.webp)
Intro to Commonly Used Medical CPT/HCPCS Codes List


Understanding medical coding is essential for healthcare providers, coders, and billers to ensure accurate billing and timely reimbursements. CPT (Current Procedural Terminology) and HCPCS (Healthcare Common Procedure Coding System) codes are the backbone of medical coding, playing a pivotal role in identifying and categorizing medical services.
This blog will guide you through the basics of CPT, HCPCS, and ICD codes, showing how these coding systems ensure precise billing and help reduce common errors. We will also delve into the most frequently used codes in medical practice, clarifying how to apply them for accurate claims.
Foundations of Medical Coding
Medical coding serves as the language of the healthcare industry, allowing providers, payers, and insurers to communicate efficiently. It ensures that the right services are billed correctly and reimbursed on time.
Understanding the differences between the various coding systems—CPT, HCPCS, and ICD—is crucial for accurate billing, compliance, and avoiding costly mistakes. In this section, we'll explore the importance of accurate coding and a breakdown of the key coding systems and their roles in the healthcare ecosystem.
1. Why Accurate Medical Coding Matters
Accurate medical coding is critical for both healthcare providers and patients. When done correctly, it streamlines the billing process, ensures proper reimbursement, and reduces the likelihood of claim denials. However, errors in medical coding can result in underpayment or overpayment, leading to reimbursement delays or compliance issues. Moreover, proper coding enables healthcare organizations to maintain the integrity of their financial systems and ensures that they meet regulatory requirements.
By understanding and applying the correct CPT, HCPCS, and ICD codes, providers can reduce the chances of errors, speed up the revenue cycle, and avoid costly billing mistakes. The importance of medical coding extends beyond billing; it is an essential component of healthcare data management, enabling precise documentation and analysis of medical services.
2. The Difference Between CPT, HCPCS, and ICD Codes
Before diving deeper into CPT and HCPCS codes, it’s important to understand the distinct roles of CPT, HCPCS, and ICD codes in the medical billing system.
- CPT Codes: These codes describe procedures and services performed by healthcare providers. They help specify what medical services were delivered, including office visits, surgeries, diagnostic tests, and therapeutic services.
- ICD Codes: The International Classification of Diseases (ICD) codes describe diagnoses or the conditions that prompted medical procedures. They provide the necessary context for the services rendered, explaining the medical necessity behind a procedure or treatment. For instance, a patient diagnosed with chest pain (ICD code) may undergo a stress test (CPT code), and both codes will be used together for accurate billing.
- HCPCS Codes: The Healthcare Common Procedure Coding System (HCPCS) codes cover services not typically included in CPT codes. These include durable medical equipment (DME), certain drugs, and ambulance services. HCPCS Level I codes are essentially the same as CPT codes, while Level II codes are used for items and services outside the CPT scope.
Understanding these distinctions is key to accurate coding and billing, ensuring that healthcare providers receive the proper reimbursement for their services.
CPT Codes Explained
CPT codes are critical to medical billing. They standardize the description of procedures and services, ensuring accuracy and consistency across the healthcare system. These codes are used to document various medical services, from office visits to surgeries and diagnostic tests.
By understanding how to use these codes correctly, healthcare providers can avoid billing errors, reduce claim denials, and ensure proper reimbursement.

1. What Are CPT Codes & How Are They Used?
CPT codes are standardized codes used to describe medical procedures and services healthcare professionals provide. They are vital for ensuring that healthcare providers are properly reimbursed for their services. Managed by the American Medical Association (AMA), CPT codes are used in both outpatient and inpatient settings and cover a wide range of services, such as surgeries, diagnostic tests, physical therapy, and laboratory work.
CPT codes are broken down into three categories:
- Category I: These are the most commonly used codes, covering routine medical services and procedures.
- Category II: These are performance tracking codes that document measures like patient follow-ups and health assessments.
- Category III: These temporary codes are assigned to emerging medical technologies, services, or procedures.
Accurate use of CPT codes helps healthcare providers ensure timely and correct reimbursement. Applying the right code for the right service reduces the risk of claim rejections and underpayments.
