.webp)
EMR Conversion Challenges & Best Practices in 2026

Healthcare organizations across the U.S. are accelerating EMR conversion projects in 2026. Mergers, regulatory changes, interoperability demands, and the push for data-driven care are forcing many providers to replace or consolidate legacy systems faster than planned.
But EMR conversion is no longer just an IT upgrade.
When done poorly, it can disrupt clinical workflows, overwhelm physicians, delay claims, and create revenue leakage that lasts months after go-live. Many organizations discover too late that data migrated "successfully" does not always mean data that is usable, accurate, or compliant in real-world workflows.
This is why electronic medical record conversion has become one of the highest-risk operational initiatives for healthcare leaders today.
The good news is that most EMR conversion challenges are predictable. Downtime, documentation gaps, coding errors, and denial spikes tend to follow familiar patterns when planning and execution fall short. With the right preparation and modern best practices, organizations can reduce these risks and stabilize both patient care and revenue much faster.
This guide cuts through generic advice and focuses on the real challenges providers face during EMR conversion in 2026, backed by practical best practices that help protect patient care and financial stability.
Key Takeaways
- EMR conversion fails after go-live, not during implementation. Documentation, coding, and billing issues surface when workflows change, and performance isn't monitored early.
- "Data migrated" does not mean "data usable." If clinical data isn't accessible, structured, and consistent, it directly increases coding errors and denials.
- Revenue risk rises fast during EMR transitions. Even small documentation or coding shifts can spike denials and delay cash flow within the first 60–90 days.
- Speed to stability matters more than speed to go-live. Organizations that baseline performance and maintain governance recover faster and avoid long-term disruption.
- AI-driven validation reduces post-conversion risk. Solutions like RapidClaims help protect documentation quality, coding accuracy, and claim performance as EMR workflows change.
Table of Contents:
- What Is EMR Conversion and Why It's No Longer a Simple IT Project
- 5 Biggest EMR Conversion Challenges Healthcare Organizations Face
- Why Traditional EMR Conversion Approaches Fail in 2026
- EMR Conversion Best Practices for Healthcare Organizations in 2026
- How Healthcare Leaders Can Reduce EMR Conversion Risk
- Conclusion
- FAQs
What Is EMR Conversion and Why It's No Longer a Simple IT Project
In theory, electronic medical record conversion, moving patient charts and administrative data from one system to another, sounds like a technical chore for the IT department. In practice, it's one of the most complex operational projects a healthcare organization can undertake.
That's because EMR conversion isn't just about shifting bits of data. It involves reshaping how clinical teams work, how revenue gets captured, and how patients experience care continuity.
At its core, EMR conversion encompasses three major components:
- Data migration: extracting, transforming, and loading legacy clinical and billing records into a new system
- Workflow alignment: redesigning daily operations to fit the new platform
- User adoption: training and support so clinicians, coders, and administrators can use the system effectively
But unlike a typical software upgrade, EMR conversion touches every function in a healthcare organization. For example:
- Clinical data integrity matters for patient safety. Missing or corrupted notes can lead to misdiagnoses or incomplete care decisions. Even minor migration gaps can compromise the continuity of care across encounters.
- Billing and coding accuracy directly impacts revenue. If data fields (diagnoses, procedures, charge details) aren't mapped correctly, downstream systems may reject claims or generate denials.
- Clinician workflows change overnight. A new interface or documentation process can slow charting and increase clinician burden unless thoughtfully optimized.
These realities mean EMR conversion cannot remain an isolated IT project. Instead, it must be treated as an enterprise transformation initiative. One that integrates technology, clinical workflow redesign, revenue cycle management, and compliance strategies under a coordinated plan.
EMR conversion in 2026 is no longer just an IT migration. It's a strategic initiative with clinical, operational, and financial consequences.
