.webp)
Top Medical Coding Software to Spot CPT/HCPCS Coding Errors

How many claims can your practice afford to lose to coding errors each year? Even minor coding mistakes can lead to revenue leakage, delayed reimbursements, and compliance concerns that directly impact outpatient practices.
To overcome these challenges, many providers are now adopting software used by hospitals to help identify CPT/HCPCS coding errors, extending accuracy and reliability into ambulatory care. The market validates this shift: valued at $18.88 billion in 2025, medical coding software is projected to reach $27.71 billion by 2034. Thus, highlighting its vital role in reducing denials and sustaining revenue.
In this blog, you’ll learn how medical coding software enables outpatient practices to strengthen accuracy, efficiency, and financial outcomes.
TL;DR (Key Takeaways)
- Medical coding software converts diagnoses, procedures, and treatments into CPT/HCPCS codes for accurate billing and compliance.
- It reduces claim denials, optimizes revenue, and improves workflow efficiency in hospitals and outpatient practices.
- Features include automated code validation, modifier management, documentation-to-code matching, denial prevention, audit simulation, and AI-assisted EHR integration.
- Top platforms include RapidClaims, 3M™ CodeFinder, Optum Pro Encoder, Oracle Health EHR, and AAPC Codify.
- Effective use requires phased implementation, ongoing coder training, routine updates, feedback loops, and continuous monitoring.
Table of Contents:
- What is Medical Coding Software?
- Why Should You Use Software to Identify Coding Errors?
- Essential Features of Medical Coding Software
- How Does Medical Coding Software Work?
- Top 5 Medical Coding Software for CPT/HCPCS Error Detection
- Choosing the Right Medical Coding Software for Your Hospital
- Best Practices for Implementation and Ongoing Use
- Conclusion
- Frequently Asked Questions (FAQs)
- Conclusion
What is Medical Coding Software?
Medical coding software for outpatient clinics and medical practices is a digital solution designed to convert patient diagnoses, treatments, and procedures into standardized codes, such as CPT and HCPCS. By automating code assignment and cross-checking documentation, this software helps practices maintain compliance with insurance requirements, reduce human errors, and ensure accurate reimbursement.
Unlike general billing software, it integrates clinical data with coding rules, enabling providers to detect and correct errors before claims submission, thereby minimizing revenue loss and administrative burden.
Why Should You Use Software to Identify Coding Errors?
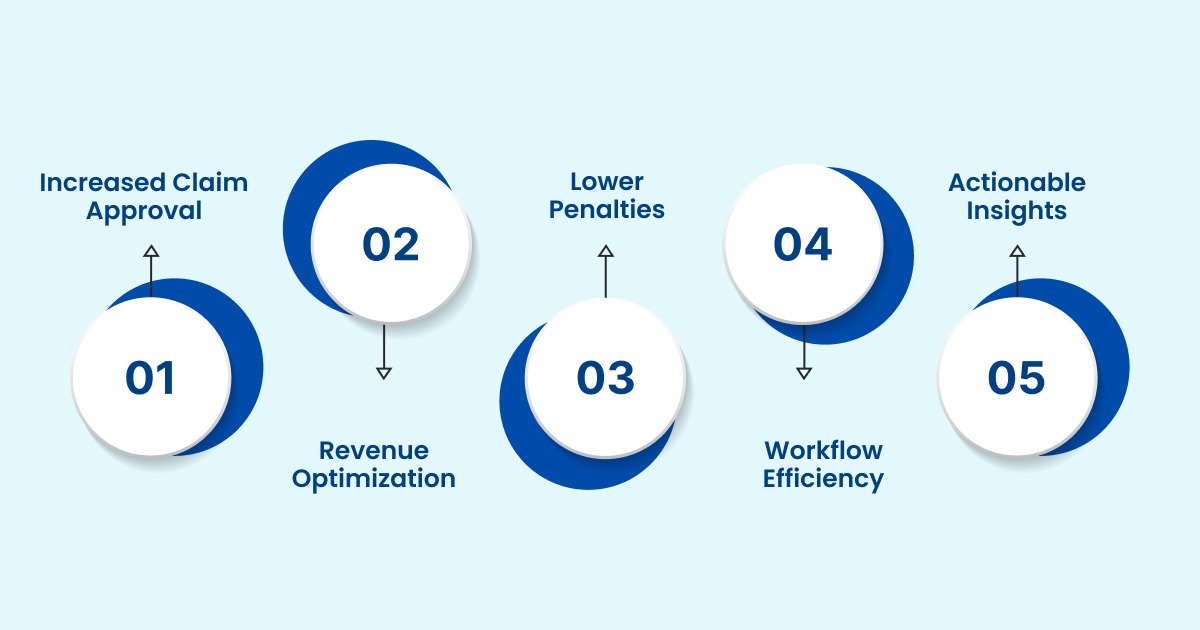
Implementing software used by hospitals to help identify CPT/HCPCS coding errors delivers both immediate and long-term advantages for revenue cycle management, compliance, and workflow efficiency:
- Higher First-Pass Claim Acceptance: Automatically detects and corrects coding errors before submission, significantly reducing payer rejections and speeding up reimbursement.
