.webp)
ICD-10 HCC: A Complete Guide for Healthcare Professionals

Staying ahead in healthcare finance begins with precision. In 2025, the Medicare Advantage and Part D Advance Notice Fact Sheet announced that risk scores are now calculated using a blended approach, with 67% coming from the updated 2024 CMS-HCC model and 33% from the legacy 2020 model. This change highlights just how much accurate documentation and coding influence reimbursement and compliance across the industry.
Risk adjustment ensures that providers are fairly reimbursed based on the complexity of their patients. ICD-10 HCC is the coding framework at the center of this process, driving value-based care, Medicare Advantage, and population health programs. Accurate HCC coding strengthens compliance, financial stability, and patient care outcomes.
In this blog, you’ll learn what ICD-10-HCC is, how risk adjustment works, why accuracy matters, common codes, challenges, best practices, and the role of technology.
TL;DR (Key Takeaways)
- Accurate ICD-10 HCC coding has a direct impact on RAF scores, reimbursement, and regulatory compliance.
- Chronic conditions must be documented annually and meet MEAT criteria to qualify for HCC coding.
- Proper HCC mapping ensures ICD-10 codes reflect patient risk and prevent under- or overpayment.
- Common coding errors include incomplete documentation, failure to recapture conditions, and over-reliance on EMR auto-suggest.
- Automation tools like RapidClaims improve coding accuracy, streamline workflows, and optimize risk-adjusted payments.
Table of Contents:
- Understanding ICD-10 HCC and Its Role in Risk Adjustment
- How does ICD-10 HCC Risk Adjustment Works?
- Importance of Accurate ICD-10 HCC Coding
- Common ICD-10 HCC Codes and Their Clinical Significance
- Essential Elements of Accurate ICD-10 HCC Coding
- Best Practices to Tackle ICD-10 HCC Coding Issues
- Conclusion
- Frequently Asked Questions (FAQs)
Understanding ICD-10 HCC and Its Role in Risk Adjustment
ICD-10-HCC is a risk-adjustment model developed by the CMS. It links ICD-10-CM codes (diagnoses) to HCC categories, which are then used to calculate a patient’s risk score. This risk score helps determine the expected healthcare costs for each patient and ensures that providers serving high-acuity populations receive fair reimbursement.
Essentially, ICD-10-HCC coding transforms clinical documentation into data-driven risk profiles. For example, diabetes without complications maps to a lower HCC weight than diabetes with chronic complications, reflecting the difference in care resources required.
Now, let's see how ICD-10 HCC risk adjustment works in practice, since that’s what drives its importance in healthcare reimbursement.
How does ICD-10 HCC Risk Adjustment Work?
The HCC risk adjustment model estimates patient cost risk using demographics and ICD-10-CM diagnoses. Each qualifying diagnosis maps to a Hierarchical Condition Category (HCC), which contributes to a Risk Adjustment Factor (RAF) score. Higher RAF scores reflect greater predicted healthcare costs.
