OB GYN CPT Codes: Guide to Gynecology Coding and Billing
.jpg)
Did You Know Incorrect OB/GYN Coding Costs U.S. Healthcare Billions Every Year?
In 2025, accurate obstetric and gynecologic CPT coding plays a crucial role in ensuring compliance, optimizing reimbursement, and supporting high-quality patient care. On January 1, 2025, the CMS implemented critical revisions to CPT codes, including the deletion of specific codes. Additionally, new codes such as 49186–49190 were introduced to classify excisions based on the total maximum length of tumors or cysts removed.
These changes highlight the need for precise coding in OB/GYN practices. This blog will explain OB GYN CPT codes and coding guidelines, offering clear insights into recent updates and practical strategies to handle this specialized area effectively.
TL;DR (Key Takeaways)
- OB GYN CPT codes ensure standardized documentation and accurate reimbursement.
- Five main categories cover E/M, surgical, radiology, lab/pathology, and medicine procedures.
- Modifiers and add-on codes document complexity and additional services to prevent denials.
- Regular updates from AMA and payers are essential for compliance and error reduction.
- Proper documentation of procedures, tests, and counseling is critical for correct code selection.
Table of Contents:
- What Are OB/GYN CPT Codes?
- 5 Primary Categories of OB/GYN CPT Codes
- Understanding Modifiers and Add-On Codes in OB/GYN Billing
- Best Practices for Accurate OB/GYN CPT Coding
- Conclusion
- FAQs
What Are OB/GYN CPT Codes?
OB GYN CPT codes are standardized numeric identifiers created by the American Medical Association (AMA) to represent medical, surgical, and diagnostic services in obstetrics and gynecology. They ensure uniform documentation and allow providers to report services for reimbursement accurately. These codes apply to everything from preventive gynecological visits to complex procedures such as hysterectomies and cesarean deliveries.
Key aspects of OB GYN CPT codes include:
- Uniform Reporting: Establishes a common language for documenting obstetric and gynecological services across healthcare systems.
- Accurate Reimbursement: Links clinical services directly to payments from Medicare, Medicaid, and private insurers.
- Comprehensive Coverage: Encompasses preventive exams, maternity care, imaging, surgical procedures, and fertility-related treatments.
- Audit Readiness: Meets CMS and payer requirements, reducing claim denials and compliance risks.
- Improved Records: Supports detailed and accurate patient documentation for better care continuity and reporting.
OB GYN CPT codes connect the clinical side of women’s healthcare with financial and administrative processes, making them indispensable for both practitioners and healthcare organizations.
5 Primary Categories of OB/GYN CPT Codes

OB/GYN CPT codes are broadly organized into categories that reflect the types of services provided in obstetrics and gynecology. For Medical Coders and Coding Managers, understanding these categories is critical to maintaining coding accuracy, ensuring compliance, and optimizing revenue. The five primary categories include:
1. Evaluation and Management (E/M) Codes
E/M codes represent services related to patient encounters such as office visits, preventive screenings, and counseling. In obstetric and gynecologic practice, these codes capture the complexity of care provided, ranging from routine wellness checks to detailed diagnostic consultations.
Below are a few E/M codes in OB/GYN practice:
- 99202–99215: Office visit codes for new or established patients, varying by visit duration, complexity, and decision-making level.
- 99384–99387: Preventive visits for new patients (ages 12–65+), covering comprehensive history, physical exam, risk assessments, and counseling.
- 99394–99397: Preventive visits for established patients (ages 12–65+), including wellness evaluations, risk-reduction strategies, and routine follow-ups.
- 99401–99404: Preventive counseling codes for interventions like contraception counseling, STI prevention, or reproductive health education.
- 81025: Urine pregnancy test (qualitative).
- 88164–88167: Laboratory screening codes for Pap smear and cervical cytology to detect precancerous or cancerous changes.
Note: Selection of the correct E/M code depends on patient status (new vs. established), visit type (problem-focused vs. preventive), and documentation of history, examination, and medical decision-making.
2. Surgical Procedure Codes
Surgery codes in OB/GYN CPT coding represent operative procedures performed in obstetrics and gynecology. These codes are particular, covering both the type of surgery and the approach used (e.g., abdominal, vaginal, or laparoscopic). They help ensure accurate billing and documentation of complex gynecologic interventions.
Common Examples of Gynecology Surgery CPT Codes:
- CPT 58150 (Hysterectomy): Total abdominal hysterectomy, including removal of the uterus and cervix.
- CPT 58570 (Laparoscopic Hysterectomy): Minimally invasive removal of uterus and cervix via laparoscopy.
- CPT 58956 (Oophorectomy): Surgical removal of one ovary (unilateral).
- CPT 58700 (Salpingectomy): Removal of one or both fallopian tubes.
