A Complete Overview of Medical Coding Modifiers

Could one simple modifier be the difference between a claim being accepted or rejected? Medical coding modifiers play a crucial role by providing the clarity and detail needed to ensure claims are processed correctly. For medical coders, billing teams, and revenue cycle management (RCM) professionals, becoming proficient in the use of these modifiers is critical to ensuring accurate reimbursements and minimizing costly claim denials. Without modifiers, the billing process would lack the required precision for accurate reimbursements.
But what exactly are medical coding modifiers, and how do they impact the medical billing process? In this blog, we'll explore their purpose, types, and common uses, and explain why correct application is essential for healthcare providers and medical coders.
What Are Medical Coding Modifiers?
Medical coding modifiers are additional codes added to primary procedure codes to provide more detailed information. They clarify the circumstances under which a service was provided or highlight special conditions during a procedure. Modifiers help refine the meaning of a service without changing the code's primary description. This allows healthcare providers to report services accurately, improving reimbursement outcomes and reducing claim denials.
How do Medical Coding Modifiers Work?
A medical coding modifier is a two-character code, either letters or numbers, added to a CPT or HCPCS Level II code. It provides extra details about the medical procedure, service, or supply without changing the original code’s meaning. Medical coders use these modifiers to accurately describe a specific encounter.
For example, a coder might use a modifier to show that a service wasn’t performed exactly as described by a CPT or HCPCS Level II code, but the correct code still applies. Modifiers can also add extra details that aren’t in the code description, like the location of the procedure. Here are a few situations where a modifier may be necessary:
- When a service or procedure involves both professional and technical components.
- If multiple providers perform a service or procedure.
- When a service or procedure occurs in multiple locations.
- If the procedure is either increased or reduced compared to the typical requirements for the code.
- If the procedure is bilateral.
- When a service or procedure is provided to the patient more than once.
Accurate use of modifiers is essential for correct coding, as some modifiers impact reimbursement. Failing to apply the right modifiers or omitting them altogether can lead to claim denials, delays in payment, or even loss of reimbursement.
CPT and HCPCS Level II Modifiers
Modifiers are classified into two main categories: CPT and HCPCS Level II modifiers. These modifiers provide essential details that help clarify procedures, ensuring proper reimbursement and correct claim processing under established guidelines.

1. CPT Modifiers
The American Medical Association (AMA) provides CPT modifiers, which are two-digit codes used alongside the main CPT codes, to provide more specific information about the service or procedure being performed. These modifiers help clarify situations such as unusual circumstances, multiple procedures, or special conditions that affect how a service is billed and reimbursed. In some cases, these modifiers are alphanumeric when applied to performance measures for CPT Category II codes (e.g., 1P-8P).
2. HCPCS Level II Modifiers
HCPCS Level II modifiers are either alphanumeric or consist of two letters. These modifiers provide additional details about a service or procedure, such as where it was performed or any special conditions that affected the treatment. They help ensure that insurers process claims correctly, particularly in accordance with the guidelines set by the Centers for Medicare & Medicaid Services (CMS).
Both CPT and HCPCS Level II modifiers play a crucial role in providing detailed information for accurate billing and reimbursement and ensuring proper claim processing under specific guidelines.
Common Medical Billing Modifiers and Their Applications
Different medical procedures require specific modifiers to ensure accurate reporting and processing of claims. Below are a few of the most commonly used modifiers:

1. Telemedicine and Virtual Care
- GQ (Via asynchronous telecommunications system): Used to indicate that a service was provided using an asynchronous telecommunications system, commonly used in telemedicine.
- GT (Via interactive audio and video telecommunications): Indicates that a service was provided using interactive audio and video telecommunications, typically used for telemedicine consultations.
- G0 (Telehealth services): Denotes telehealth services provided during the COVID-19 pandemic; this modifier helps specify telemedicine claims in the context of emergency procedures.
2. Global Modifiers
- 24 (Unrelated E&M service by the same physician during a post-operative period): This modifier is used when an evaluation and management service is provided by the same physician during the post-operative period for a condition unrelated to the surgery.
- 27 (Multiple outpatient hospital E&M services on the same date): This modifier applies when multiple outpatient evaluation and management services are provided by the same physician to a patient on the same date.
- 52 (Reduced services): This modifier is used when a service is partially reduced or eliminated at the physician’s discretion.
- 59 (Distinct procedural service): Indicates that two procedures were performed on the same day but were distinct and separate from each other.
