.webp)
Difference Between ICD-10-PCS and CPT Codes Simplified


Accurate medical coding is essential for proper billing, compliance, and reimbursement. ICD-10-PCS and CPT codes serve distinct but complementary purposes, enabling healthcare professionals to document procedures correctly and avoid claim denials.
In 2024, CMS added 41 new ICD-10-PCS procedure codes to improve inpatient documentation accuracy. At the same time, CPT codes expanded to include telehealth services, reflecting the growing role of remote care. These updates highlight the importance of staying current with coding changes to ensure accurate claims and reimbursements.
In this blog, you will learn about the key differences between ICD-10-PCS and CPT codes, their primary use cases, and how they work together to ensure accurate billing.
TL;DR (Key Takeaways)
- ICD-10-PCS codes document inpatient hospital procedures with high specificity, while CPT codes capture outpatient, physician, and ancillary services.
- Both code sets have distinct structures, update schedules, and documentation requirements that impact compliance, audits, and reimbursement.
- Accurate coding affects revenue cycle performance because ICD-10-PCS influences DRG payments and CPT determines individual service reimbursement.
- Understanding how ICD-10-PCS and CPT codes work together ensures a complete and auditable record of all services rendered.
- Following best practices, including dual expertise, update tracking, enhanced documentation, technology use, and audits ensures accuracy and optimized revenue.
Table of Contents:
- What are ICD-10-PCS Codes?
- What are CPT Codes?
- Key Differences Between ICD-10-PCS and CPT Codes
- How do ICD-10-PCS and CPT Codes Work Together?
- Importance of Accurate ICD-10-PCS and CPT Coding in Healthcare
- Common Challenges in ICD-10-PCS and CPT Coding
- Best Practices for ICD-10-PCS and CPT Coding
- Conclusion
- Frequently Asked Questions (FAQs)
What are ICD-10-PCS Codes?
ICD-10-PCS Codes are a standardized system used in the United States to document inpatient hospital procedures for medical billing, reporting, and statistical purposes. Unlike ICD-10-CM codes, which classify diagnoses, ICD-10-PCS focuses exclusively on procedures performed during hospital stays. The CMS maintains them and they are essential for accurate reimbursement under the inpatient prospective payment system (IPPS).
Key points:

- Purpose: Captures detailed procedural information for inpatient services to ensure accurate billing and compliance.
- Scope: Only used for inpatient hospital procedures; outpatient procedures are typically coded using CPT.
- Granularity: Provides high specificity, detailing precisely what was done, how, and where, which improves data quality and reduces claim denials.
Example: A code like 0FB03ZX might represent a removal of a heart valve via an open approach, with each character indicating a component such as the root operation (removal), body part (heart valve), and approach (open).
What are CPT Codes?
CPT Codes (Current Procedural Terminology codes) are a standardized set of codes to describe medical, surgical, and diagnostic services performed by healthcare providers. Unlike ICD-10-PCS, which is specific to inpatient hospital procedures, CPT codes are primarily used for outpatient services, physician services, and ancillary care. The AMA maintains them and are essential for accurate billing, reimbursement, and documentation of healthcare services.
Key Points:
- Purpose: CPT codes allow providers, payers, and auditors to document and communicate the exact services rendered for billing and compliance.
- Scope: Used for outpatient, physician, and ancillary services, including office visits, lab tests, imaging, surgeries, and telehealth services.
- Categories:
- Category I: Standard procedures and services.
- Category II: Performance Measurement Tracking (Optional).
- Category III: Emerging technologies and experimental procedures.
Example: A code like 99213 represents a level 3 office visit for an established patient, indicating the complexity and time spent during the consultation.
Accurate CPT coding is critical not only for compliance but also for optimizing revenue and reducing claim denials. Advanced coding platforms, like RapidClaims, utilize machine learning to automate CPT coding, improve accuracy, and accelerate revenue capture. Such systems can boost coder productivity by over 150% and reduce claim denials by 40%, ensuring CPT codes are applied consistently across outpatient services.
Key Differences Between ICD-10-PCS and CPT Codes
ICD‑10‑PCS and CPT codes are both essential for billing, but they serve distinct roles in documentation, revenue cycle management, and audit compliance. Understanding their differences helps coders, compliance officers, and revenue cycle managers ensure accurate claims processing and proper reimbursement.
