.webp)
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?

Accuracy and efficiency are critical to healthcare operations, yet medical billing remains one of the most complex and error-prone processes. Every claim, code, and compliance check affects both revenue and patient trust.
Manual billing systems, built on human coding and paperwork, struggle to meet the growing demand for speed and precision. Even small mistakes can lead to costly denials, delays, and compliance issues.
AI and Machine Learning are transforming this reality. These technologies streamline billing by automating coding, predicting claim outcomes, and minimizing human error. The World Health Organization highlights digital innovation as key to improving efficiency and equity in healthcare.
Researchers estimate that AI could save the healthcare industry between $200 billion and $360 billion annually in the U.S. through improved processes, reduced waste, and increased efficiency across multiple areas, including clinical operations, administrative tasks, and provider management.
It’s no longer just an administrative task; it’s evolving into a smart, data-driven system that powers faster payments, stronger compliance, and better patient outcomes.
Key Takeaways
- AI is redefining billing accuracy, minimizing human errors through automated coding and claim validation.
- Machine Learning boosts financial outcomes, cutting denial rates and improving reimbursement timelines.
- AI strengthens revenue protection, detecting fraud and compliance risks in real time.
- Predictive analytics turn billing teams into proactive decision-makers, improving forecasting and revenue stability.
- Automation is delivering tangible impact, including 15,000 labor hours saved per month in real RPA deployments.
- RapidClaims turns billing teams into high-performance, data-driven units, ensuring accurate coding, compliance, and maximum ROI.
- The future is AI-driven, with the medical billing AI market soaring toward $36.37B by 2034.
Table of Contents
- Essential AI Technologies Powering Modern Medical Billing
- Key Applications of AI in Medical Billing
- The Role of Machine Learning Models
- Use Cases of AI and Machine Learning in Medical Billing
- Challenges and Considerations in Implementing AI in Medical Billing
- Key Tools and Technologies Leading the Change
- Transform Medical Billing with RapidClaims AI
- Conclusion
- FAQ
Essential AI Technologies Powering Modern Medical Billing
AI is reshaping medical billing by automating complex workflows, improving coding accuracy, preventing claim denials, and enhancing revenue outcomes.
- Machine learning models are improving claim accuracy and reducing denials: A research paper deploying ML methods reported a 25% reduction in claim denial rates over a 6-month period when using a machine-learning flagged intervention compared to a control.
- NLP-driven coding intelligence converts unstructured clinical text into structured billable data, notably improving accuracy and reducing manual workload.
- Robotic Process Automation (RPA) is automating repetitive billing tasks like eligibility checks and payment posting; as reported, one revenue-cycle firm saved 15,000 employee hours per month thanks to automation.
- Predictive analytics and fraud detection tools help providers forecast denial trends, identify billing anomalies (e.g., upcoding/unbundling) and reduce revenue leakage, healthcare organizations are losing 15–30% of potential revenue through RCM inefficiencies.
- The AI in the medical billing market is growing rapidly: the global market was projected at USD 3.73 billion in 2024 and expected to reach USD 36.37 billion by 2034 (CAGR ~25.4%).
Key Applications of AI in Medical Billing
AI is fundamentally reshaping how healthcare organizations manage billing and revenue operations. From automating manual tasks to enabling predictive financial insights, AI is transforming the entire billing ecosystem into a smarter, faster, and more transparent process.
