCS, modifier use, and specialty-specific guidelines.
3. Claims meet internal and external compliance expectations. The checklist helps teams spot errors that can trigger payer denials, repayments, or external audits, such as incorrect E/M leveling, missing documentation, or unbundling risks.
For healthcare organizations with growing volumes and complex revenue streams, the checklist serves as the quality control layer.
Why a Medical Coding Audit Checklist Is Important
A medical coding audit is only as effective as the structure behind it. That structure is the checklist. Here is why it matters:

1. It Standardizes How Audits Are Performed
Without a checklist, coders and auditors rely on their own judgment about what to review. A structured checklist eliminates inconsistency and creates a uniform review process across teams and locations.
2. It Reduces the Risk of Missed Errors
Coding discrepancies often hide in the details. A checklist ensures key elements such as documentation support, code specificity, modifier use, and medical necessity are never overlooked.
RapidClaims RapidCode takes this further. Our AI-powered coding engine processes 1000+ charts per minute, delivers a 70% reduction in denials, and integrates instantly with your workflow. Request a demo to see how automation strengthens coding accuracy from day one.
3. It Creates a Repeatable Process That Scales
As claim volumes grow, organizations need a method that works regardless of who performs the review. A checklist makes the audit predictable, trainable, and easy to operationalize.
4. It Strengthens Compliance and Defensibility
When organizations can show that every chart was reviewed using a consistent framework, they are better prepared for payer audits, appeals, and compliance inquiries.
5. It Highlights Patterns and Improvement Opportunities
Using the same checklist across multiple audits reveals systemic issues such as provider documentation gaps, coder training needs, or specialty-specific problem areas.
In short, the checklist is what makes the audit consistent, reliable, and defensible.
Also read: Different Types of Medical Coding and Their Role in Healthcare
Key Components of a Medical Coding Audit Checklist
An effective medical coding audit checklist is built around a few core components that help teams review charts consistently and identify issues early. These components guide what every audit must cover, regardless of specialty, payer, or documentation style.
- Documentation Requirements: Defines what must be present in the medical record to support diagnoses, procedures, and E/M levels.
- Coding Standards and Guidelines: Covers ICD-10-CM, CPT, and HCPCS rules, code specificity, and correct modifier use.
- Medical Necessity Criteria: Ensures each service is clinically justified and aligned with payer coverage rules.
- Payer Policy Requirements: Incorporates LCDs, NCDs, bundling rules, frequency limits, and payer-specific edits.
- Risk and Error Indicators: Highlights common claim denial reasons, specialty-specific risk areas, and historical error patterns.
These components form the foundation of any reliable medical coding audit process. The next section outlines a complete checklist you can use.
The Complete Medical Coding Audit Checklist
A reliable medical coding audit checklist gives teams a consistent way to review charts, validate documentation, and ensure that every claim meets coding and compliance standards.
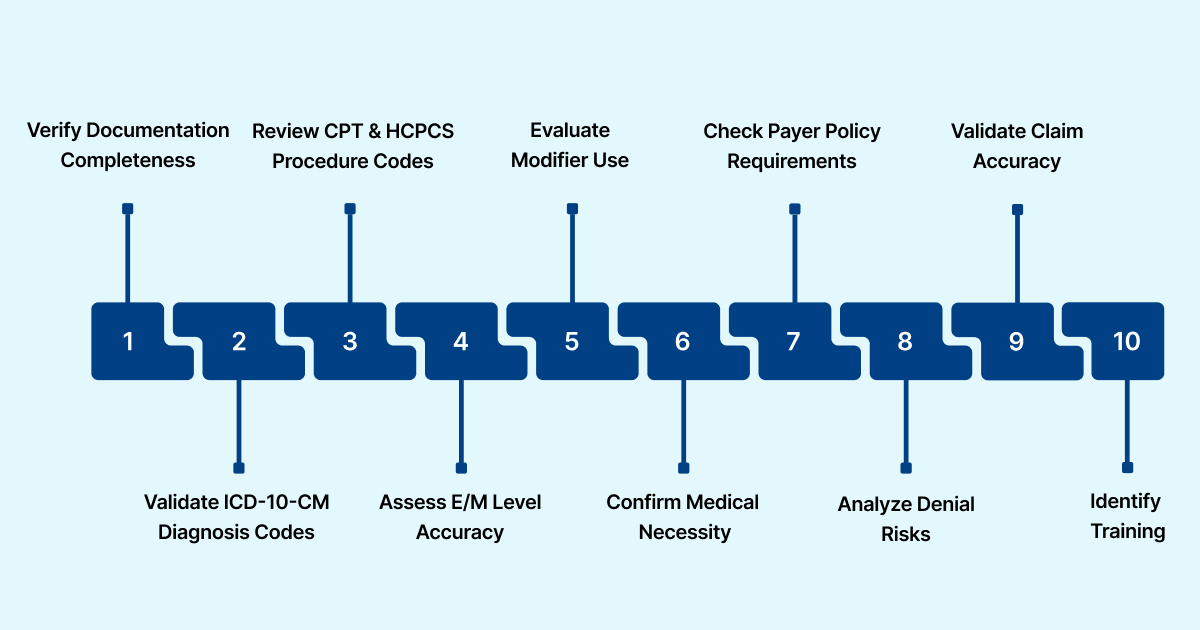
Below is a comprehensive checklist you can use as-is or tailor to your organization’s specialties and payer mix.