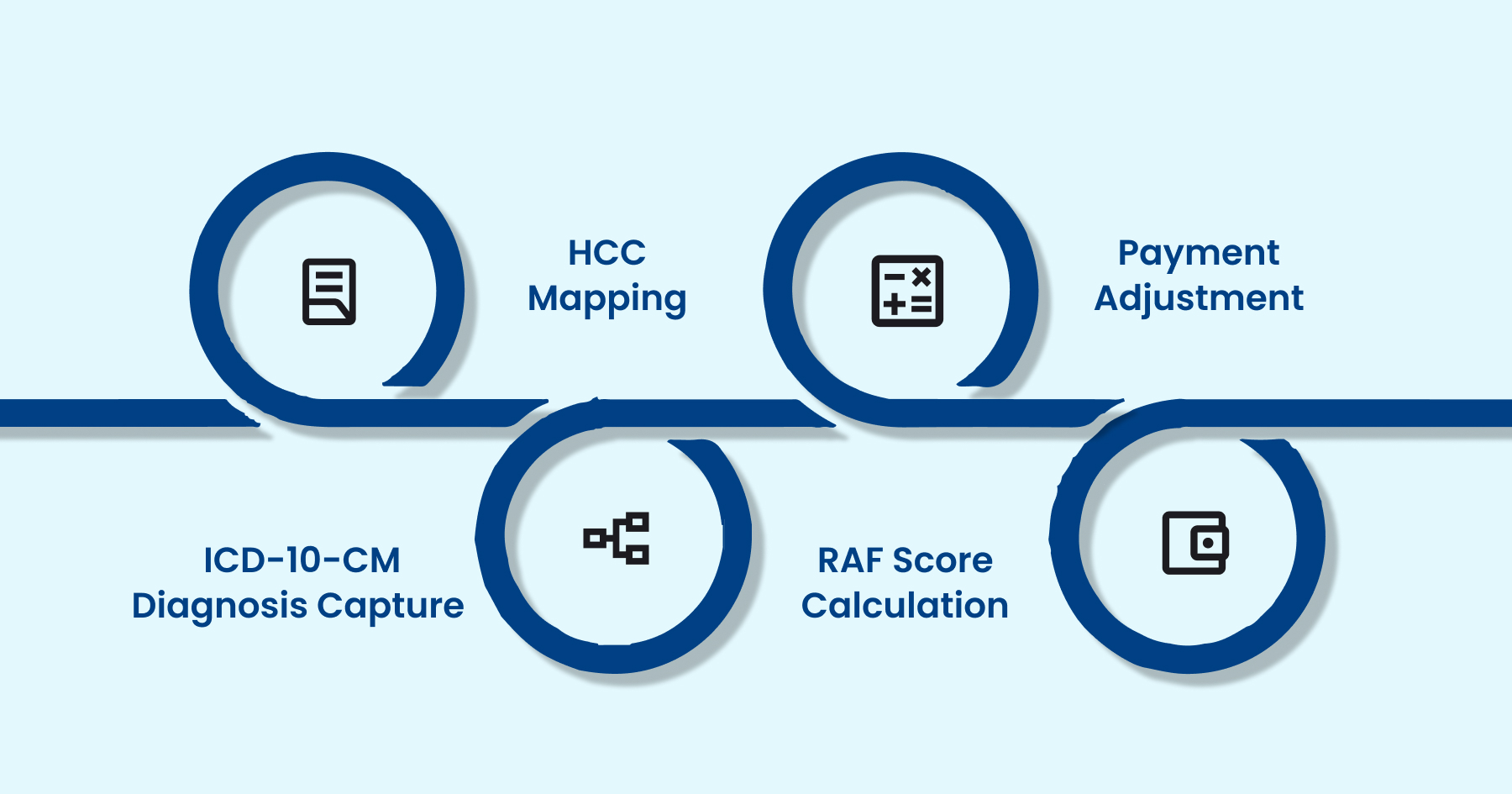
Below are the key steps in the HCC risk adjustment process:
Step 1: ICD-10-CM Diagnosis Capture
Accurate diagnosis coding is the foundation of risk adjustment. All conditions documented in provider records must be coded to the highest specificity. Chronic conditions must be reported annually, and any missing or unspecified codes can result in a reduced RAF score, leading to lower reimbursement and an inaccurate risk assessment.
Step 2: HCC Mapping
Once captured, ICD-10-CM codes are grouped into HCCs using CMS mapping logic. HCCs represent clinically significant conditions that drive costs, such as heart failure, chronic kidney disease, or diabetes with complications. Not all ICD-10 codes map to HCCs, making it crucial to identify and report qualifying conditions accurately.
Step 3: RAF Score Calculation
Each HCC has a numerical weight based on expected healthcare costs. Demographics like age, gender, Medicaid eligibility, and disability status are included. Hierarchies prevent double-counting, e.g., diabetes with complications overrides diabetes without complications. The final RAF score reflects the patient’s overall risk.
Step 4: Payment Adjustment
RAF scores are applied to adjust payments in Medicare Advantage and other risk-based contracts. Higher RAF scores result in higher reimbursement to reflect expected care needs. Incomplete or inaccurate coding leads to underpayment and compliance risks, making precise documentation and coding essential for both financial and clinical accuracy.
