.webp)
Common Medical Billing and Coding Errors and How to Protect Your Practice


Medical billing and coding errors are a major cause of lost revenue for healthcare providers, with an estimated 80% of claims being denied due to incorrect coding. These errors cost Americans $210 billion annually, with up to 75% of medical bills containing coding errors that contribute to 42% of Medicare claim denials. Errors such as incorrect procedure codes, missing patient information, or mismatched diagnosis and treatment details can lead to financial loss, delayed reimbursements, increased administrative burden, and potential compliance risks for healthcare providers.
Recognizing these common mistakes early is crucial to protecting your practice from costly errors. In this blog, we will explore the most frequent medical billing and coding mistakes, why they happen, and how you can prevent them."
6 Most Common Medical Billing and Coding Errors
A thorough understanding of the most common medical billing and coding errors is vital for minimizing their impact and safeguarding the financial health of healthcare practices. Below are the key errors frequently encountered:
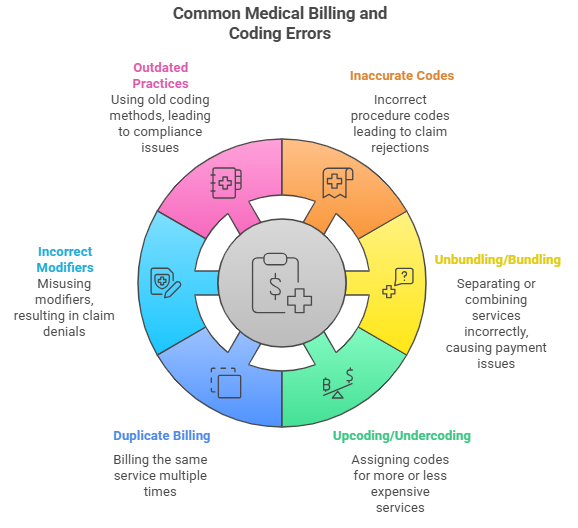
1. Inaccurate Procedure and CPT/HCPCS Codes
One of the most frequent mistakes in medical coding is the application of incorrect procedure codes, whether it’s for the diagnosis, treatment, or service provided. Using the wrong CPT (Current Procedural Terminology) or HCPCS (Healthcare Common Procedure Coding System) code can lead to claim rejections or underpayment.
2. Unbundling and Bundled Charges Issues
Unbundling occurs when a healthcare provider incorrectly separates a group of related services and bills them individually. Bundled billing, on the other hand, involves incorrectly combining services that should be billed separately. Both errors can lead to denied claims or delayed payments.
3. Upcoding and Undercoding Challenges
Upcoding refers to assigning a code for a more expensive service than what was actually provided. Undercoding happens when a less expensive code is used, resulting in lower reimbursement. Both practices can lead to compliance issues and financial losses.
4. Duplicate Billing Instances
Duplicate billing occurs when the same service or procedure is billed more than once. This error can happen due to clerical mistakes or software glitches, but it often results in overpayments or chargebacks.
5. Incorrect Modifier Applications and Documentation
Modifiers are used in medical coding to indicate that a service or procedure has been altered in some way. Incorrectly applying modifiers or failing to include necessary documentation can result in claim denials and lost revenue.
6. Errors Due to Outdated Coding Practices
Medical coding is constantly evolving, with new codes introduced regularly. Using outdated coding practices can result in inaccurate billing, insurance claim denials and compliance violations.
Recognizing and addressing these common medical billing and coding errors is crucial, as they can lead to claim denials, compliance issues, and significant financial losses. Staying updated and vigilant helps protect a healthcare practice’s revenue and reputation.
Impact of Medical Billing and Coding Errors
Medical billing and coding errors can have far-reaching effects on healthcare practices, affecting everything from cash flow to patient care. The financial impact alone can be significant. However, errors don't stop there; they can also impact patient outcomes and even bring legal issues. Here’s a breakdown of the main issues caused by these errors:
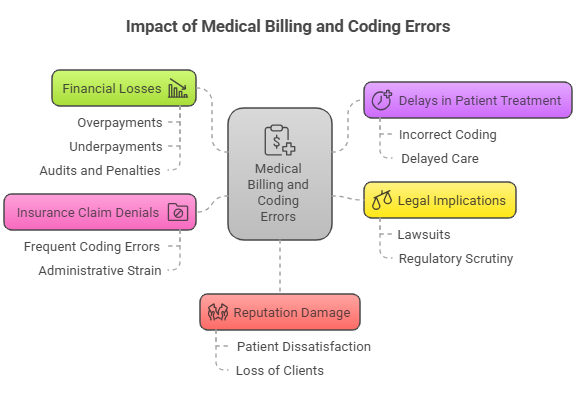
1. Financial Losses Due to Billing Errors
Billing errors can lead to overpayments or underpayments, which may destabilize your practice financially. Incorrect coding may lead to denied or delayed claims, affecting your cash flow. These errors can also trigger audits and penalties from insurers or regulators.