- 76 (Repeat procedure by the same physician): This modifier is used when the same procedure is repeated by the same physician.
- 77 (Repeat procedure by a different physician): Indicates a repeated procedure performed by a different physician.
3. Procedure-Specific Modifiers
- 22 (Increased procedural services): This modifier is applied when the procedure performed is more complex than usual, requiring extra time or effort.
- 29 (Unlisted procedure, services): It is used for procedures not specifically listed in CPT codes.
- 50 (Bilateral procedure): Indicates that a procedure was performed on both sides of the body.
- 51 (Multiple procedures): Indicates that more than one procedure was performed during the same session, highlighting multiple distinct services.
- 53 (Discontinued procedure): Indicates a procedure that was terminated before completion due to unexpected circumstances or patient condition.
4. Anatomical and Site-Specific Modifiers
- E1 (Upper left eyelid): This modifier is used to specify the upper left eyelid in the context of a procedure.
- TC (Technical component): Refers to the technical portion of a service or procedure which includes equipment, technician time, and other costs.
- XS (Separate structure): Used to indicate that the services performed were separate and distinct from the primary procedure, typically used in situations involving multiple anatomical locations.
This categorization provides clarity on when each modifier is most applicable in medical coding, ensuring the accurate representation of services performed during medical treatments.
Also Read: RapidCode and RapidAssist: The Dynamic Duo in Healthcare Coding Software
Functions and Importance of Modifiers in Billing
Medical coding modifiers are essential tools that enhance the clarity and accuracy of healthcare billing. For healthcare professionals, medical coders, revenue cycle managers, and compliance officers, these modifiers serve an important role in ensuring that services are billed correctly and reimbursements are processed smoothly. Here's why they matter:

- Clarifying Special Conditions: Modifiers are used to explain special situations, like when a procedure is more complex than usual or when multiple procedures are done during the same visit. This additional detail ensures the proper classification and reimbursement of the service.
- Ensuring Accurate Reimbursement: By providing more specifics, modifiers ensure that payers clearly understand the service provided, reducing the chances of denied claims. This leads to more accurate and timely reimbursements for the healthcare provider.
- Enhancing Billing Efficiency: Modifiers allow you to convey important information in a concise manner, eliminating the need for lengthy explanations. This speeds up the claims process and helps maintain cash flow.
- Supporting Compliance: Proper use of modifiers is essential for meeting coding standards and regulations. By following guidelines correctly, healthcare providers can avoid compliance issues and costly audits.
Streamline your medical coding and billing process with RapidClaims, an AI-powered automation platform that cuts down administrative costs and improves reimbursement processes. Designed to integrate seamlessly with hospitals, physician groups, and billing companies, RapidClaims enhances workflows, ensures compliance, and accelerates revenue cycles. Transform your medical billing operations today!
Modifier Usage in Complex Service Scenarios
Certain scenarios in medical billing require careful application of modifiers. Here are a few common scenarios where modifiers are used:

1. Service Involving Professional and Technical Components: When a service includes both professional and technical components (e.g., a diagnostic procedure), modifiers differentiate between the two.
- Modifier -26: Applied to the professional component (e.g., physician’s interpretation).
- Modifier -TC: Used for the technical component (e.g., equipment or staff performing the service).
2. Unplanned Return to the Operating Room: When a patient must return to the operating room due to complications during the post-operative period, a modifier is needed to explain the situation.
- Modifier -78: Indicates an unplanned return to the operating room within the global period for a related procedure.
3. Staged or Related Procedures During the Post-Op Period: If additional procedures are necessary during the post-operative period, modifiers clarify the relationship between the initial and subsequent procedures.
- Modifier -58: This modifier is used for staged or planned procedures during the post-op period. These procedures are usually anticipated and scheduled as part of the initial treatment.
4. Unrelated Procedure During Post-Operative Period: If an unrelated procedure is performed during the global period following surgery, modifiers help ensure separate billing.
- Modifier -79: Applied when a new, unrelated procedure occurs during the post-op period.
5. Professional vs. Technical Reimbursement: In cases where both professional and technical components are billed together, modifiers are essential to ensure appropriate reimbursement for each part.
- Modifier -25: This is used when a doctor does a check-up (E/M service) on the same day as another procedure, but the check-up was separate and important enough to bill on its own. It helps make sure both the check-up and the procedure are reimbursed.