- Revenue Optimization: Ensures all billable services are accurately captured by aligning clinical documentation with proper CPT/HCPCS codes, maximizing hospital revenue.
- Reduced Compliance Penalties: Strengthens adherence to CMS, HIPAA, and payer-specific coding rules, lowering the risk of audit-triggered fines or regulatory penalties.
- Workflow Efficiency: Frees coders from repetitive manual checks, allowing them to focus on complex or high-risk cases, improving productivity and accuracy.
- Actionable Insights: Generates detailed analytics for CFOs, compliance officers, and revenue cycle managers to identify recurring errors by department, specialty, or individual coder.
With such key benefits, understanding the core features of this software clarifies how it prevents both financial losses and regulatory risks.
Essential Features of Medical Coding Software
Modern coding error detection software goes beyond a basic reference tool, serving as a complete system that enhances accuracy, enforces compliance, and streamlines coding workflows. Here’s a closer look at its core features:
1. Automated Code Validation
The software cross-checks CPT and HCPCS codes against constantly updated payer rules, NCCI edits, and LCD/NCD guidelines. This ensures every claim reflects current coding standards, reducing the risk of denials and underpayment. Coders no longer have to manually search rulebooks for each procedure, saving a significant amount of time.
2. Modifier Management
Many claim denials occur due to missing or incorrect modifiers like -25 (significant, separately identifiable service) or -59 (distinct procedural service). The software identifies such errors automatically, helping coders apply modifiers correctly and maximizing legitimate reimbursements.
3. Documentation-to-Code Matching
Using advanced natural language processing (NLP), the system analyzes physician notes and clinical documentation to verify that assigned codes match the documented services. This feature prevents discrepancies that could trigger audits or compliance issues.
4. Denial Prevention Rules Engine
By analyzing historical payer denial patterns, the software flags claims at risk of being rejected before submission. This proactive approach reduces repeated errors, accelerates reimbursement, and protects hospital revenue.
5. Audit Simulation Tools
Before claims are submitted, the system can perform “what-if” audits, simulating an honest payer review. It highlights high-risk claims, documentation gaps, and compliance vulnerabilities, enabling coders and compliance officers to correct issues early.
Additionally, advanced dashboards and real-time alerts provide actionable insights, helping coders and managers identify errors and optimize workflows. Coupled with seamless EHR/EMR integration and customizable reporting, these features ensure continuous compliance and improve coding accuracy.
Now, let’s explore how medical coding software automates code assignment, detects errors, and streamlines the claims process.
How Does Medical Coding Software Work?
Medical coding software automates the translation of clinical documentation into standardized CPT and HCPCS codes, ensuring accuracy, compliance, and faster claim submission. By combining rule-based logic, AI, and seamless EHR/EMR integration, it streamlines coding workflows and minimizes manual errors.