- CPT 58353 (Endometrial Ablation): Destruction of the uterine lining using techniques such as thermal or radiofrequency energy.
- CPT 58140 (Myomectomy): Surgical removal of uterine fibroids while preserving the uterus.
- CPT 57421 (Cervical Biopsy): Removal of cervical tissue sample for diagnostic examination.
Surgery codes also extend to other procedures like colposcopy, dilation and curettage (D&C), and pelvic reconstructive surgeries. Correct usage of these codes is crucial to ensure compliance and avoid claim denials.
3. Radiology Codes
Radiology codes in OB/GYN CPT coding are used for diagnostic imaging studies that help evaluate reproductive health conditions. These codes vary depending on the imaging technique and the anatomical region being examined. Accurate use of radiology codes ensures proper documentation and reimbursement for essential gynecological diagnostic procedures.
Common radiology codes in gynecology include:
- CPT-76830 (Transvaginal Ultrasound): Represents an ultrasound of the female pelvis, focusing on the uterus, cervix, and ovaries. Commonly applied for evaluating uterine fibroids, ovarian cysts, or abnormal endometrial changes.
- CPT-74740 (Hysterosalpingography): An X-ray procedure performed after injecting contrast dye into the uterus to visualize the uterine cavity and fallopian tubes. It is often used in infertility evaluations to detect blockages or abnormalities in the fallopian tubes.
- CPT-72195 (MRI of Pelvis): Refers to magnetic resonance imaging of the pelvic region, including reproductive organs. Useful for identifying ovarian cancer, endometriosis, or advanced pelvic inflammatory disease.
- CPT-72193 (CT Scan of Pelvis): Specifies computed tomography imaging of the pelvis. Frequently used to evaluate pelvic masses, uterine fibroids, or staging of pelvic malignancies.
Radiology codes support gynecologists in diagnosing structural and pathological conditions, playing a critical role in both routine care and complex case management.
4. Laboratory and Pathology Codes
Laboratory and pathology codes in obstetric and gynecologic are used to document diagnostic tests and specimen studies that support accurate detection and treatment planning. These codes cover procedures such as pap smears, HPV testing, biopsies, and ultrasounds, ensuring providers can properly capture both preventive and diagnostic care.
Common Laboratory/Pathology CPT Codes in Gynecology:
- CPT-88141–88143 (Pap Smear): Reports the collection and cytologic evaluation of cervical or vaginal cells to detect abnormal changes.
- CPT-87624, 87625 (HPV Testing): Used for detecting high-risk human papillomavirus strains in women.
- CPT-87491, 87591, 87850, 87800 (Chlamydia & Gonorrhea Testing): Covers laboratory testing for sexually transmitted infections caused by chlamydia and gonorrhea.
- CPT-76856 (Pelvic Ultrasound): Imaging of the female pelvis, including uterus, ovaries, and adnexa, to assess structural or pathological conditions.
- CPT-58100, 58110, 58120 (Endometrial Biopsy): Involves tissue sampling from the uterine lining for histopathological analysis.
- CPT-58555, 58558 (Hysteroscopy): Diagnostic or operative procedure to visualize the uterine cavity using a hysteroscope, with or without additional interventions.
Note: Specific codes may vary depending on the exact test performed, payer rules, and documentation requirements.
5. Medicine Codes
Medicine codes in OB/GYN CPT coding represent diagnostic, surgical, and therapeutic procedures specific to gynecology. These codes ensure accurate billing, streamline documentation, and support proper reimbursement for specialized medical services.
Examples of Medicine-Related OB GYN CPT Codes:
- Colposcopy Procedures:
- CPT-57420: Colposcopy of the cervix, including biopsy or endocervical curettage
- CPT-57454: Colposcopy of the vulva with biopsy
- CPT-57460: Colposcopy of the vulva with destruction of lesion(s)
- Intrauterine Device (IUD) Procedures:
- CPT-58300: Insertion of intrauterine device (IUD)
- CPT-58301: Removal of intrauterine device (IUD)
- Hysteroscopy Procedures:
- CPT-58555: Hysteroscopy, surgical; removal of impacted foreign body
- CPT-58558: Hysteroscopy, surgical; endometrial biopsy and/or polypectomy, with or without D&C
- CPT-58563: Hysteroscopy, surgical; removal of leiomyomata (fibroids)
- Laparoscopic Procedures:
- CPT-58605: Laparoscopy, surgical; fulguration or excision of ovarian or pelvic lesions
- CPT-58661: Laparoscopy, surgical; removal of adnexal structures (tubes or ovaries)
- Obstetric Monitoring:
- CPT-58970: Fetal monitoring, non-stress test
CPT codes are updated annually by the AMA, and payers may enforce specific rules for reimbursement. Accurate code selection, aligned with patient documentation and medical necessity, is essential for compliance. Integrating RapidClaims with your EHR system can simplify CPT coding, minimize errors, and improve claim accuracy. This allows healthcare teams to focus on patient care while enhancing workflow efficiency.
