.webp)
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?

CPT or Current Procedural Terminology refers to a set of medical codes that are used to define the different medical services administered by hospitals and other healthcare providers. One of the factors behind assigning codes to each medical service category is to avoid ambiguity and confusion surrounding billable services and support the revenue cycle management system. Accurate medical coding is a key contributor to any hospital’s revenue. With CPT codes, billing teams can efficiently define and strategize important procedures and submit accurate claims without worrying about denials. These codes are updated, defined, and maintained by the AMA, which is an association comprising expert physicians, clinicians, and doctors. The aim of introducing CPT was to standardize a list of medical codes for common medical activities, easing the burden for medical administrative teams and billing personnel.
In this article, we discuss the meaning and relevance of CPT coding in modern medical RCM systems and how the RapidClaims software integrates them in daily workflows to ensure a hassle-free claim process.
What Are CPT Codes?
The Current Procedural Terminology (CPT) code set is a standardized medical code set developed, updated, and maintained by the AMA. Each CPT code is five characters long, can be numeric or alphanumeric, and is used to define several medical services that are categorized based on their function. Without CPT codes, the medical insurance process would lack standardization, become error-prone, causing inconsistencies in reimbursement, ultimately affecting revenue flow. For modern healthcare, CPT is not just another set of medical codes. It lays the foundation for a streamlined and transparent billing process.
The concept of CPT codes was developed in the year 1966, when experts in healthcare felt the need to categorize and consolidate medical services for easy administration.
A Brief History of CPT Codes
CPT codes were first introduced by the AMA in 1966 as a measure to standardize medical codes for medical services belonging to different categories. This change was proposed keeping in mind the exponential growth and gradual integration of technologies like AI into medical billing workflows. With the development of technology and increasing disease complexity, there arose a need to standardize medical coding, with mandatory regulations and regular updates.
RapidClaims enables healthcare organizations to stay updated with the help of autonomous coding and documentation improvement solutions. Medical services are categorized into four major sections, based on their function.
CPT Codes In Medical Billing – Structure & Categories
All medical services are assigned risk levels and categorized based on their relevance in the wider scheme of things. CPT codes representing each of these categories are also bifurcated accordingly. These categories are identified based on the purpose of each service and its relevance to the medical coding and billing systems.
Category I: Commonly Performed Procedures
This category includes generic, everyday medical processes, such as hospital visits, surgical procedures, diagnostic tests, and preventive care services.
The presence of these codes in a patient’s medical documentation are common, and hence widely accepted by payers, directly impacting reimbursement to the healthcare provider.
Category II: Performance Measurement Codes
Performance measurement codes are mainly used for administrative purposes, especially for value-based care systems. Although these codes do not directly influence treatment methods and procedures, they are essential to ensure optimal patient care and quality enhancement of ongoing treatment processes.
These codes are primarily meant to capture details such as:
- Quality of patient care.
- Clinical outcomes
- Adherence to evidence-based guidelines.
- Preventive care procedures and follow-up activities.
Modern healthcare is slowly shifting away from the fee-for-service model to a value-based care system. Category II CPT codes are essential for hospital management to understand and optimize performance-driven reimbursement processes.
Accurate documentation of these codes helps healthcare providers understand the quality of care provided to patients, how a particular anomaly was treated, and the consequent outcome, creating an effective feedback system that helps both payers and providers equally. Strict adherence to capturing category II codes ensures accountability and transparency in the reimbursement and billing process.
Category III: Codes for emerging & experimental procedures
CPT codes of this category define new and upcoming medical treatments and protocols, which are yet to gain mainstream acceptance. While beneficial to patients, Category III CPT codes indicate a healthcare establishment’s openness to novel medical practices. However, payers consider such recommendations to be highly risky, hampering chances of successful reimbursements for private practices, hospitals, and other healthcare providers.
These codes play a critical role in modern healthcare by enabling the industry to monitor innovation, assess clinical effectiveness, and collect data for future procedures and technologies.
CPT Codes Vs. ICD-10 Codes – What’s The Difference?
CPT and ICD-10 codes serve similar purposes, however, their functions are distinct. While CPT codes define a medical service or procedure, ICD-10 codes explain the reason why that particular procedure was recommended or undertaken. In medical coding, it is important that both ICD-10 and CPT codes align with each other. A procedure that doesn’t match the diagnosis, can create documentation errors, leading to a hard denial. RapidClaims uses AI driven code validation to avoid redundancies and identify any CPT-ICD 10 mismatches, enabling a robust RCM system.
Why CPT Codes Are Important To Revenue Cycle Management?