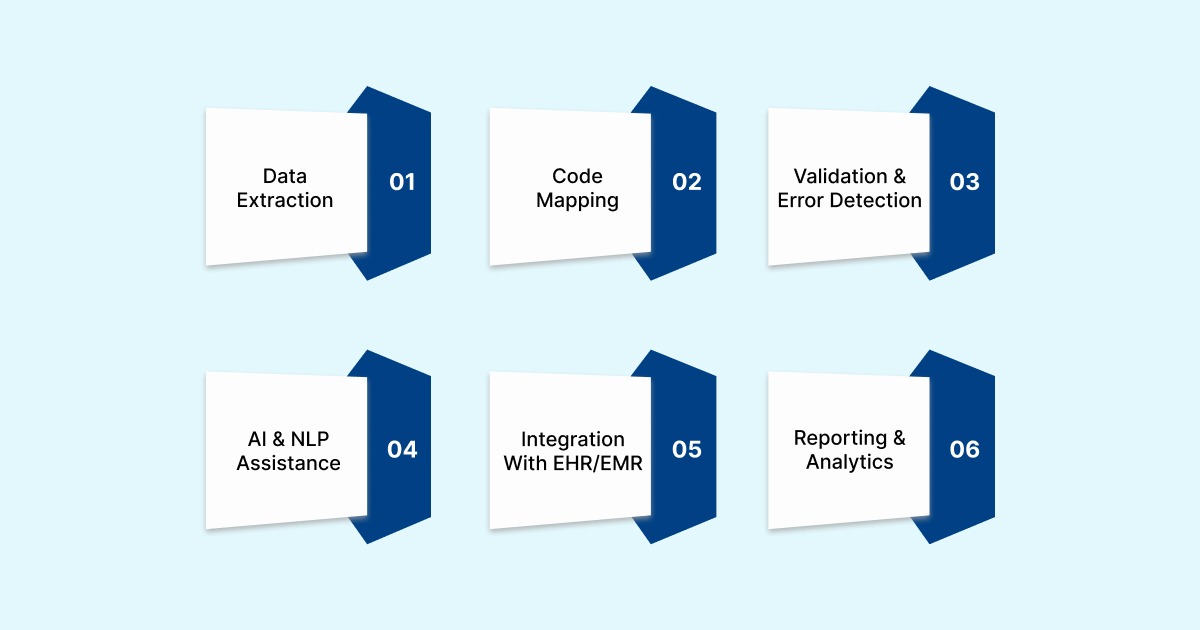
The process generally involves the following key steps:
1. Data Extraction: The software pulls relevant information from patient records, including diagnoses, procedures, and physician notes.
2. Code Mapping: Using built-in code libraries and payer-specific rules, the system assigns the correct CPT/HCPCS codes to each service.
3. Validation & Error Detection: Automated checks identify missing modifiers, inconsistent documentation, or rule violations to prevent claim denials.
4. AI & NLP Assistance: Advanced systems use natural language processing (NLP) to interpret unstructured clinical notes, ensuring codes accurately reflect patient care.
5. Integration with EHR/EMR: The software seamlessly integrates with existing hospital systems to provide real-time coding suggestions and minimize manual data entry.
6. Reporting & Analytics: Dashboards track coding accuracy, identify recurring errors, and provide insights for training, compliance, and revenue optimization.
By combining automation, AI, and real-time validation, medical coding software ensures hospitals and outpatient practices minimize errors, maximize reimbursements, and maintain compliance with ever-changing payer requirements.
While these features are powerful in theory, their true value becomes clear when examining the tangible benefits organizations achieve after implementing these systems.
Also Read: Differences and Basics of ICD-10 and CPT Codes
Top 5 Medical Coding Software for CPT/HCPCS Error Detection
Accurate CPT and HCPCS coding is essential for hospitals and outpatient practices to prevent claim denials, ensure compliance, and optimize revenue. Several advanced software solutions are now available that help coders identify and correct errors efficiently.
Below is an overview of the top five platforms widely used by healthcare organizations to detect and resolve coding errors:
1. RapidClaims

RapidClaims is an AI-powered medical coding and revenue cycle management platform that delivers end-to-end automation across coding, CDI, denial prevention, and recovery. It helps healthcare providers reduce administrative costs, minimize claim denials, capture more HCC/RAF codes, and accelerate reimbursements, supporting both Fee‑For‑Service (FFS) and Value-Based Care (VBC) models.
Key Features:
- RapidCode: Autonomous ICD-10, CPT, and E&M coding with 96%+ accuracy, processing over 1,000 charts/min, and achieving a 170% coder productivity lift. Few-shot deployment enables live implementation in under three weeks with as few as 500 historical charts.
- RapidCDI: Point-of-care HCC and quality gap detection, with inline RAF/MD prompts, longitudinal patient canvas, and V28-ready mapping, improving HCC capture by 24 % on average.
