.webp)
Difference Between Inpatient and Outpatient Coding


Have you ever found yourself stuck when determining whether a patient’s treatment should be coded as inpatient or outpatient? You’re not alone. The nuances between the two coding systems can impact reimbursement rates, compliance, and overall efficiency in billing processes. However, for many healthcare organizations, differentiating between inpatient and outpatient coding can often be a point of confusion.
In this blog, we’ll dive deep into the difference between inpatient and outpatient coding and explore how mastering these distinctions can help you improve your organization’s financial health.
What is Inpatient Coding?
Inpatient coding is used when a patient is formally admitted to the hospital under a doctor’s order, regardless of the length of stay. The key factor is the formal admission, which indicates that the patient requires comprehensive care over an extended period.
Even if a patient stays in the hospital for more than 24 hours but is not formally admitted (e.g., under observation status), they would still be classified as an outpatient. In inpatient coding, the medical coding assigned must reflect the full range of services provided during the patient’s stay, including treatments, procedures, and monitoring.
Inpatient coding is far more complex than outpatient coding due to the extensive documentation required. Coders must report not only the diagnosis but also the procedures, treatments, and services rendered throughout the patient’s extended stay in the hospital. This requires a detailed understanding of both the patient’s medical condition and the care they received.
The coding process for inpatients uses ICD-10-CM for diagnosis coding and ICD-10-PCS for procedure coding. These codes are specifically designed for inpatient hospital settings. The complexity of inpatient coding stems from the fact that it involves a detailed record of services provided over a long period. These records are often complex, with various treatments, lab tests, and physician notes that need to be interpreted and accurately coded.
Inpatient coding can be particularly challenging because of the variety and volume of services provided, as well as the need to ensure compliance with regulatory guidelines, such as ICD-10-CM for diagnoses, ICD-10-PCS for procedures, and E&M standards.
What is Outpatient Coding?
Outpatient coding, in contrast to inpatient coding, refers to the medical coding used for patients who visit a hospital or clinic for treatment but are not admitted as inpatients. These patients typically receive treatment, undergo procedures or diagnostic tests, and are then discharged within 24 hours. In many cases, outpatient visits are more straightforward and involve less complexity compared to inpatient stays.
In outpatient coding, medical coders focus on a single visit or encounter, which is often brief and involves fewer services than inpatient care. Since these patients aren’t admitted, the treatments and services are generally less extensive, and the documentation is more streamlined.
The coding system used for outpatient services includes ICD-10-CM for diagnosis coding, along with CPT (Current Procedural Terminology) or HCPCS (Healthcare Common Procedure Coding System) Level II codes for procedures, services, and supplies. The use of CPT codes is critical in outpatient settings, as they cover a wide range of services such as office visits, diagnostic tests, and minor surgeries.
Key Differences Between Inpatient and Outpatient Coding
Regarding medical coding, the differences between inpatient and outpatient coding go beyond just the length of stay. Understanding these key distinctions is crucial for healthcare providers to optimize their revenue cycles and reduce the risks associated with coding errors and denials.
1. Coding Systems Used
- Inpatient Coding: Inpatient coding relies on ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) for diagnosis coding and ICD-10-PCS (Procedure Coding System) for procedural coding. The ICD-10-PCS is specifically designed for inpatient settings and covers complex procedures that are performed during extended hospital stays. For instance, when a patient undergoes major surgery or requires extensive inpatient care, the coder uses the ICD-10-PCS codes to document these procedures.
- Outpatient Coding: Outpatient coding, on the other hand, utilizes ICD-10-CM for diagnosis coding but relies on CPT (Current Procedural Terminology) and HCPCS Level II codes for procedures, services, and supplies. CPT codes are used extensively for outpatient visits, including services like consultations, minor surgeries, and diagnostic tests such as X-rays or lab work. HCPCS Level II codes are often used for medical equipment or outpatient medications.
