.webp)
Neurology & Neuromuscular Procedures: CPT Codes Explained
In 2024, medical coding audits intensified. Retrospective reviews increased by 10% and prospective audits rose by 275% compared to the previous year. The message is clear, oversight is growing, and accuracy matters more than ever.
While this trend affects all specialties, it poses unique challenges in neurology, where coding complexity is already high. For professionals working with neurology and neuromuscular procedures, the accuracy of CPT codes is not optional. It is the safeguard against denials, compliance risks, and lost revenue.
In this blog, you'll learn key CPT codes neurology and Neuromuscular, common challenges, compliance essentials, and best practices to strengthen billing accuracy.
TL;DR (Key Takeaway)
- Audit activity is surging, highlighting the need for precise neurology CPT coding.
- The CPT range 95700–96020 covers diagnostic, therapeutic, and monitoring procedures.
- Accurate coding ensures proper reimbursement, reduces denials, and supports compliance.
- Challenges include clinical complexity, frequent CPT updates, high audit risk, and interdisciplinary overlap.
- Best practices involve meticulous documentation, AI-assisted coding, audit-ready workflows, and ongoing staff training.
Table of Contents:
- Overview on Neurology & Neuromuscular Procedures CPT Codes
- Why Accurate Neurology Coding Matters for Audit Compliance?
- Common Neurology & Neuromuscular CPT Codes
- Challenges in Neurology and Neuromuscular Coding
- Key Strategies for Coding Neurology & Neuromuscular Procedures
- Conclusion
- Frequently Asked Questions (FAQs)
Overview on Neurology & Neuromuscular Procedures CPT Codes
Neurology and neuromuscular procedures include complex diagnostic and therapeutic services that require precise CPT coding for accurate billing and compliance. These codes encompass a wide range of procedures, including electrodiagnostic testing (EEG, EMG, NCS), interventional pain management, and advanced neurosurgical techniques.
Accurate coding helps medical coders secure proper reimbursement, minimize claim denials, and adhere to payer documentation requirements, which is especially important for high-cost, closely monitored procedures.
Why Accurate Neurology Coding Matters for Audit Compliance?

Neurology and neuromuscular procedures often involve high-cost diagnostic tests, advanced monitoring, and complex therapeutic interventions. Because of this complexity, these services face closer scrutiny from payers and regulatory bodies.
Key reasons why accuracy is critical for audit compliance include:
- Regulatory Oversight: Neurology procedures, such as EEGs, EMGs, and nerve conduction studies, are frequently audited due to their cost and potential for overutilization.
- Proper Reimbursement: Correct CPT selection avoids undercoding (leading to revenue loss) and overcoding (leading to compliance violations or fraud investigations).
- Documentation Alignment: Coding must reflect the exact procedure performed, frequency, and duration as documented in the medical record.
- Audit Preparedness: Clean, accurate coding creates a defensible position during payer or RAC (Recovery Audit Contractor) reviews.
- Minimized Risk Exposure: Errors in coding neurology services may trigger payer audits, penalties, or even compliance investigations under federal guidelines.
Accurate neurology coding is not just about reimbursement; it directly protects providers from audit risks while ensuring patients’ services are reported with integrity and precision.
Common Neurology & Neuromuscular CPT Codes
The CPT range 95700–96020 covers neurology and neuromuscular procedures within the Medicine section, encompassing diagnostic, therapeutic, and monitoring services. Below is a breakdown of the 15 major subranges recognized by AAPC, with technical scope and clinical use cases.
1. 95700–95811 - Sleep Medicine Testing & Long-term EEG
This range covers extended EEG monitoring and polysomnography, often performed in sleep labs or inpatient units. Codes capture whether sleep staging, technologist review, or physician interpretation is included and are commonly used for sleep apnea diagnosis, seizure detection, and monitoring nocturnal events.
2. 95812–95830 - Routine EEG Procedures
These codes represent standard EEGs of varying durations (20–60 minutes or longer). They are fundamental for evaluating epilepsy, encephalopathies, and altered mental status. Correct documentation of time and recording conditions is critical for accurate coding.
3. 95829–95836 - Electrocorticography (ECoG)
Electrocorticography involves direct cortical recording, typically intraoperatively. It is used in epilepsy surgery planning and mapping the eloquent cortex. The codes capture electrode placement, monitoring, and interpretation during the procedure.
4. 95836–95857 - Range of Motion Testing
This subrange codes the quantitative measurement of joint mobility, often using devices like goniometers or inclinometers. Although musculoskeletal in nature, it falls within neuromuscular coding for assessing conditions such as spasticity or peripheral nerve injury.
5. 95860–95872 - Electromyography (EMG) Procedures
These codes cover needle EMG performed on specific muscles or groups. EMG helps assess motor unit function, peripheral neuropathies, radiculopathies, and myopathies. Code selection depends on whether limited or extensive muscle sets are examined.