By following these steps, providers can ensure accurate diagnosis capture, HCC mapping, and RAF calculation, thereby ensuring proper risk scoring and reimbursement. Automation tools, such as RapidClaims, further streamline this process by cross-referencing ICD-10, CPT, and HCPCS codes, reducing errors, minimizing denials, and improving revenue cycle efficiency.
Importance of Accurate ICD-10 HCC Coding
Accurate ICD-10 HCC coding is crucial for both regulatory compliance and ensuring financial performance, as well as delivering high-quality patient care. Errors or omissions in coding can have significant downstream effects on reimbursement, reporting, and clinical decision-making.
Below are a few key reasons why precise HCC coding matters:
- Reimbursement Accuracy: Inaccurate coding can underrepresent a patient’s risk profile, resulting in a lower RAF score and reduced payments for providers.
- Regulatory Compliance: CMS audits coding practices to detect under coding, over coding, or fraudulent reporting. Maintaining accurate HCC coding ensures adherence to federal regulations and reduces the risk of audit.
- Population Health Management: Correct risk-adjusted data allows healthcare organizations to identify high-risk patients, allocate resources efficiently, and implement targeted care coordination programs.
- Quality of Care Documentation: Detailed and accurate coding reflects the actual disease burden of patients, supporting treatment planning, chronic disease management, and quality reporting initiatives.
Coding errors result in lost revenue and create compliance risks. Therefore, well-trained coding teams and clinical documentation improvement (CDI) programs are essential.
To make this more concrete, let’s look at some of the most common HCC ICD-10 codes that coders and providers encounter in everyday practice.
Common ICD-10 HCC Codes and Their Clinical Significance

The following is a curated list of ICD-10-CM codes commonly mapped to HCCs, based on the 2025 reference from Blue Cross Blue Shield of Alabama. Each code is paired with a concise explanation of its clinical relevance, helping providers understand both the condition and its impact on risk adjustment and reimbursement.
1. Diabetes Mellitus
Diabetes is a common chronic condition that often leads to multiple complications affecting nerves, kidneys, eyes, and peripheral circulation. Accurate coding of these complications is essential for risk adjustment and proper reimbursement.
- E10.40 / E11.40 – Diabetes with diabetic neuropathy, unspecified: Indicates nerve damage caused by diabetes.
- E10.42 / E11.42 – Diabetes with polyneuropathy: Multiple nerve involvement due to diabetes.
- E10.22 / E11.22 – Diabetes with diabetic chronic kidney disease: Diabetes complicated by chronic kidney disease.
- E10.21 / E11.21 – Diabetic nephropathy: Kidney damage directly caused by diabetes.
- E10.31 / E11.31 – Diabetic retinopathy, unspecified: Retinal damage from diabetes affecting vision.
- E10.51 / E11.51 – Diabetic peripheral angiopathy without gangrene: Peripheral vascular disease without tissue death.
- E10.52 / E11.52 – With gangrene: Peripheral vascular disease with tissue necrosis.
- E10.621 / E11.621 – Foot ulcer: Diabetic ulceration on the foot, often a precursor to infection or amputation.
2. Endocrine & Metabolic Disorders
Endocrine and metabolic disorders can significantly increase patient risk scores due to associated comorbidities and long-term health complications.
- E66.01 – Morbid obesity due to excess calories: Severe obesity with significant health risk.
3. Mental, Behavioral & Neurodevelopmental Disorders
Mental health and neurodevelopmental conditions impact both functional status and healthcare utilization. Proper documentation ensures these conditions are reflected in risk adjustment calculations.
- F03.90 – Dementia, unspecified, without behavioral disturbance: Cognitive decline without behavioral symptoms.
- F03.91 – Dementia with behavioral disturbance: Cognitive decline accompanied by behavioral issues.
- F32.1 – Major depressive disorder, single episode, moderate: Clinically significant depressive episode.
- F32.2 – Severe single episode without psychotic features: Severe depression without psychosis.