2. The 7 Most Frequently Used CPT Codes (And When to Use Them)
Understanding the most commonly used CPT codes is essential for medical coders and billers. These codes cover frequently performed procedures across various medical specialities. Below are seven examples of CPT codes you will encounter regularly:
- 99213: Used for a typical office visit involving an established patient with moderate complexity.
- 99214: A higher complexity office visit, often used for follow-up visits involving more detailed assessments.
- 97110: Used for therapeutic exercises in physical therapy settings, helping patients improve strength and movement.
- 36415: Used for routine venipuncture (drawing blood).
- 99406: A code for smoking cessation counseling.
- 87635: Used for testing infectious diseases, such as a COVID-19 test.
- 93000: For an electrocardiogram (ECG or EKG), a test that records the electrical activity of the heart.
These CPT codes are used across multiple specialities, from general practice to emergency medicine. It's essential to know when and how to apply these codes to ensure that services are accurately billed and reimbursed.
3. Understanding Modifier Codes: The Key to Avoiding Claim Denials
Modifier codes are additional codes added to CPT codes to provide more specific information about the service performed. They help clarify the circumstances of the service, preventing errors and ensuring that the right procedure is billed accurately.
For instance, Modifier 59 is frequently used to indicate that two procedures performed on the same day are distinct and independent of one another. This modifier is crucial to prevent these services from being bundled together incorrectly.
Modifiers help prevent common billing issues such as:
- Bundling errors: When separate services are incorrectly bundled under one CPT code.
- Payment discrepancies: Ensuring the correct reimbursement for distinct services.
- Claim denials: Properly documenting services to ensure payment approval.
Medical coders must know when and how to apply modifier codes. Correctly using modifiers ensures that healthcare providers are reimbursed appropriately for each distinct service rendered. With the increasing complexity of medical coding, using AI-powered tools like RapidClaims helps improve accuracy, minimize errors, and speed up the billing process.
Using CPT Codes for Evaluation and Management
CPT codes for Evaluation and Management (E&M) are key to distinguishing between different levels of patient care, from simple office visits to more detailed, complex consultations. These codes ensure that the services provided are accurately documented, reflecting the true level of care.
Proper use of E&M codes directly affects reimbursement, making it essential for healthcare providers to select the correct code based on the complexity and duration of the visit.
1. Codes Used for Initial Evaluations and Re-evaluations in Medical Settings
CPT codes for Evaluation and Management (E&M) are essential for differentiating between various service levels, from routine office visits to more complex consultations. These codes are vital in documenting the level of care provided to patients, which directly impacts the reimbursement amount healthcare providers will receive.
- 99201 to 99205: These codes are used for new patient visits, with the number increasing based on the complexity and duration of the visit. For example, 99201 is used for a simple visit, while 99205 covers the most complex and time-consuming evaluations.
- 99211 to 99215: These codes are for established patients, with the higher numbers indicating greater complexity in the visit. A 99213 code may be used for a typical follow-up visit, whereas a 99215 code may be applied for more detailed consultations.
When coding for E&M services, it’s crucial to ensure that the level of service is accurately represented. For instance, a basic visit that requires minimal medical history will be billed with a lower code, while a visit requiring a detailed assessment and treatment plan will necessitate a higher-level code.
Case Scenarios for Accurate Billing
Consider this example: A patient with a chronic condition like hypertension visits the doctor for a follow-up. The doctor performs a thorough assessment, adjusts the medications, and provides counselling. The correct CPT code needs to be selected based on the complexity of the visit. For a simple office visit, 99213 might be appropriate, while 99214 would be a better fit for a more complex assessment involving medication changes and counselling.
Choosing the correct CPT code for these E&M services ensures proper reimbursement for the time and resources spent evaluating and managing the patient's condition.
HCPCS Codes & Advanced Coding Concepts
HCPCS codes play a vital role in medical billing by covering services and items that CPT codes don’t fully address, such as medical supplies, specific drugs, and transportation services. With the increasing complexity of healthcare services, understanding the application of both CPT and HCPCS codes is crucial for accurate billing.

1. What Are HCPCS Codes and When Should You Use Them?
The Healthcare Common Procedure Coding System (HCPCS) is a set of codes used to describe services, products, and supplies not covered by CPT codes. HCPCS codes are divided into two levels:
- Level I: These are the same as CPT codes and cover a wide range of medical procedures and services.