6. 95873–95887 - Ischemic Muscle Testing & Chemodenervation Guidance
This range includes muscle ischemia testing and EMG/ultrasound guidance for chemodenervation (e.g., botulinum toxin injections). Documentation should specify muscles tested or injected, as coverage and reimbursement often hinge on clear procedural notes.
7. 95905–95913 - Nerve Conduction Studies (NCS)
These codes capture motor, sensory, and mixed nerve conduction testing. The correct code depends on the number of studies performed. They are vital for diagnosing peripheral neuropathy, entrapment syndromes, and neuromuscular junction disorders.
8. 95919–95924 - Autonomic Function Testing
Covers procedures assessing autonomic nervous system integrity, such as tilt table testing, heart rate variability, and sudomotor testing. Essential for diagnosing dysautonomia, orthostatic intolerance, and diabetic autonomic neuropathy.
9. 95925–95941 - Evoked Potentials & Reflex Testing
These codes represent somatosensory, visual, brainstem auditory, and motor evoked potentials. They are used to evaluate neural pathway conduction in conditions like multiple sclerosis, spinal cord injury, or intraoperative monitoring.
10. 95940–95941 - Intraoperative Neurophysiology Monitoring
Dedicated to real-time monitoring during surgery, including EEG, EMG, or evoked potentials. These services help reduce surgical complications, especially in spinal and cranial procedures. Requires detailed intraoperative logs for billing compliance.
11. 95726–95954- Special EEG Testing
This category includes advanced or less common EEG procedures, such as mapping with sphenoidal electrodes or digital spike analysis. These tests are adjuncts for epilepsy surgery planning or seizure localization.
12. 95970–95984 - Neurostimulator Analysis & Programming
Covers interrogation, programming, and reprogramming of implanted neurostimulators (e.g., spinal cord, vagus nerve, or deep brain stimulators). Code selection depends on complexity and whether multiple parameters were adjusted.
13. 95990–95999 - Other Neurology & Neuromuscular Procedures
This includes miscellaneous services such as refilling and maintenance of intrathecal pumps. Documentation should capture drug type, reservoir volume, and pump adjustments for proper coding.
14. 96000–96004 - Motion Analysis Procedures
Applies to gait and motion analysis, often using computer-assisted 3D systems. These studies are integral for surgical planning in cerebral palsy, post-stroke rehabilitation, and prosthetic evaluation.