2. Delays in Patient Treatment and Care
Coding mistakes can lead to delays in treatment as claims are processed incorrectly or are sent back for rework. This can impact patient satisfaction and potentially harm the patient’s health due to delayed care.
3. Legal Implications and Compliance Issues
Improper billing practices may not only lead to financial penalties but can also lead to lawsuits and regulatory scrutiny. Healthcare providers must adhere to strict coding regulations, such as those outlined by HIPAA and CMS.
4. Insurance Claim Denials
Frequent coding errors often result in claim denials, requiring additional time and resources to rectify the issue. This can strain administrative resources, delaying reimbursement and negatively impacting practice profitability.
5. Reputation Damage
Healthcare providers rely on their reputation to build trust with patients and insurers. Frequent billing errors may harm that reputation, leading to patient dissatisfaction and a potential loss of clients.
To avoid these common medical coding errors, regular staff training and updated coding tools are vital. Consider using RapidClaims, which uses AI and automation to improve coding accuracy, speed up revenue cycles by processing over 100 charts per minute, ensure compliance with built-in regulatory rules, and lower administrative costs by reducing manual work.
Strategies to Avoid Medical Billing and Coding Errors
Preventing medical billing and coding errors involves proactive measures, such as staff training, regular audits, and investing in updated tools. Let’s explore some strategies to keep your billing and coding accurate.
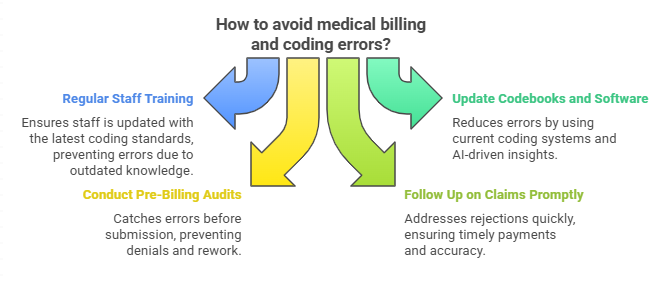
- Regular Staff Training: The healthcare industry constantly updates its codes and procedures. Regular training ensures that your staff remains well-versed in the latest coding standards and guidelines. This prevents errors due to outdated knowledge and maintains compliance.
- Implementing Updated Codebooks and Software: Using outdated codebooks or software can lead to errors. By updating your codebooks and integrating advanced software systems into your practice, you can significantly reduce coding mistakes. Tools like RapidClaim offer AI-driven insights to help identify coding errors before submission.
- Conducting Pre-Billing Audits: Implementing pre-billing audits allows your team to catch potential errors before submitting claims. Catching errors early can prevent denials and costly rework.
- Following Up on Claims Promptly: A timely follow-up on claims ensures that rejections are quickly addressed. This helps in avoiding delayed payments and ensuring the accuracy of your submissions.
- Strengthen Documentation Practices: Complete and accurate documentation is essential for medical billing accuracy. Ensure all patient records, treatments, and codes are thoroughly documented and easily accessible.
Consider using RapidClaims for pre-billing audits, real-time tracking, and AI-driven features that help catch errors early in the billing cycle.
How Technology and Tools Help Prevent Medical Billing and Coding Errors?
Using the right technology can significantly reduce billing and coding mistakes. Smart tools offer real-time insights, flagging errors before claims go out. Here are key solutions that can strengthen your revenue cycle:
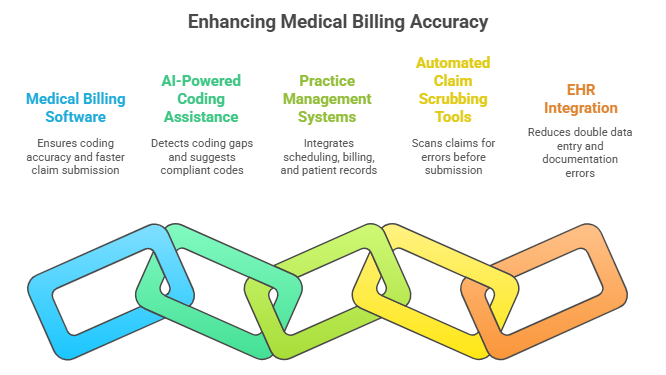
1. Medical Billing Software
Investing in reliable billing software ensures coding accuracy and faster claim submission. It also helps track payer rules and updates automatically. This reduces the risk of denials due to outdated codes.