- Level II: These codes cover services, products, and supplies not included in the CPT code set, such as durable medical equipment (DME), ambulance services, certain drugs, and medical supplies.
HCPCS Level II codes are particularly important for billing services that fall outside the standard CPT categories. For example, if a patient requires medical transportation by ambulance, an HCPCS Level II code is used to bill for that service, while the corresponding CPT code is used for the procedures performed during the patient’s care.
Understanding HCPCS codes is crucial for comprehensive medical billing. They fill the gaps left by CPT codes, ensuring healthcare providers can be reimbursed for all services provided.
2. HCPCS vs. CPT: Understanding the Key Differences
While CPT codes and HCPCS codes serve similar purposes, there are key differences between the two. CPT codes cover medical procedures and services, including surgeries, diagnostic tests, and office visits. HCPCS codes, on the other hand, extend beyond CPT to cover services and supplies that CPT doesn’t address.
- CPT Codes: Primarily used for medical procedures and services.
- HCPCS Level I: Essentially the same as CPT codes but used for billing additional services not covered under CPT.
- HCPCS Level II: Includes codes for DME, ambulance services, some drugs, and other supplies not included in the CPT code set.
While CPT codes are used for the majority of medical services, HCPCS codes ensure that items and services not directly linked to procedures can still be billed and reimbursed. Both coding systems are necessary for accurate and complete billing.
3. The Role of CCI Edits in Medical Billing
The Correct Coding Initiative (CCI) is a program developed by Medicare to reduce improper coding and prevent overbilling. CCI edits are a set of rules that help coders determine whether certain combinations of CPT codes can or cannot be billed together. These edits ensure that services are not duplicated or billed incorrectly.
For example, when two procedures are part of a single service (bundling), CCI edits prevent both CPT codes from being billed separately, avoiding improper reimbursements. By adhering to CCI edits, healthcare providers can ensure they are following correct billing practices and reduce the chances of claim denials.
The CCI edit list is regularly updated by Medicare, and many private insurers follow similar guidelines to ensure coding accuracy. Coders must regularly check these updates to maintain compliance and avoid errors.
Best Practices & Optimizing Your Coding Process
Optimizing your coding process is essential for improving efficiency, reducing errors, and ensuring timely reimbursement. By following best practices, such as staying updated on the latest code revisions, using modifiers correctly, and avoiding common mistakes, you can streamline your medical billing process.
Additionally, leveraging AI tools like RapidClaims can help automate coding tasks, reduce administrative overhead, and improve overall accuracy. In this section, we've outlined the key practices and tools you can adopt to enhance your coding process and maintain compliance.
The Top 5 Mistakes in Medical Coding (And How to Fix Them)
Accurate medical coding is crucial for ensuring that healthcare providers are reimbursed appropriately and that claims are processed without errors. However, mistakes are common, and even small coding errors can lead to claim denials or underpayment. Below are five common mistakes in medical coding and how you can avoid them:
- Incorrect Use of CPT Codes: One of the most frequent mistakes is applying the wrong CPT code for a service. Ensure that the code used accurately reflects the procedure or service provided. Always double-check the service description and match it with the most specific CPT code available.
- Failure to Use Modifiers: Modifiers like Modifier 59 (distinct procedural services) are crucial for ensuring that separate services are billed correctly. Not using the appropriate modifier can lead to bundling errors or incorrect reimbursements.
- Upcoding or Undercoding: Upcoding involves billing for a higher level of service than was actually provided, which can result in overpayment or compliance issues. Undercoding, on the other hand, means billing for a lower level of service, leading to underpayment. Ensure that the documentation matches the level of service provided and use the correct CPT code.
- Neglecting to Update Codes: CPT codes are revised regularly, and failing to stay current with the latest versions can lead to incorrect billing. Regularly review coding updates from the AMA and other relevant organizations to stay current.
- Not Checking for CCI Edits: Incorrectly combining CPT codes flagged by the Correct Coding Initiative (CCI) can result in claim rejections. Always check the CCI edit list to ensure you're not submitting incompatible codes.