15. 96020 - Functional Brain Mapping
This code is specific to brain mapping using direct cortical stimulation. Often performed during neurosurgery, it identifies eloquent areas of the brain to preserve motor, sensory, or language function during resections.
Given the complexity of neurology and neuromuscular CPT coding, providers face manual, error-prone workflows that create 20–40% revenue leakage. RapidClaims delivers end-to-end revenue-cycle automation across coding, documentation, and denial management, achieving a 98 % clean-claim rate and 30-day time-to-value. With AI-driven insights, it reduces denials by 40%, enhances coder productivity by 170%, and supports audit-ready, compliant workflows.
Also Read: HCPCS Code Lookup Tool: The Efficient Way to Find CPT Codes & Reduce Billing Errors
Challenges in Neurology and Neuromuscular Coding
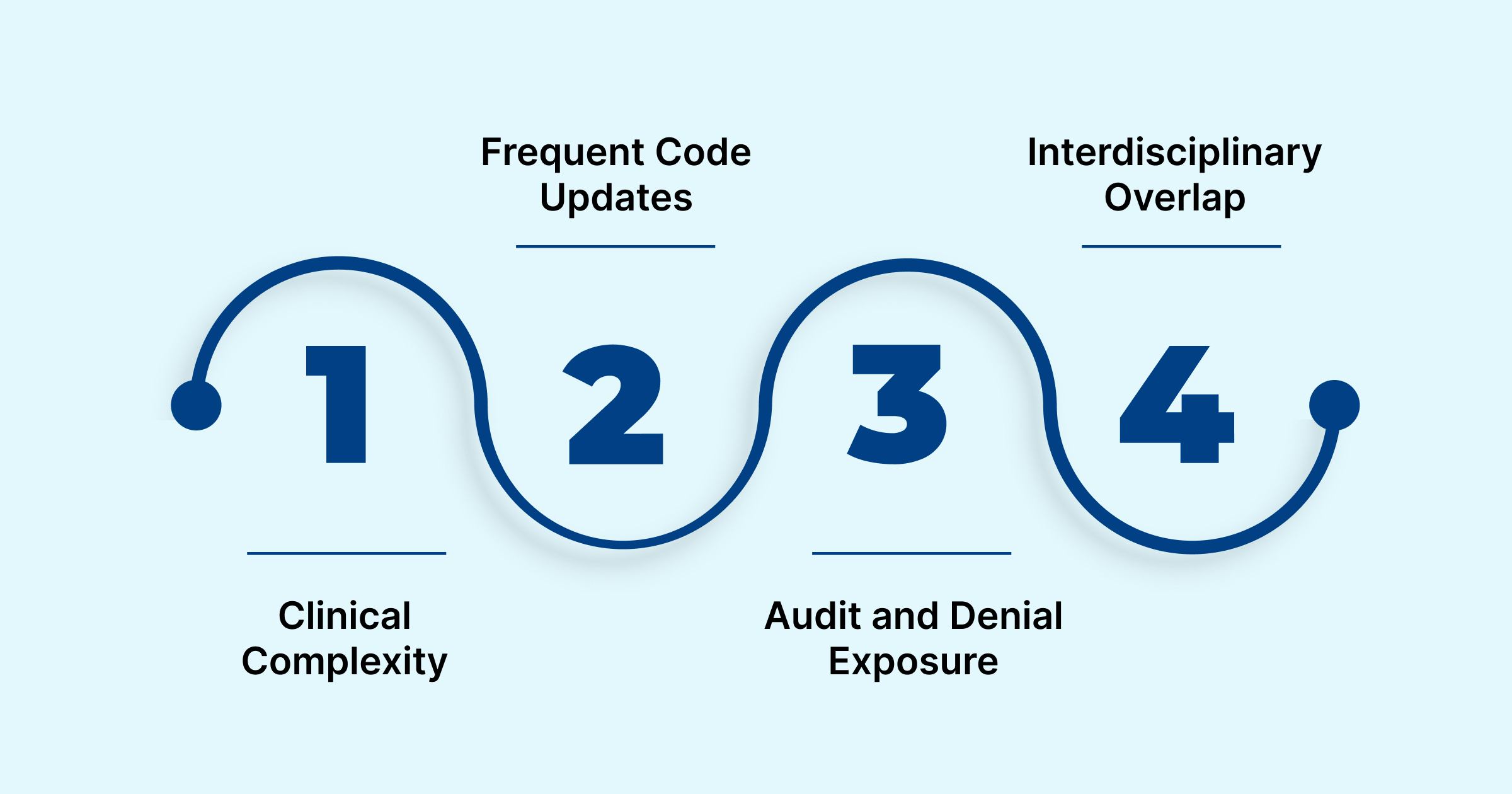
Coding neurology and neuromuscular procedures is rarely straightforward. The specialty’s complexity, frequent code updates, and high audit risk create unique challenges for medical coders and billing teams. Major obstacles include:
- Clinical Complexity: Neurology covers a wide range of conditions, from seizures and migraines to multiple sclerosis and motor neuron disease, making accurate CPT and ICD code selection technically demanding.
- Frequent Code Updates: With annual CPT changes, including 270 new codes, 112 deletions, and 38 revisions in 2025, staying compliant requires continuous training and reference to AMA updates.
- Audit and Denial Exposure: Neurology is a high-cost specialty under close payer scrutiny. Even minor errors in code specificity or documentation can trigger denials, rejections, or audit flags.
- Interdisciplinary Overlap: Many neurology services, such as cognitive assessment, pain management, or physical therapy, intersect with other specialties, creating reimbursement gray zones and requiring coders to understand multi-specialty documentation.
To address these challenges, RapidClaims offers an AI-powered platform that automates coding, clinical documentation, and denial prevention. Its modules, including RapidCode and RapidScrub, help practices achieve higher accuracy, faster reimbursements, and reduced audit exposure. By integrating seamlessly with existing EHRs, RapidClaims enables coders and clinicians to work efficiently while staying fully compliant with payer requirements.