Verify Documentation Completeness
- Confirm provider notes are present, signed, and dated
- Check HPI, exam findings, and medical decision-making for clarity
- Ensure documentation supports all diagnoses and procedures
- Identify missing or unclear details that require provider clarification
Validate ICD-10-CM Diagnosis Codes
- Confirm accuracy and specificity of assigned diagnoses
- Ensure codes match the documented condition
- Check laterality, episode of care, and severity
- Review for unsupported or omitted diagnoses
Review CPT and HCPCS Procedure Codes
- Verify procedures are fully documented
- Confirm proper code selection for services rendered
- Check for incorrect or outdated codes
- Validate alignment with payer coverage rules
Assess E/M Level Accuracy
- Confirm documentation supports the billed E/M level
- Validate time-based visits, when applicable
- Check for overcoding or undercoding
- Ensure guidelines for problem-focused, expanded, detailed, or comprehensive assessments are met
Evaluate Modifier Use
- Ensure modifiers are appropriate and supported
- Identify unbundling or duplicate billing risks
- Check payer-specific rules for modifiers such as 25, 59, 76, and 91
Confirm Medical Necessity
- Ensure documented diagnoses justify services provided
- Verify alignment with payer coverage policies
- Review local and national coverage determinations (LCDs and NCDs)
- Flag services with insufficient justification
Check Payer Policy Requirements
- Confirm adherence to commercial and government payer rules
- Ensure documentation meets frequency and coverage limits
- Validate claim edits and bundling rules
- Identify discrepancies with organization-specific payer contracts
Analyze Denial Risks and Historical Patterns
- Review common coding-related denial reasons
- Check for recurring patterns across providers or coders
- Flag specialty-specific risk areas
- Identify charts requiring deeper review or education
Validate Claim Accuracy and Completeness
- Confirm codes, units, and charges match the encounter
- Verify all necessary supporting documents are attached
- Ensure consistency across documentation, coding, and billing
- Identify missing elements that could delay or deny the claim
Identify Training and Compliance Issues
- Note trends that suggest coder skill gaps
- Flag patterns tied to specific providers or specialties
- Recommend corrective actions or documentation education
- Document audit findings for internal reporting and follow-up
This checklist covers the core elements every coding audit should include, but no two organizations operate the same way.
The next step is tailoring it to your specialties, payer mix, and internal workflows so it becomes a reliable tool for daily use.
How to Create a Medical Coding Audit Checklist That Works
A checklist is only effective if it reflects your organization’s documentation patterns, specialties, payer mix, and compliance priorities. Here is how to create a checklist that consistently delivers accurate and defensible audit results:
1. Start With Your Highest-Risk Areas
Review past denials, payer audits, and internal QA reports. Focus your checklist on:
- Services with frequent coding discrepancies
- Specialties with complex documentation
- High-volume encounters
- Providers with recurring documentation issues
This ensures the checklist addresses the areas most likely to impact revenue and compliance.
2. Incorporate Payer and Regulatory Requirements
Your checklist must reflect current ICD-10, CPT, and HCPCS guidelines, as well as:
- Local and National Coverage Determinations
- Commercial payer policies
- E/M guidelines
- Modifier rules
Update this regularly as payers revise rules and CMS releases new guidance.
3. Build Clear, Actionable Review Steps
Each checklist item should be specific enough that any auditor or coder can follow it consistently. Replace vague instructions like “Check documentation” with precise steps, such as:
- “Confirm two supporting elements for the diagnosis.”