By staying vigilant and using the correct codes, modifiers, and documentation, you can avoid these common mistakes and ensure accurate billing and reimbursement. Automating the coding process with RapidClaims ensures that the latest codes are always applied, reducing human error and improving the overall accuracy of the billing process.
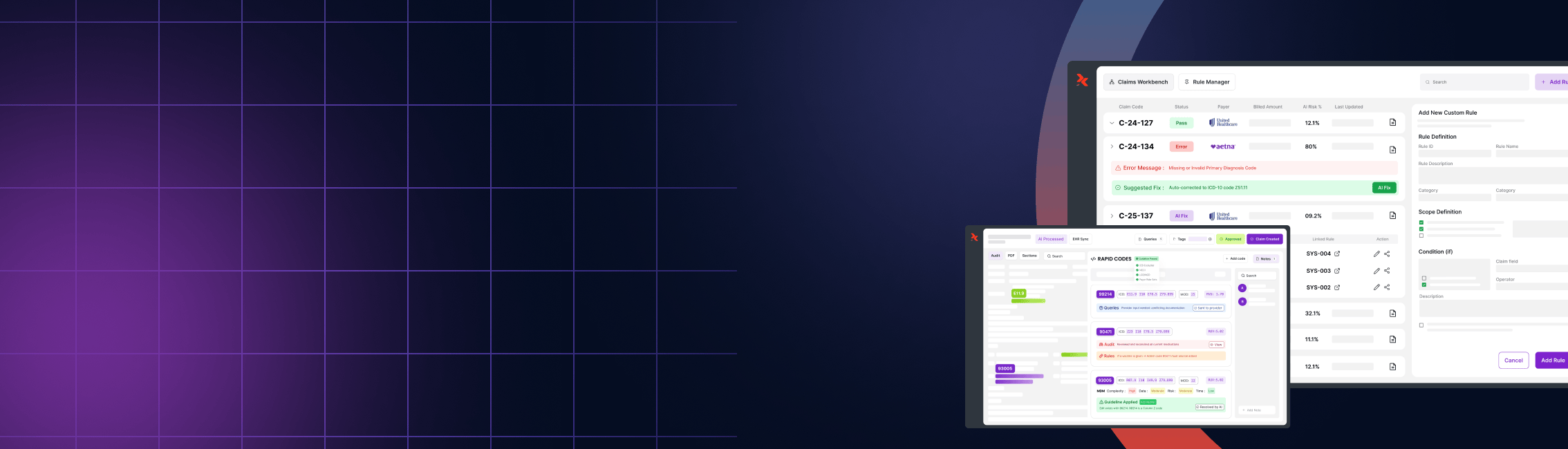
How AI is Transforming Medical Coding & Reducing Errors
The complexity of medical coding has grown with the increasing number of codes and the frequent updates to coding systems. Many healthcare providers are turning to AI-powered solutions like RapidClaims to reduce errors and improve efficiency.
AI tools can help by automating the coding process ensuring that the correct CPT and HCPCS codes are applied with every claim. These AI systems use machine learning algorithms to analyze medical records, identify the services rendered, and match them to the appropriate codes.
Some of the key benefits of AI in medical coding include:
- Improved Accuracy: AI reduces the risk of human error by automatically applying the correct codes based on the provided documentation.
- Faster Coding: AI systems can process codes faster than manual entry, leading to quicker claim submissions and improved cash flow.
- Up-to-date Compliance: AI platforms like RapidClaims are designed to keep up with the latest coding revisions, ensuring that your billing practices align with the current guidelines.
- Reduced Administrative Overhead: By automating routine tasks, AI frees up time for coders and billers to focus on more complex cases, improving overall efficiency.
Integrating AI into your coding process ensures accuracy, reduces administrative workload, and helps maintain compliance with evolving coding standards.
Conclusion
Understanding and properly applying CPT codes is crucial for effective medical billing. Whether you're dealing with evaluation and management codes, modifier codes, or HCPCS codes, accurate coding ensures that healthcare providers are reimbursed correctly and on time.
By staying up to date with the latest CPT codes, adhering to best practices, and utilizing tools like the CCI edit list, you can streamline the billing process and reduce the risk of claim denials.
Remember, CPT codes are more than just numbers—they represent the services provided, the level of care delivered, and, ultimately, the reimbursement that healthcare providers rely on. With the right tools, knowledge, and diligence, you can navigate the complexities of medical coding and ensure that your practice is operating efficiently and effectively.