- RapidScrub: AI-driven denial prevention utilizing 119M smart edits, real-time eligibility & prior authorization checks, and multi-layer claim validation, resulting in a 40% reduction in denials.
- RapidRecovery: Success-based denial recovery with automated appeals, AI worklists, and managed services, delivering faster cash recovery with a 100 % contingency model.
- Explainable AI & Compliance – Full audit trail, line-level rationale, AHIMA/CMS-compliant templates, HIPAA, SOC 2, and ISO 27001-certified infrastructure.
- Seamless Integration: SMART-on-FHIR & HL7 support for Athena, Epic, Cerner, and eClinicalWorks.
Ideal For: Large healthcare organizations seeking scalable, end-to-end automation in coding, billing, and revenue cycle management.
2. 3M™ CodeFinder
3M™ CodeFinder is a computer-assisted coding (CAC) software that assists coders in generating accurate and complete ICD-10, CPT, and HCPCS codes using sophisticated decision logic.
Key Features:
- Guided Coding Pathways: Offers step-by-step guidance to coders, ensuring accurate code selection and implementation.
- Expert Decision Logic: Employs advanced algorithms to cross-reference medical records with the latest coding standards, reducing human error.
- Web-Based Deployment: Easily deployed as a web-based application, facilitating remote access and updates.
- Comprehensive Code Sets: Provides access to a wide range of code sets, including ICD-10-CM, CPT, and HCPCS Level II.
Ideal for: Hospitals and large practices that require sophisticated coding assistance and compliance support.
3. Optum Pro Encoder
Optum Pro Encoder is an online medical coding software that provides fast and detailed search capabilities for CPT, ICD-10-CM/PCS, and HCPCS Level II codes. The platform also offers lay descriptions for procedures and HCPCS, access to Coders’ Desk Reference descriptions, and automatic monthly updates to ensure coding accuracy and compliance.
Key Features:
- Extensive Code Lookup: Provides access to over 20 volumes of procedure, service/supply, and diagnosis reference material.
- Real-Time Updates: Offers complimentary code updates, ensuring coders have the most current information.
- User-Friendly Interface: Designed for quick and efficient code lookup, enhancing coder productivity.
Ideal for: Outpatient practices and billing teams that need quick and accurate code lookup.
4. Oracle Health EHR (formerly Cerner Ambulatory EHR)
Oracle Health EHR is a comprehensive electronic health record and revenue cycle management platform specifically designed for outpatient and ambulatory care settings. It combines medical coding, billing, practice management, and telehealth modules to improve clinical workflows and optimize financial performance.
Key Features:
- Integrated EHR and RCM: Combines clinical documentation with revenue cycle management to streamline operations and reduce administrative burden.
- Customizable Templates: Supports specialty-specific workflows with adaptable templates for efficient documentation.
- Voice Recognition: Enables accurate voice dictation and recognition to speed up documentation while maintaining compliance.
- Patient Portal: Provides patients with access to scheduling, test results, messaging, and telehealth appointments.
- Reporting & Analytics: Offers real-time dashboards and reporting tools to monitor coding accuracy, revenue performance, and operational efficiency.
Ideal For: Healthcare organizations and outpatient practices seeking an integrated EHR and RCM solution that enhances both clinical and administrative workflows.
5. Codify by AAPC
Codify by AAPC is a comprehensive online medical coding platform designed to streamline the coding process for healthcare professionals. It offers access to the latest CPT®, ICD-10-CM/PCS, and HCPCS Level II codes, along with coding guidelines and resources.
Key Features:
- Comprehensive Code Lookup: Provides access to a wide range of code sets, including CPT, ICD-10-CM/PCS, and HCPCS Level II.
- Coding Guidelines: Provides coding guidelines and resources to assist coders in selecting accurate codes.
- Regular Updates: Ensures that code sets and guidelines are regularly updated to reflect the latest standards.
- User-Friendly Interface: Designed for ease of use, facilitating quick and efficient code lookup.
Ideal For: Coders and healthcare professionals seeking a comprehensive coding reference tool.
With multiple solutions available, the real challenge lies in selecting the right fit for a hospital’s size, complexity, and compliance requirements.
Choosing the Right Medical Coding Software for Your Hospital
Selecting the right coding error detection software is a critical, multi-step process that impacts revenue, compliance, and operational efficiency. Key considerations include:
- EHR Compatibility: The software should integrate seamlessly with major EHR/EMR systems, such as Epic, Cerner, Meditech, or Allscripts, to minimize workflow disruptions.