- “Validate laterality and specificity for ICD-10 codes.”
- “Verify provider signature and date.”
Clarity reduces variability across auditors.
4. Align the Checklist With Your Specialties
Different specialties have different coding challenges. Tailor sections for:
- Emergency Medicine
- Radiology
- Nephrology
- OBGYN
- Internal Medicine
- Labs and Home Health
- Ambulatory Surgery
By aligning the checklist with your service lines, you make it more accurate and more relevant.
5. Make the Checklist Easy to Use at Scale
A checklist should support quick, repeatable reviews. Consider:
- Grouping items by documentation, coding, and compliance
- Using simple yes/no or pass/fail indicators
- Keeping the list concise enough to complete efficiently
The more usable it is, the more consistently it will be applied.
6. Involve Both Coding and Compliance Teams
Strong checklists reflect both coder expertise and compliance oversight. Involving multiple stakeholders ensures the checklist covers:
- Coding accuracy
- Documentation sufficiency
- Medical necessity
- Fraud, waste, and abuse risks
This creates a balanced and defensible audit tool.
7. Test, Refine, and Update Regularly
Pilot the checklist on a sample of charts, gather feedback, and refine unclear steps. Revisit the checklist quarterly or whenever major regulatory or payer changes occur. A great checklist evolves with your coding environment.
Also read: Top Medical Coding Software to Spot CPT/HCPCS Coding Errors
How to Get the Most Out of Your Audit Checklist
A medical coding audit checklist is most effective when it is applied consistently and integrated into broader quality assurance and documentation improvement processes.
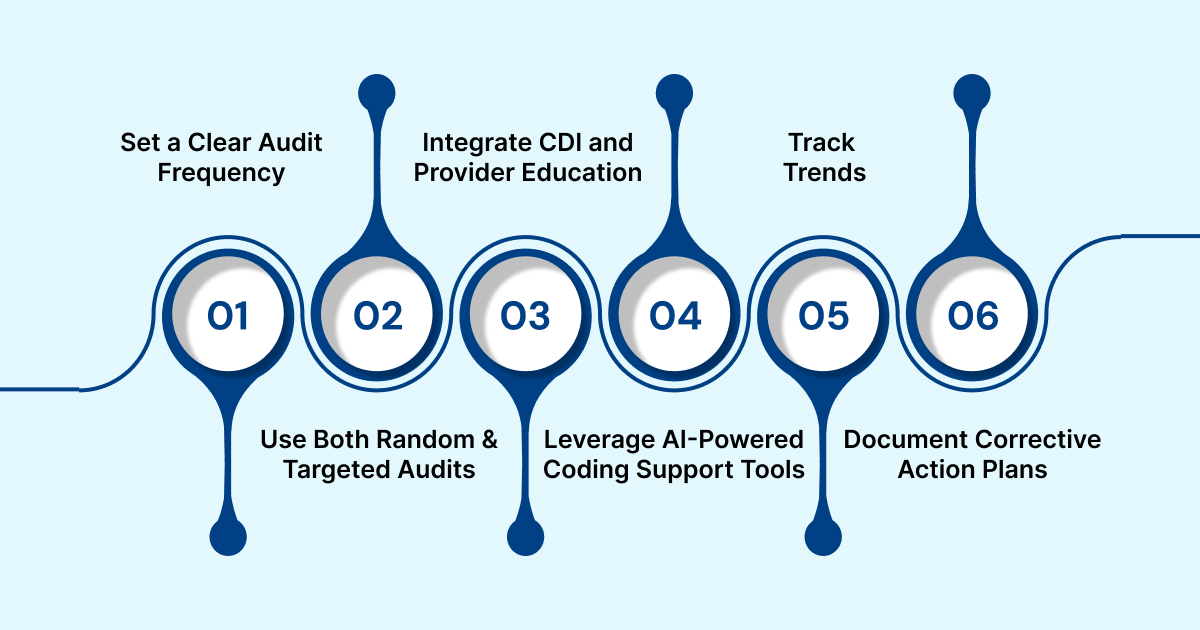
The following best practices help organizations get the most value from their audit efforts.