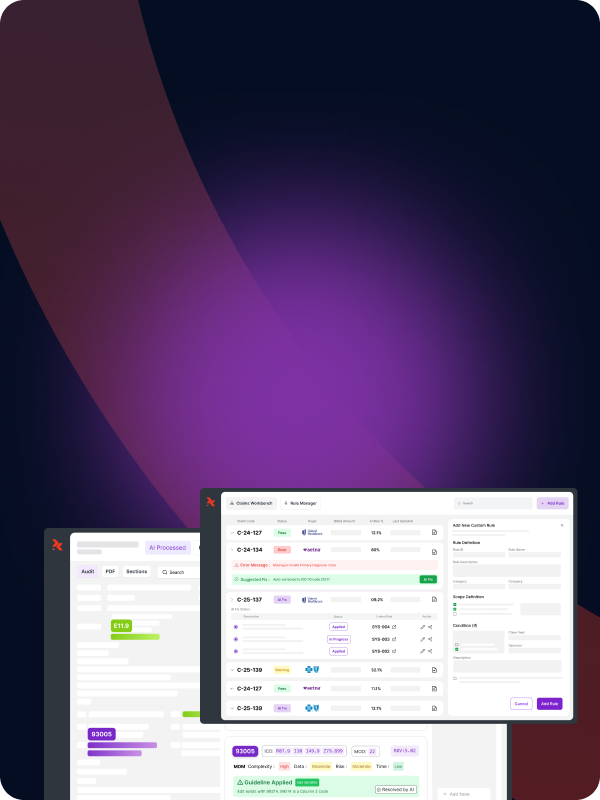
Optimize Your Coding Process with RapidClaims
At RapidClaims, we understand that accurate medical coding is the key to a smooth revenue cycle and faster reimbursements. Our AI-driven platform automates the medical coding process, ensuring precise CPT and HCPCS code assignments while reducing administrative costs and errors.
Transform your coding operations today with RapidClaims and unlock faster, more accurate reimbursements.
Ready to streamline your medical coding?
Get in touch with us for a demo and see how RapidClaims can revolutionize your billing process.
Frequently Asked Questions
1. What are CPT codes?
CPT (Current Procedural Terminology) codes are used to describe medical, surgical, and diagnostic procedures and services. These codes ensure that healthcare providers are reimbursed correctly for the services they render to patients.
2. What are HCPCS codes, and how do they differ from CPT codes?
HCPCS (Healthcare Common Procedure Coding System) codes are used to describe items and services not covered by CPT codes. These include medical supplies, durable medical equipment, transportation services, and certain drugs. HCPCS Level I codes are essentially the same as CPT codes, while HCPCS Level II codes cover non-physician services and supplies.
3. Why are CPT codes important for healthcare providers?
CPT codes are critical for accurate billing and reimbursement in healthcare. By correctly applying CPT codes, healthcare providers ensure they are reimbursed for the services they perform and that claims are processed efficiently by payers.
4. How can RapidClaims help with CPT and HCPCS coding?
RapidClaims uses AI-driven automation to streamline the medical coding process. By reducing manual efforts and minimizing human error, RapidClaims ensures that CPT and HCPCS codes are applied correctly, leading to faster claim processing and improved reimbursement accuracy.
5. What types of medical procedures are covered by CPT codes?
CPT codes cover various medical services, including office visits, surgeries, diagnostic tests, physical therapy, radiology procedures, etc. Each procedure or service is assigned a specific code for accurate billing.
6. How do modifier codes work in conjunction with CPT codes?
Modifier codes add more specific information to a CPT code. For example, Modifier 59 indicates that two procedures performed in the same visit are distinct and should be billed separately. RapidClaims automates the correct application of these modifiers, reducing the risk of billing errors.
7. What is the Correct Coding Initiative (CCI), and how does it relate to CPT codes?
The Correct Coding Initiative (CCI) is a program developed by Medicare to prevent improper coding and ensure correct billing. RapidClaims helps healthcare providers comply with CCI edits by automatically verifying CPT codes against the CCI edit list, preventing claim denials.
%201.png)