- F32.3 – Severe single episode with psychotic features: Severe depression with psychotic symptoms.
- F33.1 – Recurrent moderate depression: Multiple depressive episodes of moderate severity.
- F33.3 – Recurrent severe depression with psychotic features: Severe, recurring depression with psychosis.
- F50.2 – Bulimia nervosa: Eating disorder characterized by bingeing and purging.
- G30.9 – Alzheimer’s disease, unspecified: Progressive neurodegenerative disorder affecting memory and cognition.
4. Neurological Conditions
Neurological disorders such as epilepsy and convulsions require careful documentation for appropriate risk adjustment and management.
- G40.909 – Epilepsy, unspecified, not intractable: Seizure disorder not resistant to treatment.
- R56.9 – Unspecified convulsions: Non-specific seizure events requiring monitoring.
5. Cardiovascular
Cardiovascular conditions often drive high healthcare costs due to chronic management and complications. Accurate coding ensures that risk-adjusted payments accurately reflect the true complexity of each patient.
- I11.0 – Hypertensive heart disease with heart failure: High blood pressure causing structural heart damage and heart failure.
With these real-world examples, it’s clear that ICD-10 HCC coding goes beyond assigning codes. Accurate coding requires systematic documentation, clinical validation, and precise mapping to HCCs for proper risk adjustment.
Essential Elements of Accurate ICD-10 HCC Coding
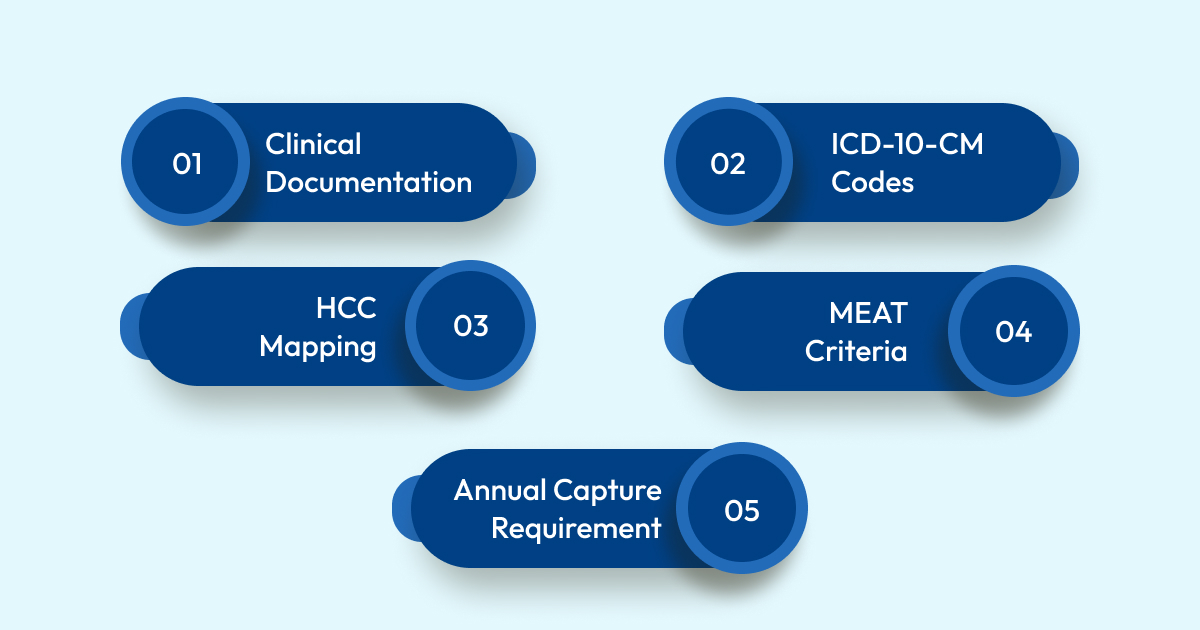
Accurate ICD-10 HCC coding relies on a structured process that integrates documentation, coding, and compliance to ensure correct coding. Each component plays a critical role in ensuring proper risk adjustment and reimbursement:
- Clinical Documentation: Physicians must clearly and thoroughly document all chronic and relevant conditions. Complete documentation provides the foundation for accurate coding and risk assessment.