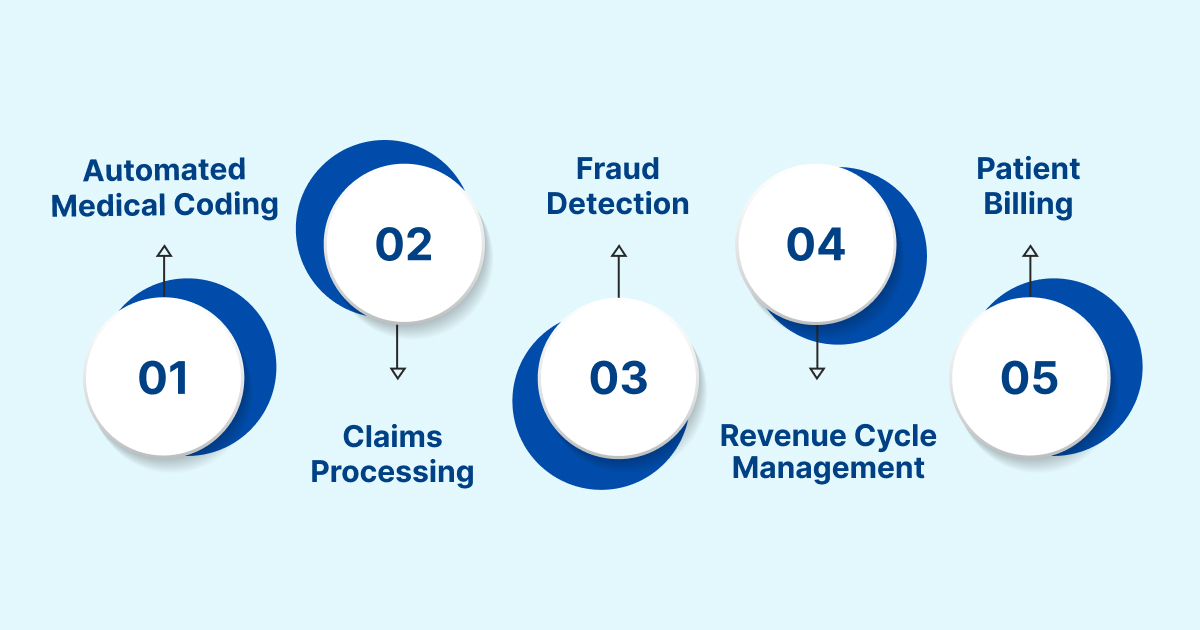
Automated Medical Coding
AI-powered Natural Language Processing (NLP) is transforming how clinical data is interpreted and converted into billing codes.
- NLP scans and understands clinical notes, reports, and discharge summaries, identifying key terms for accurate code assignment.
- It automatically generates ICD-10 and CPT codes, minimizing human error and improving speed.
- This automation ensures coding uniformity and compliance, reducing audit risks and claim rejections.
Manual coding doesn’t have to be the bottleneck anymore. With RapidCode, an autonomous AI-powered coding engine, healthcare providers can process charts in seconds with consistent accuracy and full compliance.
Claims Processing and Error Detection
AI brings precision and foresight to claims management by predicting and preventing errors before submission.
- Machine learning models analyze historical claim data to identify patterns that often result in denials or delays.
- Intelligent claim scrubbing tools detect missing or mismatched data, ensuring cleaner claims.
- Predictive models continuously refine their accuracy, leading to faster reimbursements and fewer reworks.
Fraud Detection and Compliance
AI strengthens the integrity of billing operations by ensuring fraud prevention and regulatory adherence.
- Advanced algorithms monitor vast datasets to detect irregular billing patterns or duplicate entries in real time.
- Machine learning learns from past fraud attempts, enhancing its ability to spot anomalies before they cause losses.
- AI systems ensure compliance with HIPAA, CMS, and payer regulations, reducing financial and legal risks.
Revenue Cycle Management (RCM)
AI optimizes the entire revenue cycle, from pre-authorization to payment posting, by combining automation with predictive insights.
- Predictive analytics forecast cash flow, denial probabilities, and payment cycles, helping organizations plan more effectively.
- AI automates routine follow-ups, identifies high-value claims, and prioritizes resource allocation for efficiency.
- This leads to improved collection rates, reduced overhead, and better financial stability.
Patient Billing and Cost Estimation
AI is redefining the patient billing experience, offering transparency, personalization, and real-time support.
- Chatbots and virtual assistants manage billing queries, insurance checks, and payment reminders instantly.
- Machine learning models generate customized cost estimates before procedures, reducing confusion and disputes.
- Patients gain greater visibility into their billing process, improving satisfaction and timely payments.
Struggling with incomplete or inaccurate documentation affecting reimbursements? RapidCDI turns clinical notes into precise risk scores at the point of care. It improves RAF accuracy by 25%, saves physicians 30 minutes per day, boosts quality measures by 15%, and generates $2.2M in value through automated coding.
The Role of Machine Learning Models
ML forms the foundation of AI-driven medical billing systems. These models continuously learn from data, adapt to new regulations, and refine prediction, making them more accurate and efficient over time.
Training on Historical Claim Data
ML models are trained on large volumes of past billing and claim data to understand real-world patterns and outcomes.
- They analyze thousands of historical claims, identifying trends in approvals, rejections, and coding variations.
- The models learn which factors lead to denials or delayed payments and use that insight to predict and prevent future issues.