Understanding Modifiers and Add-On Codes in OB/GYN Billing
Modifiers and add-on codes are part of the CPT coding system, providing additional details or reporting extra services. They clarify the nature, extent, or timing of a procedure, ensuring accurate billing, proper reimbursement, and compliance with payer requirements. For Medical Coders and Coding Managers, understanding and applying these correctly is critical:
Common Modifiers in OB/GYN Billing:
- 25: Indicates a significant, separately identifiable evaluation and management (E/M) service performed on the same day as another procedure. This helps differentiate the E/M service from the primary procedure for accurate reimbursement.
- 59: Denotes a distinct procedural service, used when procedures that are typically bundled are performed separately, such as two unrelated surgeries during the same session.
- 62: Used when two surgeons are involved in a procedure, typically for complex surgeries requiring specialized expertise.
- 78: Represents an unplanned return to the operating or procedure room for a related procedure during the postoperative period, ensuring that follow-up procedures are appropriately documented and reimbursed.
Example: A patient undergoes both a cervical biopsy (CPT-57421) and an endometrial biopsy (CPT-58100) during the same visit. Modifier 59 is added to one code to show the procedures are separate and not bundled.
Common Add-on Codes:
- +99354–99357: Applied for prolonged evaluation and management services when the time spent with the patient exceeds the typical E/M service.
- +99368–99372: Covers non-face-to-face prolonged E/M services, such as reviewing complex records or coordinating care outside the patient encounter.
- +99415–99416: Used for non-face-to-face prolonged preventive services, including extended counseling or preventive care planning.
Example: A gynecologist spends 45 extra minutes with a patient discussing complex fertility treatment; +99354 is added to the standard office visit CPT code.
Proper use of modifiers and add-on codes ensures clear billing, prevents claim denials, and maintains compliance with AMA and payer rules. These codes also capture the complexity and time involved in OB/GYN services. RapidClaims enhances this process by cross-referencing HCPCS, ICD-10, and CPT codes. This integration improves coding accuracy, minimizes denials, and streamlines reimbursement.
Best Practices for Accurate OB/GYN CPT Coding
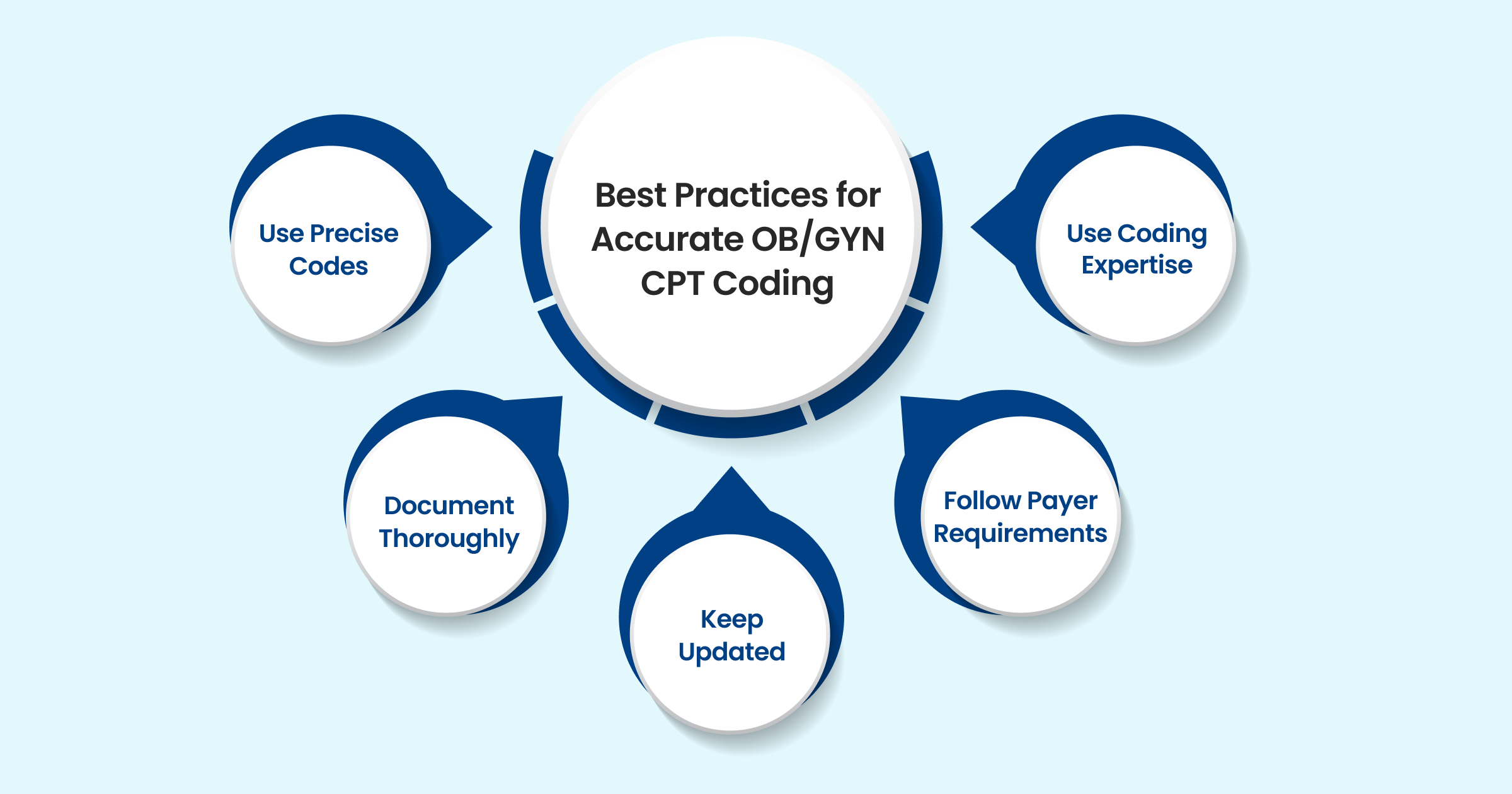
Accurate OB/GYN coding ensures compliance with regulatory requirements and proper reimbursement for services. Mistakes in code selection or documentation can lead to claim denials, delayed payments, and potential audits. With CPT updates in 2025 and evolving payer rules, maintaining precision is essential for both clinical and administrative accuracy.
Below are key strategies to ensure accurate coding:
- Use Precise Codes: Apply the CPT code that directly corresponds to the procedure or service performed, including any applicable modifiers.
- Document Thoroughly: Capture all clinical details, such as patient history, examination findings, procedures, and counseling, to support code selection.
- Keep Updated: Regularly review AMA CPT revisions and payer-specific policy changes to ensure codes are current.