6. Service or Procedure for Non-Standard Circumstances: Modifiers are needed for clarity in certain situations, such as procedures that occur outside the typical settings or conditions.
- Modifier -23: Indicates that an anesthesia service was performed under unusual circumstances, such as extreme patient anxiety or other significant factors that increased the complexity.
Ensure your medical coding modifiers stay accurate and fully compliant with RapidClaims. Our AI-assisted platform automatically updates and verifies codes, using built-in rule sets that align with HIPAA and CMS guidelines. With continuous compliance and automated updates, RapidClaims helps you minimize errors and prevent claim denials.
Also Read: Evaluation and Management in Medical Coding Guide.
Usage Guidelines and Documentation
Medical coding modifiers are essential for accurate billing and claims processing. To ensure proper use, it’s important to follow established guidelines and best practices. Below are the key points to consider:
- Know the Modifier Codes: Each modifier has specific uses, so it’s critical to understand when and how to apply them.
- Review the Guidelines Regularly: Modifier rules can change. Stay updated with the latest coding manuals and payer-specific guidelines.
- Apply Modifiers Correctly: Only use a modifier when necessary, ensuring it accurately reflects the service provided.
- Document the Reasoning: Always document why a modifier was applied. This helps prevent claim denials and ensures reimbursement accuracy.
- Follow Payer Policies: Different insurance companies may have distinct requirements for modifier usage. Always refer to their policies to avoid errors.
By following these guidelines, you can ensure that medical procedures are coded accurately, improving reimbursement outcomes and reducing the risk of claim denials.
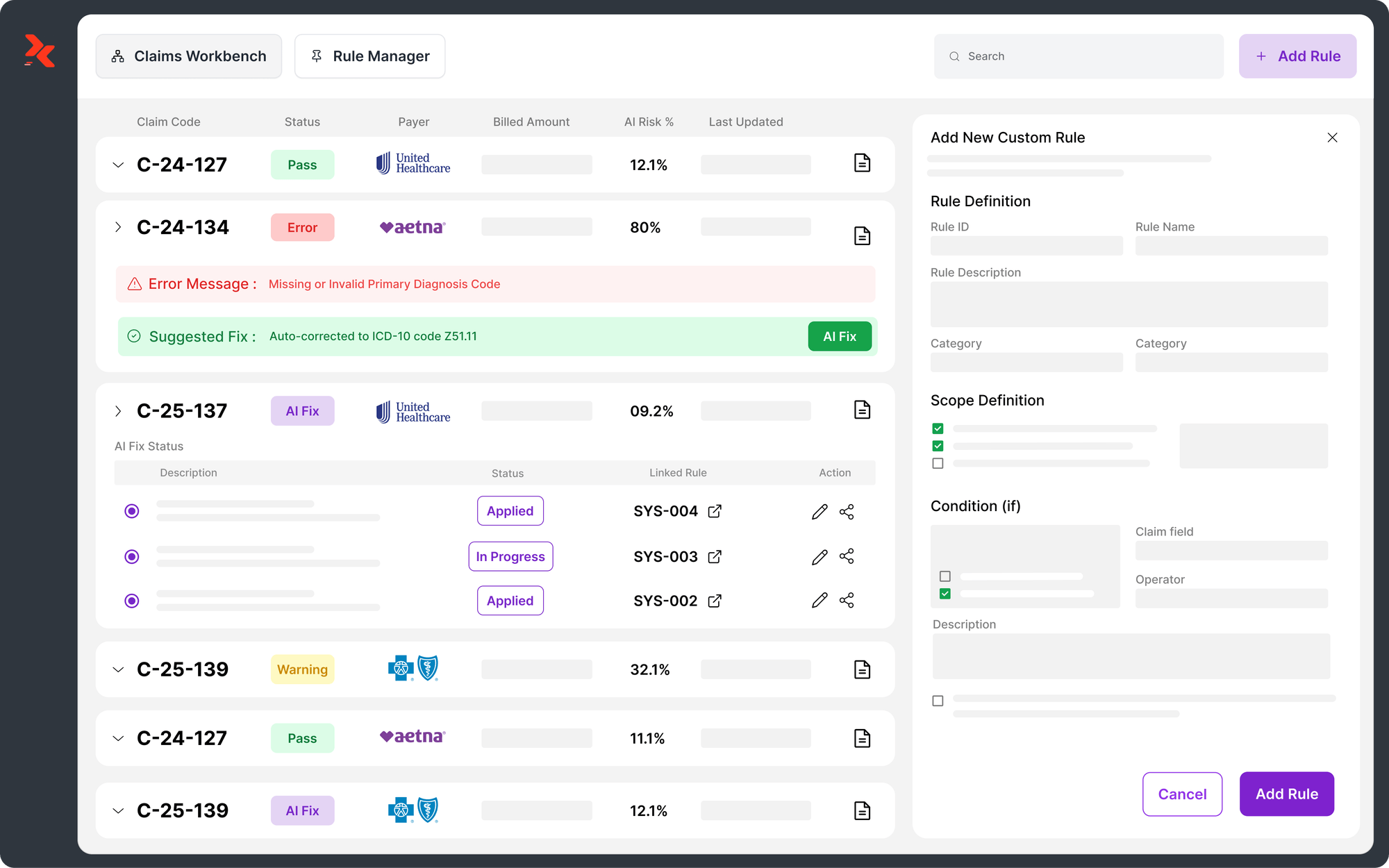
RapidClaims: Streamlining Medical Coding Modifiers with AI-Driven Automation

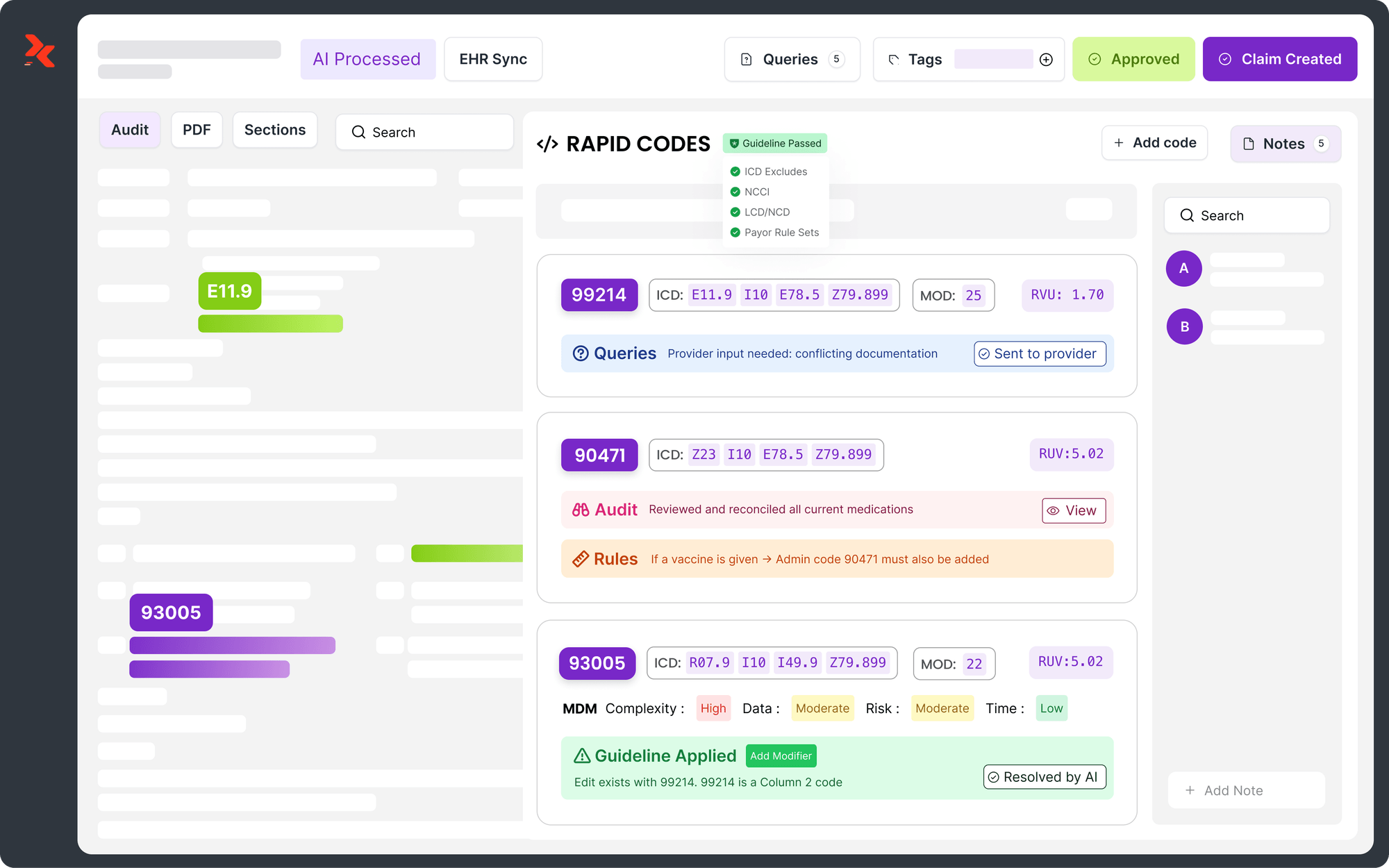
RapidClaims is an AI-driven automation platform that streamlines medical coding operations and ensures accurate modifier application through its RapidScrub module. Unlike traditional scrubbers, RapidScrub utilizes over 119 million pre-submission edits, continuously updated with the latest payer rules, to predict and prevent denials before submission. This proactive approach enables cleaner claims and maximizes reimbursement instantly.