- Volume Handling: It must scale effectively, from small outpatient clinics with low claim volumes to large tertiary hospitals processing thousands of claims daily.
- Payer-Specific Customization: The platform should support local payer edits in addition to CMS guidelines, ensuring accurate coding across all contracts.
- AI Maturity: Preference should be given to solutions that utilize advanced machine learning to predict and prevent claim denials proactively.
- Training & Adoption: Vendors that provide comprehensive coder training, ongoing compliance updates, and responsive support simplify implementation and improve adoption rates.
Choosing wisely is only half the battle; how hospitals implement and maintain these solutions determines their success.
Best Practices for Implementation and Ongoing Use
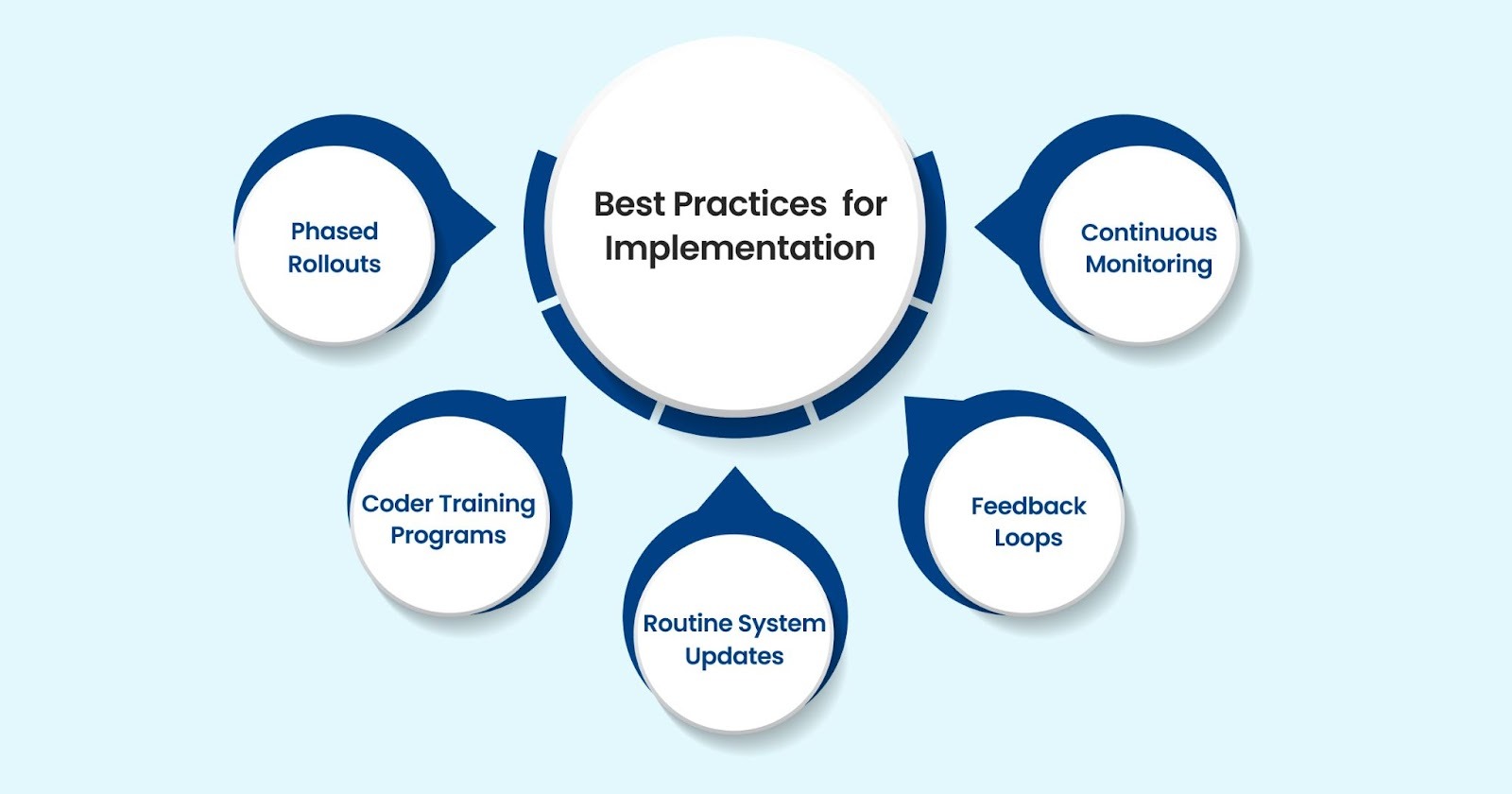
Effectively leveraging software used by hospitals to identify CPT/HCPCS coding errors requires a structured strategy that balances technology, training, and continuous oversight:
- Phased Rollouts: Implement the software in one department initially, such as outpatient surgery or cardiology, to evaluate workflow integration, identify challenges, and optimize configuration. Gradually expand hospital-wide to ensure seamless adoption and minimize disruption.