- Over time, they build a knowledge base that mirrors the organization’s unique billing and payer environment.
Continuous Learning Through Feedback Loops
Unlike static software, ML models evolve through constant feedback and real-world performance monitoring.
- Each new claim submission and its outcome act as feedback data to fine-tune algorithms.
- The system automatically adjusts to billing patterns, payer responses, and compliance changes.
- This self-improving loop ensures models stay relevant and accurate, even as workloads increase.
Adaptive Systems That Evolve with Regulations
Regulatory frameworks and coding systems in healthcare are dynamic, ML helps organizations keep pace effortlessly.
- Models adapt to updates in ICD-10, CPT, and payer-specific billing rules without manual reprogramming.
- AI engines can auto-refresh their databases when new codes or compliance policies are introduced.
- This adaptability minimizes compliance risks and ensures long-term sustainability of billing systems.
Unlike static software, RapidClaims’ AI learns from every chart, denial, and payer update, becoming more accurate over time. Its self-optimizing models ensure compliance with changing ICD-10 and CMS rules automatically.
Also Read: From Chaos to Clarity: How AI in Medical Coding Enhances Accuracy
Use Cases of AI and Machine Learning in Medical Billing
AI and Machine Learning are redefining how healthcare organizations manage billing operations. These technologies are improving accuracy, reducing costs, and creating smarter, data-driven systems that adapt to ever-changing regulatory and operational demands.

- Automated Medical Coding
AI-powered Natural Language Processing scans and interprets physician notes, clinical reports, and discharge summaries to assign accurate ICD-10 and CPT codes. This automation minimizes manual effort, eliminates common coding errors, and ensures greater speed and compliance across departments.
- Predictive Claim Management
Machine Learning models analyze historical claim data to predict potential denials and delays. By identifying risks early, billing teams can correct discrepancies before submission, resulting in faster reimbursements, fewer resubmissions, and better cash flow management.
- Fraud Detection and Prevention
AI continuously monitors billing data to detect unusual patterns, duplicate entries, or irregular claim behavior. These systems safeguard healthcare providers by identifying fraud indicators in real time and helping maintain financial integrity and trustworthiness.
- Revenue Forecasting and Optimization
Predictive analytics powered by AI provide insights into expected reimbursements, denial trends, and payment cycles. Healthcare leaders use these forecasts to plan budgets, allocate resources efficiently, and improve overall revenue predictability.
- Automated Compliance Monitoring
AI tools automatically check every claim against HIPAA, CMS, and payer-specific rules. They stay updated with regulatory changes, reducing audit risks and ensuring billing teams maintain consistent adherence to evolving compliance standards.
- Error Detection and Quality Control
AI validates claim data before submission, detecting incomplete information, mismatched codes, and other discrepancies. This ensures cleaner claims, fewer rejections, and improved accuracy across the billing workflow.
- Patient Billing Transparency
Machine Learning enables personalized billing communication and cost estimation. Patients can access clear, real-time information about payments and coverage, improving satisfaction and promoting timely payments.
- Operational Efficiency and Workforce Support
AI automates repetitive billing processes such as data entry, claim scrubbing, and follow-ups. This not only reduces administrative overhead but also allows billing professionals to focus on higher-value tasks like compliance auditing and revenue analysis.
These advancements show the value AI brings to billing operations, but turning potential into practice requires navigating several real-world challenges.
Challenges and Considerations in Implementing AI in Medical Billing
AI and ML are transforming medical billing, but implementation isn’t without obstacles. Healthcare organizations must balance innovation with compliance, security, and operational readiness to fully realize the benefits of intelligent automation.
- Data Privacy and Security: Protecting sensitive patient and financial data remains a top priority. AI systems must comply with HIPAA and other privacy laws while safeguarding against breaches and cyberattacks.
- Integration with Legacy Systems: Many healthcare organizations still rely on outdated billing platforms that aren’t compatible with AI applications. Seamless integration is essential to avoid data silos and workflow disruptions.
- High Implementation and Maintenance Costs: Deploying AI tools requires significant investment in technology, skilled personnel, and continuous maintenance. The return on investment grows over time but may strain smaller providers initially.
- Data Quality and Availability: AI models depend on large volumes of clean, accurate data to perform effectively. Incomplete or inconsistent records can reduce prediction accuracy and increase system bias.
- Workforce Training and Adaptation: AI adoption demands upskilling teams to interpret insights, manage exceptions, and maintain compliance. Human expertise remains vital for oversight and ethical use.