- Follow Payer Requirements: Check insurer-specific rules, pre-authorization needs, and coverage guidelines to minimize denials.
- Use Coding Expertise: Employ certified coders or perform periodic audits to maintain accuracy and optimize revenue cycle management.
Implementing best practices in OB/GYN coding can be further supported by automation tools. RapidClaims offers AI-powered tools: RapidCode for fully automated coding, RapidAssist to support coders with AI recommendations, and RapidRisk for risk-adjusted coding to optimize reimbursements. The platform ensures accurate CPT coding and seamless EHR integration, helping practices maintain compliance, reduce errors, and improve revenue cycle efficiency.
Also Read: Intro to Commonly Used Medical CPT/HCPCS Codes List.
Conclusion
Accurate CPT coding is vital for OB/GYN practices to ensure proper reimbursement and compliance with regulations. Correct code application streamlines billing, reduces errors and denials, and supports efficient practice operations. Staying updated with coding changes, payer rules, and professional guidelines is essential to maintain accuracy in OB/GYN billing.
RapidClaims simplifies complex coding workflows with features like real-time code validation, predictive search, and seamless EHR integration. Its AI-powered tools help ensure accuracy, reduce errors, and keep practices compliant with evolving CPT and insurance guidelines.
Want to improve the efficiency and precision of OB/GYN CPT code management? Request a Free Demo today to see how RapidClaims can streamline your coding process and optimize your billing operations.
Frequently Asked Questions (FAQs)
1. Can I bill for a preventive visit and a procedure on the same day?
Yes, but only if the evaluation and management (E/M) service is significant and separately identifiable from the procedure. Use modifier 25 to indicate this distinction. Proper documentation of both services is required to avoid claim denials.
2. Can an IUD insertion and removal be billed in the same patient visit?
Yes, each service has a distinct CPT code: CPT-58300 for insertion and CPT-58301 for removal. Ensure documentation clearly shows that both procedures were performed and medically necessary.
3. Can telehealth visits for OB/GYN services be coded using standard E/M codes?
Yes, telehealth visits may use standard E/M codes if guidelines for telemedicine are followed. Payer-specific modifiers and documentation of virtual services are required for accurate reimbursement.
4. Can I bill for both a Pap smear and an HPV test on the same visit?
Yes, but use separate CPT codes: CPT-88141–88143 for Pap smear and CPT-87624 or 87625 for HPV testing. Document each test clearly to support medical necessity.
5. Can a hysteroscopy be coded with other procedures performed in the same session?
Yes, but only if each procedure is distinct and medically necessary. Use add-on codes or modifiers to indicate separate services and avoid claim denials.
6. Can E/M codes be billed for postpartum visits after a cesarean section?
Yes, postpartum visits are billable using standard E/M codes. Documentation should reflect patient status, evaluation, and any complications for proper reimbursement.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