2. AI-Powered Coding Assistance
AI-driven coding tools detect missing documentation and coding gaps in real-time. Platforms like RapidClaim automatically suggest compliant CPT and ICD-10 codes based on clinical notes, ensuring accurate and up-to-date coding. These tools boost claim acceptance rates and minimize manual errors, improving overall efficiency and reducing the risk of costly rework or claim denials.
3. Practice Management Systems (PMS)
PMS platforms integrate scheduling, billing, and patient records into one system. They improve workflow efficiency and prevent billing mistakes caused by data mismatch. This keeps billing teams organized and claims clean.
4. Automated Claim Scrubbing Tools
Claim scrubbing tools scan claims for errors before submission to payers. They flag missing modifiers, coding conflicts, and policy violations. Fixing issues upfront speeds up approvals and shortens payment cycles.
5. Electronic Health Records (EHR) Integration
Connecting billing systems with EHRs reduces double data entry and documentation errors. Direct coding from patient encounters also ensures higher billing accuracy. This leads to fewer rejections and faster reimbursements.
If you want to safeguard your practice from costly mistakes, build a strong billing and coding strategy. RapidClaims automates the process by detecting coding errors and missing documentation before claim submission. Its AI-driven insights boost claim acceptance rates, while customized rule sets adapt to different specialties. RapidClaims also keeps your coding updated automatically with payer rules, NCCI edits, and LCD/NCD compliance, helping you stay accurate and efficient.
Improving Communication and Collaboration
Strong communication between billing, coding, and clinical teams is key to reducing errors. When coders have direct access to clinical staff for clarification, it helps prevent incorrect code selection and missing documentation. Establishing clear communication channels, such as regular meetings or quick-response chats, can help teams resolve questions early and avoid claim denials later.
Encouraging collaboration between providers and coders also builds a stronger understanding of documentation needs. Providers who understand common coding issues can document services more clearly, supporting accurate coding from the start. Additionally, staying informed about insurance payer policies ensures that teams apply the correct coding guidelines, reducing rejected claims and protecting practice revenue.
Choosing the Right Coding Partner
Choosing the right coding partner plays a major role in reducing billing errors and maintaining compliance. Look for providers that prioritize strong coder training, specialty expertise, and a thorough understanding of payer requirements. A reliable partner should have certified coders, proven auditing processes, and clear quality assurance standards to help prevent mistakes like upcoding, unbundling, and incorrect modifiers.
Third-party coding providers can also help practices manage billing accuracy by offering specialized teams trained across multiple specialties. They often bring updated knowledge of payer rules, CMS guidelines, and coding changes, which can help your internal team stay compliant without getting overwhelmed. However, it is important to evaluate their track record, security protocols, and auditing capabilities before making a decision.
Now that we’ve explored common billing and coding errors and strategies to prevent them, let’s see how RapidClaim can help streamline your practice's billing process and reduce these errors with its AI-powered solutions.
RapidClaims: Simplifying Medical Coding and Billing
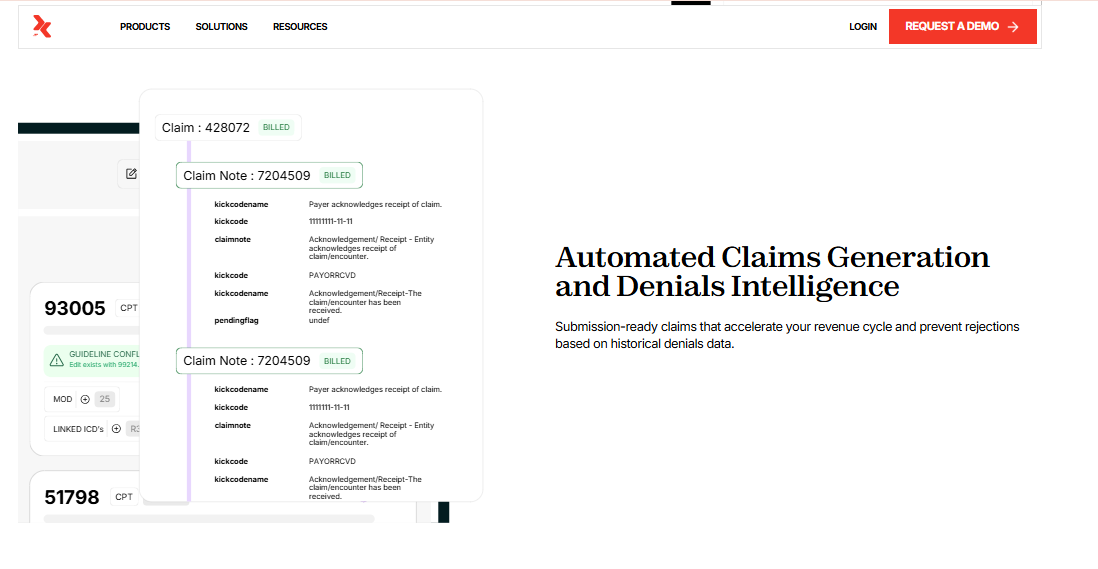
RapidClaims is an AI-driven medical coding automation platform that streamlines coding operations, reduces administrative costs, improves reimbursement processes, and ensures compliance with industry standards. Unlike traditional solutions that require lengthy onboarding, RapidClaims offers pre-built API integrations for easy setup, minimal IT workload with cloud-based deployment, and custom rule sets customized for specialty-specific coding, ensuring quick and efficient implementation.