- Ethical and Transparency Concerns: Ensuring AI systems are explainable and fair is crucial for trust and accountability. Decisions must be auditable, especially when tied to claim approvals or denials.
- Evolving Regulatory Environment: Healthcare AI adoption is still guided by emerging laws and standards. Organizations must stay agile to adapt to new compliance frameworks and ethical AI guidelines.

Also read: AI-Powered Automation in Medical Coding
Key Tools and Technologies Leading the Change
The evolution of AI and Machine Learning in medical billing is powered by a new generation of intelligent technologies. From automated billing platforms to integrated EHR systems, these tools are redefining how healthcare organizations manage financial operations with greater precision and efficiency.
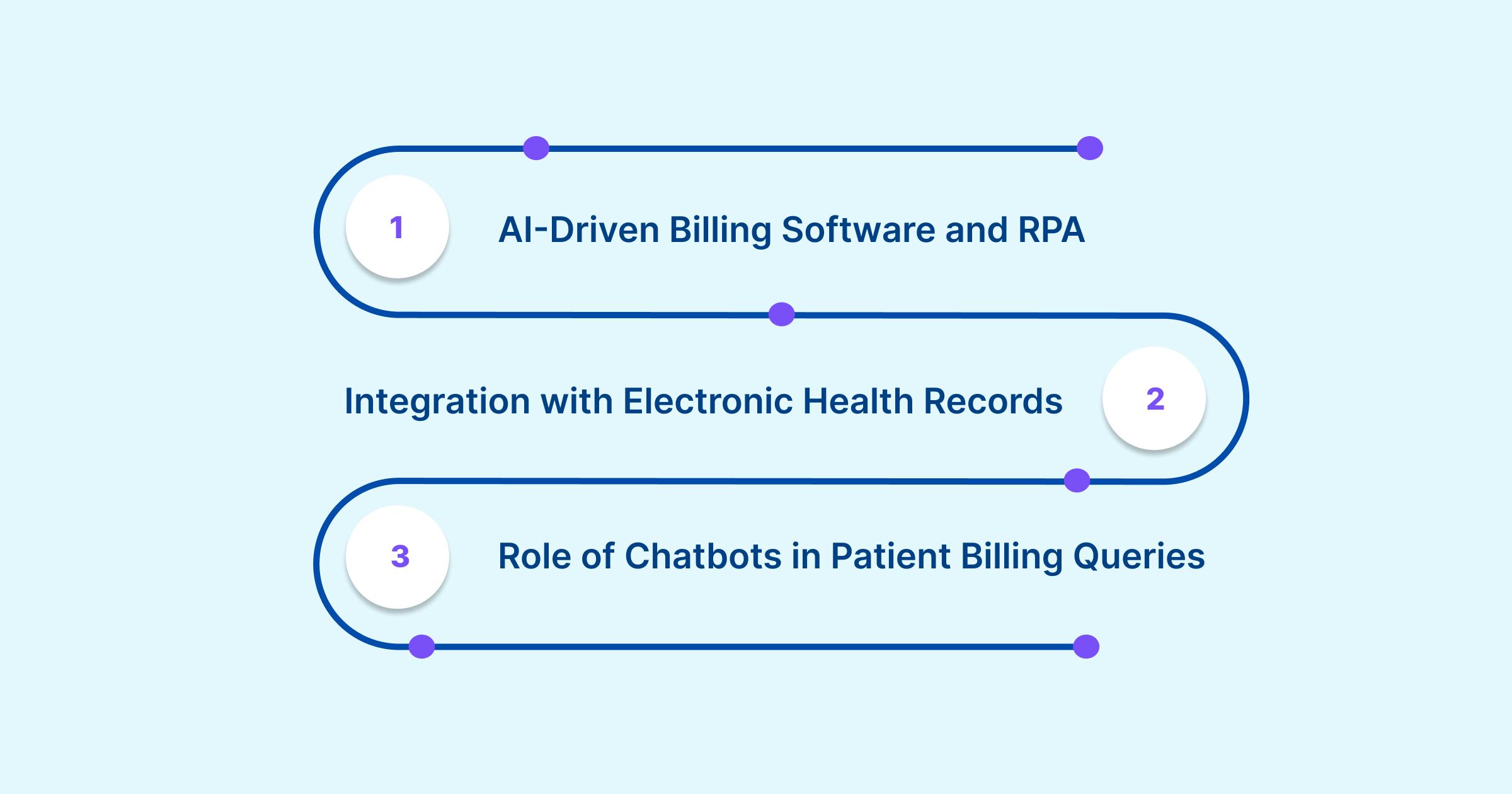
AI-Driven Billing Software and RPA (Robotic Process Automation)
AI and Robotic Process Automation (RPA) work together to streamline complex billing workflows and reduce human effort.