Key Strategies for Coding Neurology & Neuromuscular Procedures
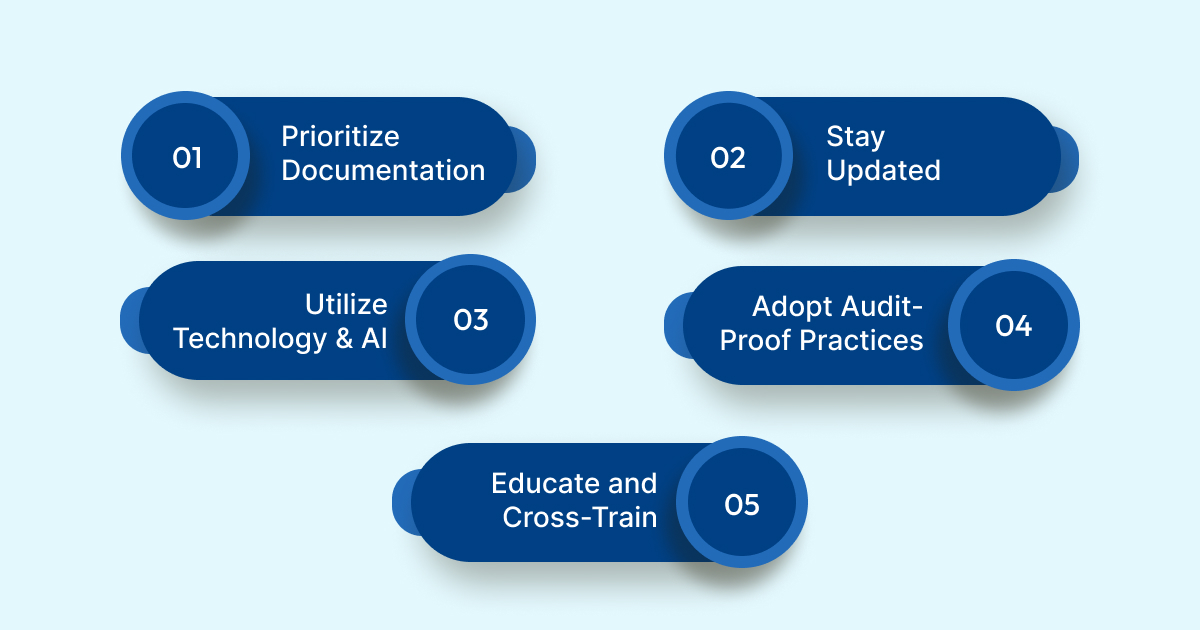
Given the complexity and audit sensitivity of neurology services, coders must adopt structured practices to maintain accuracy, compliance, and efficiency. The following strategies are essential:
1. Prioritize Documentation
Align ICD-10 diagnoses precisely with CPT codes and ensure physician notes capture duration, nerves or muscles tested, and clinical rationale. Supporting evidence, such as imaging or prior treatments, strengthens medical necessity.
2. Stay Updated
Monitor annual CPT updates from AMA and CMS, and track specialty guidelines from groups like the American Academy of Neurology. Regular updates prevent miscoding and ensure reimbursement aligns with evolving standards.
3. Utilize Technology and AI
Implement AI-powered coding platforms, such as RapidClaims, to minimize manual errors, identify missing documentation, maintain compliance, and streamline the submission of timely and accurate claims.
4. Adopt Audit-Proof Practices
Combine retrospective and prospective reviews to detect errors early. Benchmark coding teams to maintain 95%+ accuracy and establish strong audit defense with compliance-ready documentation.
5. Educate and Cross-Train
Provide continuous coder training on neurology-specific procedures, modifiers, and payer rules. Encourage collaboration with clinicians to improve documentation habits that directly support coding compliance.
With these best practices in place, we can now summarize the key takeaways and bring everything together in a clear, actionable conclusion.
Conclusion
Neurology and neuromuscular procedures involve complex CPT coding. Errors in documentation, incorrect ICD-10/CPT alignment, or missed modifiers can delay reimbursements and trigger audits. Following coding guidelines and best practices helps healthcare teams improve accuracy, compliance, and revenue.
To address these hurdles, RapidClaims offers an AI-powered revenue cycle intelligence platform. With modules like RapidCode for coding automation, RapidScrub for denial prevention, and RapidCDI for clinical documentation optimization, the platform helps practices achieve cleaner claims, faster reimbursements, and reduced audit exposure.
Ready to transform your neurology coding workflow into a seamless, error-free process? Request a Free Demo with RapidClaims today, and see how your team can process more claims, stay audit-ready, and achieve modern coding efficiency.
Frequently Asked Questions (FAQs)
1. How do I determine the appropriate CPT code for a long-term EEG study?
A. For long-term EEGs, CPT codes 95717–95720 cover inpatient monitoring with continuous physician access. Ambulatory studies with periodic downloads may not fit these codes. In such cases, the unlisted code 95999 can be used, provided that proper documentation is included.
2. I need to code for neuromuscular reeducation. What documentation is required?
A. CPT 97112 requires documentation of the patient’s neuromuscular assessment and medical necessity to support its use. Record specific techniques used, treatment duration, and patient response. This ensures accurate billing and supports compliance during audits.
3. What are the billing guidelines for nerve conduction studies?
A. Limited studies use CPT 95870, billed per extremity or tested muscle. Codes 95860–95864 apply to comprehensive testing. Always document muscles tested and results to avoid claim denials.
4. How do I handle coding for unlisted neurology procedures?
A. Use CPT 95999 for procedures without a specific code. Include a detailed description, medical necessity, and outcomes. Check payer-specific guidelines for submission requirements.
5. I’m coding for a neurology consultation. Which CPT codes should I use?
A. Consultations generally fall within 95700–96020. Choose codes based on service complexity, setting, and documentation. Reviewing the medical record ensures accurate and compliant billing.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
Related Post
Top Products

%201.png)