- Coder Training Programs: Beyond initial onboarding, provide ongoing training that combines software proficiency, updates on coding standards, and best practices for accurate documentation. Regular certification refreshers ensure coders remain compliant with evolving CPT, HCPCS, and ICD-10 rules.
- Routine System Updates: Ensure the software is updated consistently with the latest CPT, HCPCS, and ICD-10 code sets, payer-specific edits, and NCCI/NCD/LCD guidelines. Timely updates reduce errors and prevent denials due to outdated coding rules.
- Feedback Loops: Establish structured review cycles using denial reports, coding audits, and exception tracking to ensure effective feedback. Insights gained should guide workflow improvements, targeted coder coaching, and policy refinements to prevent repeat errors.
- Continuous Monitoring and Analytics: Utilize dashboards, AI analytics, and automated alerts to track coder performance, identify recurring error patterns, and detect systemic issues. This proactive approach enables early interventions, ensuring consistent coding accuracy across the organization.
By following these best practices, hospitals not only enhance current compliance and revenue protection but also build a foundation for scaling AI-driven coding automation and predictive analytics in the future.
To further streamline coding and ensure accuracy, platforms like RapidClaims can be integrated directly with EHR systems. Its RapidScrub module utilizes 119 million smart edits, refreshed daily from payer bulletins, and performs real-time eligibility and prior authorization checks. It also uses AI-powered multi-layer claim validation to reduce denials by up to 70%. By automating repetitive tasks, these solutions simplify claim submission and support faster, more reliable reimbursement.
Conclusion
Outpatient centers and private practices face the same coding risks as hospitals. Utilizing software used by hospitals to help identify CPT/HCPCS coding errors ensures mistakes are caught early, helping smaller practices safeguard revenue and maintain compliance.
Platforms like RapidClaims deliver AI-powered validation, payer-specific edits, and real-time error detection. Designed for both hospitals and outpatient practices, it reduces denials and accelerates reimbursements through seamless, cloud-native integration. Its analytics dashboards also give providers full visibility into recurring errors and financial performance.
Streamline your claims process and prevent costly coding mistakes with RapidClaims. Request a Free Demo today to see how your organization can achieve accurate, error-free coding with confidence.
Frequently Asked Questions (FAQs)
1. Can I automatically detect missing documentation in my patient records?
A. Yes. AI-powered coding software scans clinical notes, flags incomplete documentation, and prevents submission errors. This reduces denials and ensures compliance with CPT, HCPCS, and ICD-10 standards.
2. How can I customize coding rules for different payers or specialties?
A. Most platforms allow you to set payer-specific edits and specialty-based rules. This ensures your claims follow unique requirements, improving first-pass acceptance and minimizing manual corrections.
3. Is there a way I can monitor my coders’ performance and recurring errors?
A. Yes. Dashboards and analytics track coder activity, highlight frequent mistakes, and identify trends. Managers can use this data to provide targeted training and maintain coding accuracy.
4. Can I integrate this coding software with my existing EHR system?
A. Absolutely. Most solutions integrate seamlessly with major EHR platforms, enabling real-time coding suggestions within the clinical workflow. This improves efficiency and reduces duplicate work.
5. Will I be able to use this software in both small practices and large hospitals?
A. Yes. Coding software scales according to claim volume and complexity. Small outpatient practices gain efficiency, while large hospitals benefit from high-volume management and AI-driven analytics.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
Related Post
Top Products

%201.png)