- AI algorithms automate coding, claims validation, and payment posting with near-zero error rates.
- RPA bots execute repetitive tasks, like data extraction, claim filing, and payer follow-ups, 24/7 without fatigue.
- Combined, they significantly enhance accuracy, speed, and cost savings.
Integration with Electronic Health Records (EHRs)
AI-driven billing tools now seamlessly connect with Electronic Health Record (EHR) systems to ensure real-time, accurate data exchange.
- This integration eliminates data silos between clinical and billing departments.
- Billing systems can automatically pull diagnosis codes, treatment details, and patient demographics directly from EHRs.
- Enhances claim accuracy and minimizes documentation errors that lead to denials.
Role of Chatbots in Patient Billing Queries and Payment Reminders
AI-powered chatbots and virtual assistants are transforming patient engagement in billing and payment processes.
- They handle common queries such as insurance coverage, balance inquiries, and due dates.
- Chatbots send automated payment reminders and enable secure online payment links.
- This reduces call center loads while improving patient satisfaction and on-time payments.
Transform Medical Billing with RapidClaims AI
As healthcare organizations continue to embrace AI and Machine Learning, success will depend on using technology that not only accelerates coding but understands it. That’s exactly what RapidClaims delivers.
- AI-Powered Accuracy: Automate medical coding with RapidCode, an autonomous engine capable of coding thousands of charts per minute with near-perfect precision.
- Predictive Error Prevention: Use RapidScrub to detect documentation gaps, incorrect mappings, and payer rule mismatches before claims are submitted.
- Smarter Human-AI Collaboration: Empower coders with RapidCDI, an AI partner that recommends accurate codes, flags missing data, and accelerates claim validation.
- Optimized Reimbursements: Improve risk-adjusted coding accuracy, ensuring fair compensation and compliance with HCC, ICD-10, and CMS guidelines.
- End-to-End Compliance & Transparency: Every claim is traceable, auditable, and aligned with the latest payer regulations, eliminating costly rework and audit risks.
With RapidClaims, healthcare billing transforms from a manual, error-prone process into a high-velocity, insight-driven revenue engine.
Conclusion
AI and Machine Learning are significantly enhancing medical billing. Automation, advanced analytics, and real-time fraud detection are streamlining billing operations to be more efficient, clear, and reliable.
Innovate with RapidClaims:
- Automating complex workflows with AI-powered claim management
- Ensuring clean claims, faster reimbursements, and zero data silos
- Offering real-time analytics for smarter revenue cycle management
Streamline your billing with AI. Book a demo with RapidClaims to experience how intelligent automation can reshape your medical billing process.
FAQ
1. How does Machine Learning improve billing accuracy?
ML continuously learns from historical billing data to identify trends that lead to claim denials or delays. It uses this insight to predict potential errors before submission, ensuring cleaner claims and higher reimbursement rates over time.
2. Can AI completely replace human billers?
No. AI complements rather than replaces human expertise. While AI automates repetitive tasks like data entry and claim scrubbing, human professionals still provide oversight, handle exceptions, and ensure ethical and compliant billing practices.
3. How does AI detect and prevent billing fraud?
AI algorithms analyze vast datasets to detect irregular billing patterns, duplicate entries, or anomalies that could signal fraud. These systems continuously learn from new cases, improving detection accuracy and safeguarding healthcare revenue.
4. Is AI billing compliant with healthcare regulations?
Yes. AI billing systems are designed to comply with HIPAA, CMS, and other regulations. They maintain secure data encryption and automatically update to meet changing coding standards, reducing audit risks and legal exposure.
5. What is Natural Language Processing (NLP) in medical billing?
NLP allows AI systems to read and interpret doctors’ notes, clinical reports, and discharge summaries. It automatically assigns accurate ICD-10 and CPT codes, minimizing human intervention while maintaining high precision.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
What Is An Additional Diagnosis In Medical Coding And Why It Matters For Reimbursement?
Top Products

%201.png)