Types of Medical Coding Handled by RapidClaims
Below are the key coding types that RapidClaims handles, ensuring comprehensive coverage across multiple healthcare settings:
- ICD (Diagnosis Coding): Used for disease classification, risk assessment, and patient conditions.
- CPT (Procedure Coding): Medical, surgical, and diagnostic procedure codes for billing.
- E&M (Evaluation & Management): Determines reimbursement levels for patient visits based on complexity.
- HCC (Risk Adjustment Coding): AI-optimized risk-adjusted coding for Medicare Advantage and other payers.
- HCPCS (Medicare & Medicaid Coding): Covers outpatient services, ambulance billing, and durable medical equipment (DME).
The RapidClaims platform seamlessly integrates with hospitals, physician groups, medical billing companies, and ACOs. It provides automated coding, AI-assisted workflow optimization, and real-time insights to reduce claim denials and speed up revenue cycles.
Conclusion
Medical coding modifiers are a vital part of the billing process. They provide crucial information about the service, improve reimbursement, and reduce claim denials. Accurate modifier usage is essential for healthcare providers to receive appropriate payment for their services.
Implementing platforms like RapidClaims enhances the accuracy and efficiency of modifier usage. Its AI-driven platform automates modifier application, reducing errors, accelerating claims processing, and ensuring proper reimbursement. By streamlining the coding process, RapidClaims allows healthcare providers to focus more on patient care while minimizing administrative burden.
Schedule a Free Demo today to see how RapidClaims can transform your billing operations.
FAQs
1. How do modifiers help medical providers avoid underpayment for bundled services?
Modifiers prevent underpayment by ensuring that each service, even if part of a bundled procedure, is accounted for correctly. For example, when multiple services are performed but billed under a single code, modifiers such as 59 help separate these services, ensuring fair reimbursement for each action taken.
2. How do modifiers help address billing for multi-phase treatments, like chemotherapy cycles?
Modifiers help coders handle multi-phase treatments like chemotherapy by specifying the distinct phases of care. For instance, modifier 59 is used to separate distinct services performed on the same day but as part of different phases of treatment. This ensures each treatment phase is reimbursed appropriately.
3. How do modifiers help in coding for experimental or non-standard procedures?
Modifiers allow coders to accurately describe experimental, investigational, or non-standard procedures. By using the correct modifier, providers can ensure that these unique services are properly identified, coded, and reimbursed, while also meeting regulatory requirements.
4. How do modifiers impact reimbursement for preventive care versus therapeutic services?
Modifiers like 33 for preventive services and 25 for significant, separately identifiable services help differentiate between preventive and therapeutic services. This distinction is crucial for insurance providers to ensure that preventive services, such as screenings or vaccinations, are reimbursed without the patient incurring additional costs.
5. How do modifiers address billing for services that involve both inpatient and outpatient care?
Modifiers are key in distinguishing services provided in both inpatient and outpatient settings. Modifiers such as 25 (significant, separately identifiable E&M service) and 56 (preoperative management) help ensure that the distinction between inpatient and outpatient services is clear, leading to proper billing and reimbursement.
6. Why are modifiers important when coding for experimental or off-label drug treatments?
For treatments involving experimental drugs or off-label uses, modifiers allow healthcare providers to code these services with the necessary clarity. This ensures that insurers understand the unique nature of the treatment and can process claims accurately, even if the treatment is not widely covered.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products
%201.png)


.jpg)