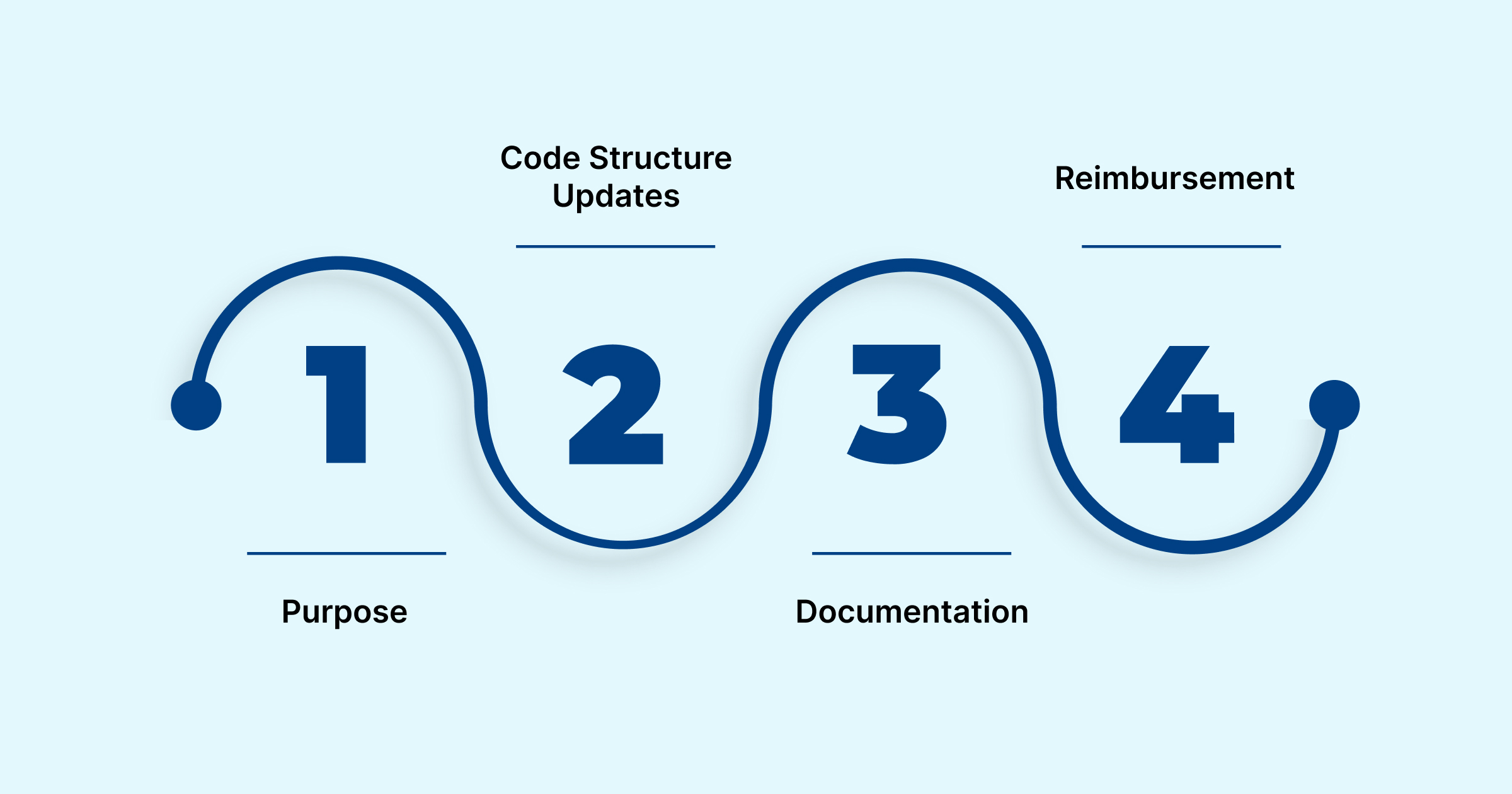
1. Purpose: Inpatient Procedure vs. Service/Procedure
The most significant difference between ICD‑10‑PCS and CPT codes lies in what they represent.
- ICD‑10‑PCS: Focus on inpatient procedures, capturing exactly how and why a procedure was performed during a hospital stay.
For example, 027034Z represents dilation of one coronary artery via a percutaneous approach, without a device, providing a highly detailed procedural description.
- CPT Codes: Describe services and procedures delivered in both inpatient and outpatient settings, including diagnostic tests, therapeutic interventions, and treatments.
For example, 92928 represents a percutaneous coronary intervention with a stent, emphasizing the service rendered rather than the granular procedural details.
2. Code Structure and Update Schedules
Both code sets have unique structures and update schedules that coders must manage to ensure compliance and readiness for audits.