5 Biggest EMR Conversion Challenges Healthcare Organizations Face
The hardest parts of EMR conversion aren't the system install or the data extract. They're the second-order effects that show up after go-live: clinicians slow down, documentation quality drifts, coding gets inconsistent, and denials rise because "the same work" is suddenly produced in a different format.

Here are the challenges that most often cause real operational damage, plus how they show up, what to watch for, and why they matter.
1) Data Migration Gaps That Break Clinical Context
Most EMR conversions don't “lose all the data." They lose the correct data in ways that don't become obvious until a clinician is mid-visit or a claim is being appealed.
Where it breaks in the real world:
- Problem lists get duplicated, outdated, or deprioritized
- Medication histories lose sig details or stop dates
- Scanned documents and attachments migrate, but become hard to find
- Free-text notes move, but lose structured tags that downstream tools rely on
Why this is bigger than inconvenience: chart errors are common even without a conversion. One 2024 analysis of EHR documentation errors found 15% of reviewed charts contained documentation errors in a specialty setting. Now layer a conversion on top, and the risk to data integrity rises fast.
What to monitor during conversion validation (high-yield checks):
- Medication list accuracy (active meds + allergies)
- Active problem list accuracy (not just "present" but correct)
- Presence and retrievability of scanned clinical documents
- Completeness of prior notes for high-risk cohorts (CHF, CKD, diabetes, oncology)
2) The Post–Go-Live "Usability Dip" That Slows Clinicians Down
Even when training is intense, a new EMR changes cognitive flow. That shift shows up as slower documentation, more clicks, and more after-hours work.
This isn't anecdotal. A 2024 study in JAMIA Open examining clinician experience during an EHR transition found that EHR usability scores declined after the transition, with declines evident 2 months post-go-live. The study tracked how these patterns persisted over time.
And the burden is already heavy before any conversion. How this hits the business:
- Visits run long → fewer appointments per day
- Notes close later → coding queues grow
- Clinical Documentation Improvement (CDI) queries rise → physician annoyance spikes
Go-live warning signs to call out early:
- Note closure delays (same-day close rate dropping)
- Inbox volume spikes, especially for refill and portal messages
- Increased "pajama time" (after-hours EHR work)
3) Revenue Cycle Disruption That Starts Quietly, Then Snowballs
EMR conversion often creates revenue risk in a subtle sequence:
- Templates change → documentation gets less specific
- Coding gets conservative or inconsistent
- Claims go out "technically complete," but weaker
- Denials rise because payers request documentation or flag inconsistencies
In 2024, Optum's Denials Index reported national denial rates around 12% based on analysis at scale, illustrating how little room providers already have for additional denial pressure.
HFMA materials (2024) also highlight how common initial denials are in commercial reimbursement: nearly 15% of medical claims submitted to private payers are initially denied.
Why this matters specifically during EMR conversion:
- If your baseline is already near 10–15% in some lines of business, even a small conversion-driven bump creates significant rework and cash drag.
What to track daily for the first 60–90 days:
- First-pass resolution / clean claim rate (by payer)
- Denials by reason category (medical necessity, auth, coding edits, demographics)
- Days in A/R trendline (not just monthly averages)
- Charge lag and claim lag (time from encounter → bill drop)
4) Interoperability and Mapping Issues That Break Downstream Systems
In 2026, EMR conversion usually isn't "one system to one system." It's EMR + clearinghouse + labs + imaging + registries + payer connections.
Modern integration increasingly relies on standards such as HL7 and FHIR, but real-world systems aren't consistent in how they encode and structure data.
Academic work in 2024–2025 continues to highlight the complexity of harmonizing heterogeneous EHR data and transforming formats (e.g., CDA to FHIR), especially when local configuration varies by site.
What this looks like operationally:
- Eligibility or authorization checks fail intermittently
- Orders route incorrectly (labs/imaging)
- Clearinghouse edits behave differently post-migration
Practical prevention move: Validate end-to-end transactions, not just data fields (encounter → claim → remit)
5) Governance & Support Gaps That Turn Issues Into "The New Normal.”