- ICD-10-CM Codes: Coders convert provider documentation into precise ICD-10 codes. Correct code selection ensures that conditions are accurately reflected in the patient’s risk profile.
- HCC Mapping: Only specific ICD-10 codes qualify for HCC assignment. Mapping determines which conditions carry risk weights and contribute to the patient’s Risk Adjustment Factor (RAF).
- MEAT Criteria: CMS requires that each diagnosis be Monitored, Evaluated, Assessed, or Treated during the encounter. This ensures that only actively managed conditions are included in risk adjustment.
- Annual Capture Requirement: Chronic conditions must be documented and coded every year to maintain accurate RAF scores and avoid underpayment.
These elements demonstrate that ICD-10 HCC coding is not simply a coding exercise; it is a continuous cycle of documentation, validation, and compliance that underpins accurate risk adjustment and quality patient care.
Next, let’s review the common challenges in ICD-10 HCC coding and the best practices to address them effectively.
Best Practices to Tackle ICD-10 HCC Coding Issues
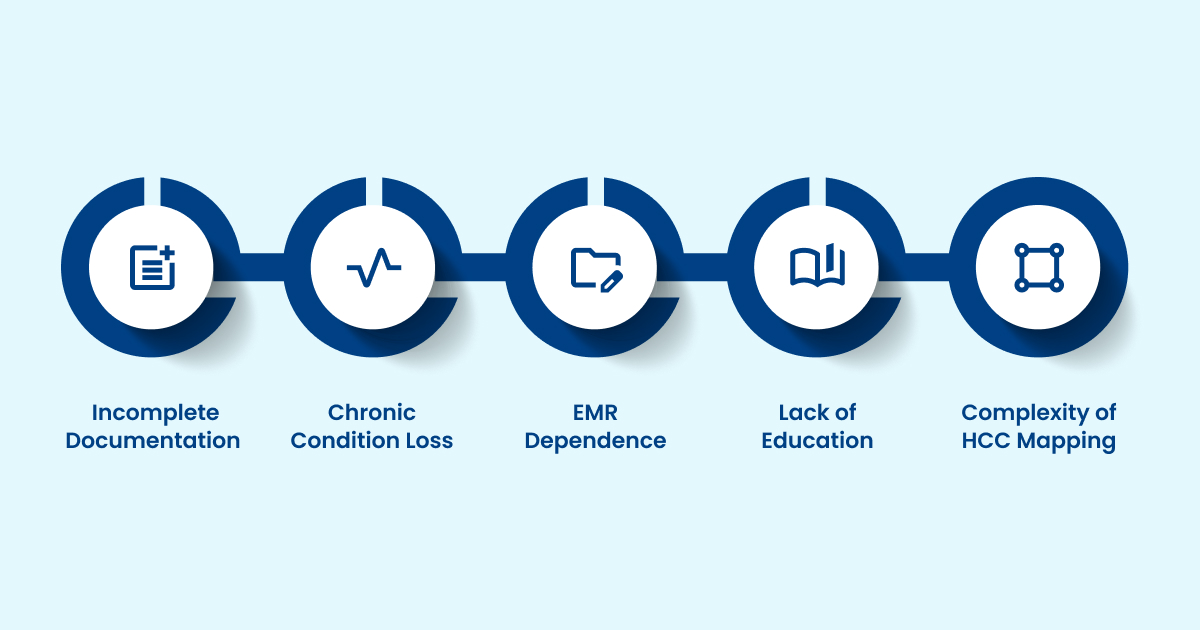
Accurate ICD-10 HCC coding is crucial for risk adjustment, reimbursement, and quality reporting; however, several real-world challenges can compromise coding accuracy. Understanding these pitfalls and adopting best practices helps providers maintain compliance and optimize revenue.
1. Incomplete Documentation: Missing details on disease severity, complications, or comorbidities can understate the patient’s risk, resulting in lower RAF scores.