- ICD‑10‑PCS: Each ICD-10-PCS code is 7 alphanumeric characters, with each character representing a specific aspect of the procedure (e.g., section, body system, root operation, body part, approach, device, qualifier).
Updates: ICD-10-PCS codes are updated annually, typically taking effect on October 1, with additional updates sometimes implemented on April 1. These updates follow CMS proposals and stakeholder feedback, ensuring that coding remains current and aligned with clinical practice. For details, refer to this Official ICD-10-PCS Update Document.
- CPT Codes: These codes are five numeric characters, sometimes with modifiers to provide additional details (e.g., bilateral procedures, increased complexity).
Updates: CPT codes are updated annually, with new codes, revisions, and deletions published by the AMA, typically taking effect January 1 each year.
3. Documentation: Hospital Record vs. Billing Claim
The timing and application of each code type differ significantly:
- ICD‑10‑PCS: Serves as a detailed record of inpatient procedures, providing evidence for internal and external audits. They support compliance with federal regulations and validate clinical decision-making.
- CPT Codes: Creates a clear paper trail for services delivered, linking clinical actions to reimbursement claims. Proper documentation ensures clarity in payer reviews, reduces claim denials, and supports post-payment audits.
Accurate documentation in both code sets helps coders track workflow, coordinate between departments, and maintain completeness of the medical record, which is critical for both revenue integrity and regulatory compliance.
4. Reimbursement: DRG Assignment vs. Payment Determination
Each code type impacts reimbursement differently:
- ICD‑10‑PCS: Directly influences DRG assignment, which in turn affects bundled hospital payments and overall inpatient reimbursement. Accurate procedural coding ensures correct revenue capture, minimizes audit risk, and supports compliance with federal and payer regulations.
- CPT Codes: Determine individual service payments, detailing what the healthcare provider is reimbursed for each procedure, intervention, or therapy session. Proper CPT coding ensures precise billing, reduces claim denials, and facilitates smoother payer adjudication.
In addition to purpose, structure, documentation, and reimbursement, there are several other distinctions that coders and revenue cycle managers should note. The table below highlights these differences, providing a clear snapshot of audit readiness and billing:
Accurately coding ICD‑10‑PCS and CPT is challenging due to documentation gaps, frequent updates, and manual processes that slow revenue cycles. RapidClaims uses AI to automate coding, denial prevention, and clinical documentation integrity. RapidCode delivers 96 % accuracy, RapidScrub cuts denials by 40 %, and RapidCDI improves HCC capture, enhancing clean‑claim rates and optimizing revenue with measurable ROI in under 30 days.
How do ICD-10-PCS and CPT Codes Work Together?
In practice, both coding systems often appear on claims: ICD-10-PCS for inpatient procedures, and CPT for ancillary outpatient services or related reporting. For instance, consider a patient admitted for cardiac bypass surgery, coded with the appropriate ICD-10-PCS code that reflects the surgical procedure. Post-op physical therapy or diagnostic imaging rendered during the admission might be coded separately using CPT codes.
This interplay illustrates the difference between ICD-10-PCS and CPT codes: one captures the procedural detail core to inpatient treatment, the other covers additional services that may be billed separately. Together, they form a comprehensive coding narrative for audit, billing, and clinical documentation.
Importance of Accurate ICD-10-PCS and CPT Coding in Healthcare

Accurate application of both ICD-10-PCS and CPT codes is critical for multiple aspects of healthcare operations:
- Revenue cycle efficiency: Precise coding minimizes claim denials, reduces resubmissions, and accelerates reimbursement. ICD-10-PCS ensures inpatient procedures are fully captured, while CPT codes document ancillary and physician services, preventing gaps that often trigger payer rejections.
- Audit resilience and compliance: Linking ICD-10-PCS and CPT codes with patient records and clinical documentation strengthens defensibility during internal and external audits. Proper use demonstrates adherence to CMS and HIPAA standards, reducing the risk of penalties and post-payment reviews.
- Data analytics and quality metrics: ICD-10-PCS provides granular insight into inpatient procedures, enabling hospitals to monitor trends, track outcomes, and optimize resource allocation. CPT codes support service utilization analysis and benchmarking for physician performance, telehealth adoption, and preventive care measures.
Understanding the differences between ICD-10-PCS and CPT codes enables healthcare stakeholders to maintain accurate documentation, streamline billing processes, and enhance reporting accuracy throughout the revenue cycle.