The conversion doesn't end at go-live. It ends when performance stabilizes.
A major reason organizations struggle: they lack a clear stabilization governance model (who owns what, how issues are prioritized, what "fixed" means).
One of the clearest public-sector signals of how governance and issue resolution can derail EHR modernization is the U.S. GAO's 2025 reporting on VA EHR modernization, which includes structured feedback showing significant user dissatisfaction with problem resolution and the ability to perform duties.
What strong governance looks like in practice:
- A cross-functional "conversion command center" (clinical + IT + HIM + RCM)
- Weekly stabilization sprints for the first 6–10 weeks (then monthly). Implementation reviews often recommend continued optimization beyond go-live.)

Why Traditional EMR Conversion Approaches Fail in 2026
Most EMR conversion projects fail for the same reason: they're still executed as technical migrations instead of operational transformations. In 2026, that gap matters more than ever.
- Traditional EMR conversion plans focus on hitting a go-live date. But real risk appears after launch, when clinical workflows, documentation patterns, and billing behavior shift simultaneously.
- Most conversions still depend on classroom training and tip sheets. That approach doesn't hold up under real-world clinical pressure.
- Legacy approaches assume that if data migrates successfully, the job is done. In reality, data must be easy to find during an encounter and structured for coding and CDI.
- Payer rules, edits, and documentation expectations are changing faster than ever. Static rules-based checks that worked before conversion often fail once templates and workflows change.
- Finally, many organizations dissolve their conversion command structure too soon. Without ongoing cross-functional ownership, workarounds harden into long-term workflow debt.
This is precisely why modern EMR conversion best practices focus on continuous validation, workflow support, and early revenue protection, not just data migration.
Traditional EMR conversion plans focus on system readiness. RapidClaims focuses on performance readiness.
- RapidCode validates coding accuracy as documentation patterns change
- RapidCDI supports clinicians with real-time documentation guidance
- RapidScrub adapts to payer edits that often spike after conversion
Together, they help organizations stabilize faster after go-live.
See how RapidClaims supports EMR transitions beyond the go-live checklist. Request an overview.
EMR Conversion Best Practices for Healthcare Organizations in 2026
In 2026, successful EMR conversion is less about flawless execution on day one and more about how quickly organizations detect, correct, and adapt when workflows shift. The best-performing organizations plan for disruption and engineer guardrails around it.
Here's what that looks like in practice.
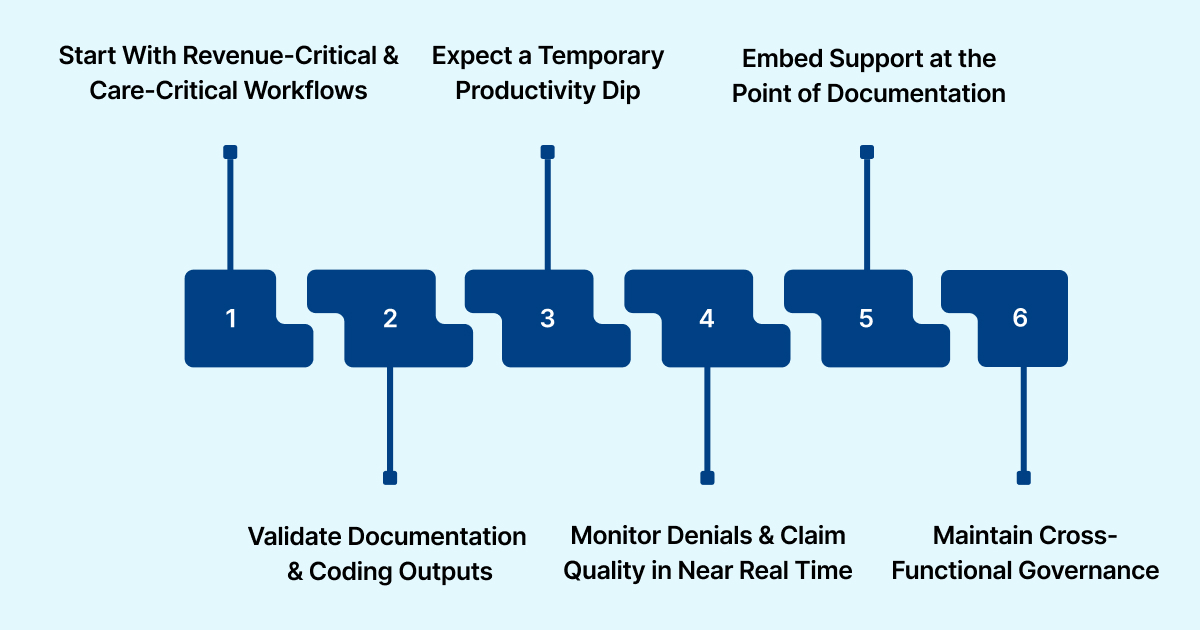
1. Start With Revenue-Critical & Care-Critical Workflows
High-performing organizations don't begin EMR conversion by asking, "What features does the new system have?" They start by identifying which workflows cannot afford to break.