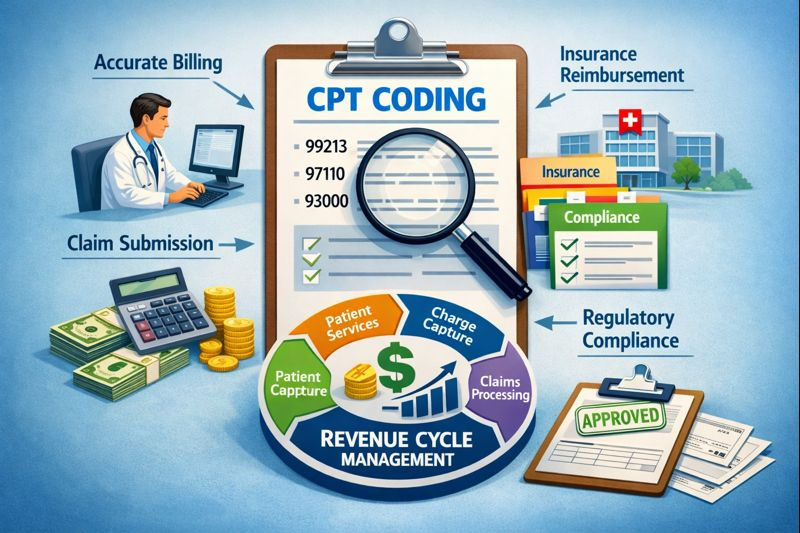
CPT codes serve multiple purposes, from capturing billable services to defining medical procedures for different diagnoses; their role is instrumental to any healthcare RCM system. They are not just billing identifiers, they are the foundation of an efficient RCM system. CPT codes define a vast range of medical services, from hospital visits till the last point of treatment, care and billing, CPT codes cover it all.
RapidClaims views CPT code set as a strategic point to enhance and ensure stable reimbursements, while ensuring optimum patient care.
CPT Codes & Charge Capture Accuracy
Accurate CPT codes ensure that billable medical services are accounted for, providing transparency and clarity to payers, making the reimbursement process smooth and efficient, causing a stable revenue stream. If CPT codes are:
Missing: It can cause services to go unbilled, leading to an imbalance in the billing cycle, causing direct revenue loss.
Incorrect coding: This can lead to hard denials, directly affecting the healthcare provider’s caregiving ratings, and underpayment for medical services, affecting the revenue cycle.
Incomplete coding: Leads to payers questioning the medical necessity for the services provided. Hard inquiries are initiated, questioning a hospital’s integrity and a downfall in the overall ratings.
RapidClaims leverages AI to identify and detect any coding anomalies automatically, allowing billing teams to oversee coding inconsistencies and capture them well in time.
CPT codes in claim creation and submission
Once the charges are captured accurately, payers rely on CPT codes to determine important parameters like:
- What service was performed.
- Whether the level of medical necessity matches the captured procedure.
- Whether it complies with the current regulations.
- It helps teams determine how much money has to be reimbursed to healthcare providers.
CPT Codes & Reimbursement Accuracy
CPT codes can directly impact how much healthcare providers get paid for their services. Hence, it is important to have an autonomous system in place to check for minor inconsistencies and coding errors. Leveraging AI-powered algorithms and tools to do so can be beneficial in the long run.
Accurate CPT coding ensures:
- Correct reimbursement of amounts.
- The medical procedures performed justify the risk level and medical necessity mentioned in the records.
- Reduced underpayments.
- Lesser post-payment adjustments and negotiations.
CPT coding is essential in ensuring that the reimbursements handed out to hospitals and private practices are justified without confusing both payers and patients. Rapid Claims uses AI-powered code detection and validation to prevent common errors, making the billing process smooth and effective.
Common CPT Coding Challenges in Modern Healthcare
One of the most common sources of errors that cause billing issues stems from inaccurate or inconsistent coding practices. Here are some of the most common coding issues that most billing teams face while processing medical bills for huge amounts.
- Undercoding and overcoding
- Unbundling services
- Misuse of modifiers or sometimes, even omission.
- Outdated CPT codes.
- Incomplete documentation.
These errors not only increase the chances of incorrect reimbursements but also improve the chances of audit, causing a spike in operational costs.
Conclusion
Inaccurate or inconsistent CPT codes cause close to 25% of hard denials, causing major revenue drainage. CPT codes are not just administrative identifiers. They are crucial to running a stable revenue cycle management system and contribute to the overall financial health of healthcare providers. When managed effectively, accurate CPT coding can benefit not just patients but also healthcare providers. The widespread use of AI in healthcare indicates the need to incorporate AI-based tools in the regular billing workflows. With RapidClaims RCM, you can optimize repetitive tasks, ensure accurate CPT coding and assignment, leading to a justified reimbursement process.
FAQs
How does CPT coding affect a healthcare provider’s revenue inflow?
CPT codes define medical, surgical, and diagnostic services rendered to patients. Insurance providers mainly check for these codes to verify and validate reimbursement claims. Inconsistent and inaccurate codes raise red flags, causing payers to reject hospital claims, causing a revenue drainage for the involved hospital.
How does AI help improve CPT coding accuracy?
AI-powered RCM platforms analyze historical claims, payer rules, and coding patterns to identify errors before submission. This helps reduce manual mistakes, improve clean claim rates, and prevent avoidable denials.
How does RapidClaims help manage CPT coding challenges?
RapidClaims uses AI-driven validation, payer-specific rules, and denial analytics to detect CPT errors early, reduce coding-related denials, and improve overall revenue cycle efficiency.
Latest Post
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
What Is An Additional Diagnosis In Medical Coding And Why It Matters For Reimbursement?
Top Products

%201.png)