1. Set a Clear Audit Frequency
The right cadence depends on your volume, specialties, and risk profile, but most organizations benefit from a mix of:
- Monthly routine audits for general oversight
- Quarterly comprehensive audits for deeper evaluation
- Ad hoc audits when payer rules change or new services launch
A predictable schedule ensures ongoing visibility into coding accuracy rather than relying on occasional, reactive reviews.
2. Use Both Random and Targeted Audits
Random audits give an unbiased view of everyday coding performance, while targeted audits focus on areas with known issues. Prioritize charts:
- With past coding discrepancies
- In high-risk specialties
- Tied to high denial rates
- From providers with recurring documentation gaps
Balancing both approaches provides a more accurate picture of overall performance and emerging risk.
3. Integrate CDI and Provider Education
Audit findings should not stay within the coding team. Coding accuracy depends heavily on documentation quality, so collaboration with Clinical Documentation Integrity (CDI) and provider teams is essential.
Use audit results to support:
- Clarification requests
- Documentation improvement initiatives
- Specialty-specific education sessions
- Updates to internal documentation guidelines
When coders, CDI, and providers work together, accuracy improves at the source.
4. Leverage AI-Powered Coding Support Tools
Modern revenue cycle teams benefit from technology that can prevent errors before they reach the audit stage.
RapidClaims is an AI-powered revenue cycle intelligence platform that supports accurate coding, stronger documentation, real-time compliance, and proactive denial prevention.
Instead of relying solely on manual reviews, you can use AI to reduce preventable discrepancies and make the audit process more focused and efficient.
Here is how we can help:
- RapidCode: Automates routine chart coding with high accuracy and full guideline coverage, reducing basic errors and allowing coders to focus on complex cases.
- RapidScrub: Flags incorrect codes, invalid pairings, modifier issues, and policy violations before submission, lowering denial risk and minimizing audit rework.
- RapidCDI: Enhances documentation clarity and specificity at the point of care, reducing discrepancies tied to unsupported diagnoses or incomplete E/M details.
With RapidClaims, healthcare organizations see measurable impact within weeks, including:
- Greater than 98% clean claim rates
- 40% reduction in denials
- 2 hours saved per coder per day
Talk to an expert to see how AI strengthens compliance and reimbursement from day one.

5. Track Trends and Close Feedback Loops
Individual chart reviews are helpful, but the real value comes from spotting patterns over time. Monitor trends involving:
- Frequently misused codes
- Common documentation gaps
- Specialty-specific discrepancies
- Recurring payer denial reasons
Create a feedback loop where findings are shared with coding leadership, CDI teams, and providers so issues can be corrected proactively.
6. Document Corrective Action Plans
Every audit should produce actionable next steps. Document findings clearly and outline follow-up actions such as:
- Coder retraining
- Provider documentation guidance
- Updates to internal coding rules
- Additional targeted audits
- Process changes to prevent repeat issues
A structured corrective action plan ensures audit results lead to measurable improvements rather than one-time observations.
Wrapping Up
A strong medical coding audit checklist helps organizations protect revenue, maintain compliance, and reduce preventable denials. When teams follow a structured approach, they catch issues earlier, document more consistently, and strengthen coding accuracy across every specialty.
The challenge is that manual audits cannot keep pace with changing payer rules and rising documentation complexity.
This is where platforms like RapidClaims make a measurable difference. By adding continuous coding checks, real-time compliance validation, and automated denial prevention, teams move from reactive auditing to proactive accuracy management.
FAQs
1. What are the five audit checklists?
The five core areas reviewed in most medical coding audits are documentation completeness, diagnosis code accuracy, procedure code accuracy, modifier appropriateness, and medical necessity or payer policy compliance.
2. How do you audit medical coding?
To audit medical coding, reviewers select a sample of charts and confirm that documentation supports the assigned codes, ICD-10 and CPT/HCPCS codes are accurate, E/M levels are correct, modifiers are used appropriately, and payer rules are fully met.
3. What are the 5 C’s of audit findings?
The 5 C’s of audit findings are Correct, Complete, Compliant, Consistent, and Clear. These principles help ensure audit results are thorough, defensible, and actionable.
4. How often should healthcare organizations perform coding audits?
Most organizations conduct monthly or quarterly audits, but high-volume specialties or high-risk services may require more frequent review. Continuous auditing through AI tools can reduce the need for large manual audits.
5. What are the most common errors found during coding audits?
Typical issues include incomplete documentation, incorrect E/M levels, missing or incorrect modifiers, outdated payer rules, and diagnosis codes lacking required specificity.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