That typically includes:
- High-volume outpatient visits
- Specialty encounters tied to complex coding (cardiology, nephrology, oncology)
- Prior authorization and charge capture workflows
Even short disruptions to charge capture and authorization workflows can materially impact cash flow in the first 60 days post-conversion.
Best practice: Rank workflows by financial and clinical risk, then design the conversion plan around those priorities.
2. Validate Documentation & Coding Outputs
One of the most common EMR conversion mistakes is validating data at rest rather than in use.
In other words:
- It's not enough that a diagnosis exists in the chart.
- It has to surface correctly in clinician workflows and downstream coding processes.
Documentation completeness and specificity vary widely depending on template design and workflow configuration. During EMR conversion, even small template changes can reduce diagnostic specificity, directly affecting medical coding accuracy.
Best practice: Before full go-live, test real encounters end-to-end: Document → code → bill → payer response. This catches issues that field-level checks never reveal.
3. Expect a Temporary Productivity Dip & Plan for It Explicitly
Even well-run EMR conversions cause short-term productivity loss. What separates successful organizations is whether that dip is planned and buffered or ignored.
Peer-reviewed studies and extensive health-system reports consistently show:
- Reduced clinician throughput immediately after go-live
- Increased documentation time per encounter
- Slower note closure for several weeks
Organizations that planned staffing buffers, adjusted visit volumes, or extended stabilization support recovered faster and avoided prolonged backlogs.
Best practice: Treat the first 30–90 days as a controlled recovery phase, not a return to business as usual.
4. Monitor Denials & Claim Quality in Near Real Time
Denial spikes rarely happen because "the EMR failed." They occur because documentation patterns change faster than revenue-cycle controls.
During EMR conversion, even minor documentation or coding inconsistencies can push baseline denial rates higher if not detected early.
What leading organizations monitor daily after go-live:
- Clean claim rate by payer
- Claim denials by category (medical necessity, auth, coding)
- Charge lag and claim lag
Best practice: Use early payer feedback as a diagnostic signal, not a lagging KPI.
5. Embed Support at the Point of Documentation
Post-conversion clean-up is expensive and frustrating. The most effective organizations reduce rework by supporting clinicians as documentation occurs, not by querying days later.
- High levels of physician administrative burden are tied to EHR use. During EMR conversion, that burden increases unless documentation workflows are actively optimized.
Best practice: Prioritize real-time guidance, template refinement, and workflow coaching over retrospective corrections.
6. Keep Cross-Functional Governance Until Performance Stabilizes
Many EMR conversions technically succeed but operationally stall because governance ends too early. Unresolved workflow issues persist when ownership dissolves after go-live.