Common Challenges in ICD-10-PCS and CPT Coding
Healthcare professionals encounter several challenges when working with ICD-10-PCS and CPT codes:
- Coding complexity: ICD-10-PCS contains tens of thousands of codes with multiple axes, requiring precise selection to represent the procedure performed accurately.
- Synchronization of updates: CPT and ICD-10-PCS have overlapping but distinct update cycles, which can result in temporary misalignments in EHR systems, training, or workflow protocols.
- Documentation gaps: Incomplete or unclear clinical documentation increases the risk of coding errors, which can lead to claim denials or compliance issues.
- Compliance demands: Both code sets must adhere to HIPAA, CMS, and payer-specific regulations, necessitating continuous education and vigilance from coders and clinicians.
By understanding these challenges, healthcare teams can reduce coding errors and enhance accuracy. Next, we’ll review best practices for ICD-10-PCS and CPT coding to ensure compliance and optimize workflows.
Best Practices for ICD-10-PCS and CPT Coding

Implementing best practices in ICD-10-PCS and CPT coding is essential for accuracy, compliance, and efficient revenue cycle management. By establishing clear processes and utilizing available tools, healthcare organizations can minimize errors, streamline workflows, and ensure proper reimbursement.
To put these strategies into action, consider the following key practices:
1. Maintain Dual Expertise
Coders should be fully proficient in the structure and logic of both ICD-10-PCS and CPT. Understanding procedural definitions, code axes, and system-specific rules is critical for accurate inpatient and outpatient coding.
2. Track Update Cycles
CPT is revised annually, while ICD-10-PCS updates occur in April and October. Proactively monitoring these schedules allows timely system updates, staff training, and workflow adjustments to prevent coding gaps or errors.
3. Enhance Clinical Documentation
Detailed clinician notes, capturing the procedure approach, body part, device usage, and clinical context, provide the foundation for precise coding, reduce audit risk, and support quality metrics and outcome analysis.
4. Utilize Technology
AI-assisted coding platforms, such as RapidClaims, can suggest accurate codes, identify documentation gaps, and automate validation checks, significantly reducing manual errors and improving coder efficiency.
5. Conduct Proactive Audits
Regular internal audits comparing ICD-10-PCS and CPT selections identify inconsistencies early, ensure compliance with CMS and HIPAA regulations, and prepare organizations for external audits or payer reviews.
Implementing these best practices ensures accurate coding, regulatory compliance, and optimized revenue cycle performance.
Conclusion
Manual coding errors and the complexity of ICD-10-PCS and CPT procedures can slow down revenue cycles, increase claim denials, and create compliance risks. By implementing structured coding practices and utilizing AI-assisted tools, healthcare teams can achieve accurate documentation, faster reimbursement, and audit readiness.
Platforms like RapidClaims, featuring modules such as RapidCode and RapidScrub, automate code suggestions, detect documentation gaps, and maintain compliance, transforming coding workflows across inpatient and outpatient settings.
Take control of your revenue cycle today. Request a Free Demo with RapidClaims to streamline coding, reduce errors, and optimize revenue performance, achieving a potential 70% reduction in claim denials.
Frequently Asked Questions (FAQs)
1. How do I know which procedures require both ICD-10-PCS and CPT codes?
Inpatient procedures are coded using ICD-10-PCS, while related outpatient services or physician-administered procedures may require CPT codes. Reviewing clinical documentation and understanding the service context helps determine when both code sets are needed. AI-assisted coding platforms can flag cases requiring dual coding.
2. Can I rely entirely on AI-assisted coding tools like RapidClaims for all claims?
AI tools provide high accuracy but should complement, not replace, human review. Coders should verify AI-generated suggestions, especially for complex or unusual cases, to maintain compliance and correctness. Combining human expertise with AI support delivers the most reliable results.
3. How can I reduce errors when coding telehealth services?
Ensure correct CPT selections, modifiers, and place-of-service codes are applied. Accurate documentation of the virtual visit, including duration and clinical details, is essential. AI-assisted coding platforms can identify missing or inconsistent information to prevent errors.
4. How do I keep track of frequent changes in CPT and ICD-10-PCS codes?
Subscribe to CMS and AMA updates, attend coding webinars, and maintain a calendar of release dates. Coding software that flags recent updates ensures teams consistently follow the latest guidelines.
5. How can I use coding data to improve operational decisions?
Analyzing ICD-10-PCS and CPT data can identify high-volume procedures, trends in claim denials, and training needs. Insights from coding data support resource allocation, workflow optimization, and strategic planning across inpatient and outpatient services.
%201.png)