- Best Practice: Implement structured documentation templates and regular provider audits to ensure that all chronic conditions and complications are fully captured in the medical record.
2. Failure to Recapture Chronic Conditions: Chronic diseases must be documented and coded annually to ensure accurate tracking and management of these conditions. Failing to do so removes these conditions from patient profiles, which reduces reimbursement and distorts population risk data.
- Best Practice: Establish annual coding reviews and automated reminders within the EMR to prompt providers to recapture all chronic diagnoses each year.
3. Over-reliance on EMR Auto-Suggest: Relying solely on EMR auto-suggest can introduce errors, including misclassification or upcoding, as automated recommendations may not accurately reflect clinical nuances.
- Best Practice: Combine EMR suggestions with coder review and clinical validation, ensuring each diagnosis is supported by documentation and meets MEAT (Monitored, Evaluated, Assessed, or Treated) criteria.
4. Insufficient Provider Education: Physicians often under-document or omit conditions due to a lack of awareness about HCC rules, hierarchies, and MEAT requirements.
- Best Practice: Conduct ongoing provider education sessions, share coding tip sheets, and provide feedback on documentation quality to reinforce accurate reporting.
5. Complexity of HCC Mapping and Hierarchies: Certain conditions may be overridden by hierarchical rules, causing confusion and coding errors. Misunderstanding these rules can lead to inaccurate RAF scores.
- Best Practice: Use coding software with built-in HCC mapping validation and provide coders with reference guides on hierarchies to ensure proper code selection.
Implementing these best practices can be further enhanced with automation tools that streamline documentation, coding, and validation. RapidClaims offers a product suite, including RapidCode, which enables few-shot deployment and provides comprehensive coverage of ICD-10/PCS, CPT, and HCPCS guidelines. With explainable AI, continuous learning, and seamless EHR integration, it ensures accurate CPT coding, compliance, and optimized revenue cycle efficiency.
By addressing these challenges systematically, healthcare organizations can improve documentation accuracy, safeguard compliance, and optimize risk-adjusted payments.
Also Read: Intro to Commonly Used Medical CPT/HCPCS Codes List.
Conclusion
Accurate ICD-10 HCC coding is critical for risk adjustment, compliance, and reimbursement. Understanding HCC mapping, RAF scoring, documentation requirements, and common challenges helps providers maintain precise coding and improve patient care. Consistently following best practices, including compliant documentation and annual recapture, ensures both financial and clinical accuracy.
To simplify and streamline this process, RapidClaims offers an AI-driven platform that automates HCC coding, validates documentation, and ensures compliance with CMS guidelines. By integrating with your existing EHR system, RapidClaims helps providers reduce errors, maximize RAF scores, and save significant time on administrative tasks.
Want to improve the efficiency and precision of ICD-10 HCC coding? Request a Free Demo today to see how RapidClaims can streamline your workflow and optimize billing operations.
Frequently Asked Questions (FAQs)
1. Can I use ICD-10 codes for conditions that are not chronic?
No. Acute or non-chronic conditions generally do not map to HCCs. Only chronic conditions that have a significant impact on healthcare costs are eligible. For example, a sprained wrist or a common cold would not receive an HCC code.
2. Can I code a condition if it's not currently being treated but is documented in the patient's history?
Yes, but for risk adjustment, the condition must be actively monitored, evaluated, assessed, or treated during the current encounter to qualify for HCC coding. This follows the MEAT criteria.
3. Can I use the same ICD-10 code for multiple conditions if they share the same code?
No. Each ICD-10 code represents a specific diagnosis. Even if multiple conditions share a code, each must be documented and coded separately to accurately reflect the patient’s health.
4. Can I code a condition if it's not documented in the medical record?
No. Coding undocumented conditions is not permitted and can lead to compliance issues. Only conditions supported by proper documentation should be coded.
5. Can HCC codes change from year to year for the same patient?
Yes. HCC codes can change annually based on current documentation and health status. Conditions must be recaptured annually to accurately reflect the patient’s risk.
%201.png)