- Automate and Assist
RapidClaims automates medical coding with AI, offering coder-assisted recommendations for improved efficiency. It processes thousands of charts per minute with high accuracy, reducing errors and administrative costs.
- Explainable and Compliant AI
With a full audit trail for every code, RapidClaims ensures transparency and compliance. The AI accurately interprets medical notes, diagnoses, and procedures while adhering to ICD-10, CPT, HCPCS, and E&M guidelines.
- Actionable Insights
RapidClaims detects coding errors and missing documentation before submission, reducing rejections. AI-driven real-time insights improve claim acceptance rates and streamline reimbursement processes.
- Customized AI & Rule Sets
RapidClaims adapts coding logic to fit each specialty and updates based on payer rules, NCCI edits, and LCD/NCD compliance, ensuring accuracy and up-to-date coding practices.
- Security & Privacy
Fully HIPAA-compliant and encrypted, RapidClaims ensures secure data handling and meets U.S. data residency requirements for regulatory compliance, protecting sensitive patient information.
These features help hospitals, physician groups, medical billing companies, and Accountable Care Organizations (ACOs) minimize claim denials and accelerate revenue cycles.
Conclusion
Medical billing and coding errors can lead to significant consequences, including financial losses and compliance issues. By implementing regular training, using advanced software, and ensuring clear communication, practices can prevent common coding errors and safeguard their financial health.
Consider adopting RapidClaims, an advanced solution that streamlines your billing and coding process, reduces errors, and ensures compliance. With AI-driven features and automated error-checking, RapidClaims can help safeguard your practice from the costly consequences of coding mistakes.
Schedule a Free Demo today to see how RapidClaims can enhance your billing accuracy and help you avoid common medical coding errors.
FAQs
1. What certifications should healthcare providers look for when hiring medical coders?
Healthcare providers should prioritize certifications like the CPC (Certified Professional Coder) from AAPC or the CCS (Certified Coding Specialist) from AHIMA when hiring medical coders. These certifications ensure the coder’s expertise and familiarity with healthcare coding standards.
2. How often must healthcare providers ensure their certified medical coders complete recertification?
Healthcare providers should ensure that their certified medical coders complete continuing education units (CEUs) annually and recertify every 2-3 years. This process ensures that coders are up to date with the latest industry regulations and coding guidelines.
3. How do healthcare providers avoid common medical coding errors when dealing with multiple insurance companies?
To minimize coding errors across multiple insurance companies, healthcare providers must stay updated with each insurer’s specific rules and guidelines. Implementing automated coding systems, conducting regular audits, and training staff on various payer requirements can help ensure accuracy.
4. Can medical coding automation completely replace human coders?
While automation tools are improving efficiency, human coders will still be necessary for complex cases, decision-making, and ensuring compliance with ever-evolving coding standards. Automation can assist coders but not fully replace the need for human oversight in the coding process.
5. How can medical coders keep up with frequent changes in coding standards and regulations?
Medical coders can stay updated by attending continuing education courses, subscribing to industry newsletters, and participating in coding seminars and webinars. Joining professional organizations, like the American Health Information Management Association (AHIMA), also provides access to resources that help coders stay informed.
6. How do I handle coding for rare or experimental treatments that don’t have established codes?
For rare or experimental treatments without established codes, coders can use "unclassified" or "unspecified" codes temporarily. It’s important to document these treatments thoroughly and work closely with healthcare providers to assign the most accurate codes available until a specific code is introduced.
%201.png)