Strong programs maintain:
- Joint clinical, IT, HIM, and RCM ownership
- Clear success metrics (note closure time, coding turnaround, denial mix)
- Regular optimization cycles until performance returns to baseline
Best practice: Define stabilization success metrics up front and maintain governance until they are met.
These practices focus on speed-to-stability rather than speed-to-go-live.
How Healthcare Leaders Can Reduce EMR Conversion Risk
In 2026, the biggest EMR conversion failures don't happen because the technology breaks. They occur because leadership doesn't see risk early enough or respond fast enough when workflows shift.
Here's how healthcare organizations can manage EMR conversion as a risk-management exercise rather than an implementation task:
- First, instead of measuring progress by whether the system went live, focus on whether clinical and revenue performance remain intact. That means tracking indicators such as note closure time, coding turnaround, clean-claim rates, and denial mix immediately after go-live.
- Second, establish a performance baseline before conversion. Without knowing pre-conversion norms, it's impossible to tell whether post-go-live issues are caused by the EMR transition or by unrelated payer or staffing changes.
- Third, keep clinical voices involved during stabilization. When leadership responds quickly to documentation friction and usability concerns, both clinician efficiency and documentation quality recover faster.
- Finally, governance stays in place longer than feels comfortable. Maintain cross-functional ownership until performance metrics normalize, and avoid turning temporary workarounds into permanent operational debt.
Healthcare leaders can reduce EMR conversion risk by focusing less on implementation milestones and more on early performance signals, clinician experience, and sustained accountability.
When those elements are managed tightly, conversion disruption remains temporary rather than becoming the new normal.
Conclusion
In 2026, EMR conversion is no longer just about moving from one system to another. It's about preserving the integrity of the encounter-to-claim lifecycle while clinical workflows, documentation patterns, and revenue processes are in flux.
Healthcare organizations that treat EMR conversion as an operational risk to be actively managed, not a technical milestone to be completed, are better positioned to protect clinicians from unnecessary burden and prevent temporary disruption from becoming long-term revenue leakage.
If your organization is evaluating how to strengthen documentation quality, coding accuracy, and claim performance before or after EMR conversion, a focused automation approach can make the difference.
Request a personalized demo with RapidClaims to see how AI can support your RCM team across coding, CDI, and denial prevention. This will help you stabilize faster and operate with confidence in 2026.
FAQs
Q. How long does an EMR conversion realistically take for mid- to large-sized practices?
A. While technical migration may take a few months, complete operational stabilization often takes 3–6 months. The timeline depends less on data volume and more on workflow complexity, specialty mix, and how quickly documentation and billing processes normalize after go-live.
Q. What data should not be migrated during an EMR conversion?
A. Not all legacy data adds value. Organizations often exclude outdated problem lists, inactive medications, and low-value scanned documents. Migrating excessive or irrelevant data can clutter clinician workflows and increase documentation and coding errors post-conversion.
Q. Can EMR conversion affect value-based care performance and risk adjustment?
A. Yes. Changes in documentation templates and problem list behavior can impact HCC capture, RAF scores, and quality reporting. Without safeguards, even short-term documentation gaps during conversion can lead to measurable revenue and performance losses in value-based contracts.
Q. What are the most overlooked costs of EMR conversion?
A. Beyond vendor and implementation fees, hidden costs include productivity loss, increased denial rework, temporary staffing needs, and delayed cash flow. These indirect costs often exceed direct IT expenses if conversion risk isn't actively managed.
Q. How can organizations tell if post-conversion issues are temporary or structural?
Temporary issues typically improve within weeks as users adapt. Structural problems persist across multiple cycles and manifest as sustained declines in note closure, coding throughput, or clean-claim rates. Monitoring these signals early helps distinguish customary adjustment from deeper workflow misalignment.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
CO 11 Denial Code: What It Means and How to Fix It
What Is An Additional Diagnosis In Medical Coding And Why It Matters For Reimbursement?
Related Post
Top Products

%201.png)