While both use ICD-10-CM, the coding systems diverge significantly regarding procedures. Inpatient coding uses ICD-10-PCS, while outpatient coding uses CPT/HCPCS codes for services provided in a shorter timeframe.
2. Length of Stay and Documentation
- Inpatient Coding: A patient is classified as an inpatient when they are formally admitted to the hospital and stay for more than 24 hours. This extended stay requires a comprehensive and detailed record of all procedures, tests, and treatments performed during the hospitalization. Because of the prolonged period of care, the documentation for inpatient coding is much more complex, requiring coders to track multiple diagnoses, treatments, and any complications that arise.
Moreover, inpatient coders need to assign a Present on Admission (POA) indicator for each diagnosis, which helps distinguish conditions that were present when the patient was admitted from those that developed during their hospital stay.
- Outpatient Coding: Outpatient coding deals with patients who do not stay overnight in the hospital. These patients typically receive treatment in a clinic, emergency room, or outpatient surgical center. The treatment is usually less intensive and requires less detailed documentation. Outpatient coders only need to account for the visit, the diagnosis, and any procedures performed during the visit.
The focus is on providing a snapshot of the patient’s condition and treatment within a brief time frame, typically less than 24 hours. There is no need to track complications or conditions that develop over time.
3. Diagnosis and Treatment Complexity
- Inpatient Coding: In inpatient settings, coders may assign codes for diagnoses that are unconfirmed or suspected. If a diagnosis is not fully established, the coder may still report it based on the clinical documentation, such as terms like "probable" or "suspected." This is particularly important for inpatient settings, where conditions might evolve during the patient's extended stay.
- Outpatient Coding: In outpatient coding, however, coders cannot assign a diagnosis code unless the diagnosis has been confirmed. For example, if a patient presents with symptoms of a disease, outpatient coders can only assign the diagnosis if the physician has confirmed it through tests or a clinical examination.
If the diagnosis remains uncertain, coders are required to report signs and symptoms, rather than a specific condition. In other words, outpatient coding relies on more definitive documentation before a diagnosis can be made.
4. Reimbursement Systems
- Inpatient Coding: Reimbursement for inpatient services follows a system known as Diagnosis-Related Groups (DRGs). DRGs are used under Medicare Part A to classify hospital stays into categories based on the patient’s diagnosis, the procedures performed, and other factors like age, sex, and comorbidities. The DRG system helps determine the amount of reimbursement a hospital will receive for each inpatient stay, making accurate coding essential for ensuring proper payment.
- Outpatient Coding: Outpatient services, covered under Medicare Part B, use a different reimbursement method called the Ambulatory Payment Classification (APC) system. Under APCs, hospitals are paid a set amount for each outpatient procedure or visit, regardless of the complexity or length of the treatment. This system is designed to encourage efficiency in outpatient care and requires precise coding to ensure hospitals are paid accurately for the services provided.
5. Code Assignment and Diagnosis Types
- Inpatient Coding: Inpatient coding often involves multiple diagnoses, including primary, secondary, and any complications or comorbidities. Coders must assess the full range of medical conditions present during the patient’s stay, which may require assigning codes for conditions that weren’t initially apparent at the time of admission but were diagnosed or worsened during the hospital stay. Inpatient coding also involves principal diagnosis assignment, which reflects the main reason for the patient’s admission.
- Outpatient Coding: Outpatient coding is typically simpler, with a focus on the first-listed diagnosis—the reason for the patient’s visit. In many outpatient settings, the treatment involves a focused, single issue that doesn’t require the same level of in-depth coding. Coders assign codes based on the services provided during the encounter, ensuring they match the clinical documentation and patient’s condition.
Challenges in Inpatient and Outpatient Coding

In both inpatient and outpatient coding, healthcare providers face a series of challenges that can affect coding accuracy, compliance, and reimbursement. Below are some of the common pain points encountered in both coding systems:
1. Incomplete or Inaccurate Documentation
- Inpatient Coding: One of the most significant challenges in inpatient coding is incomplete documentation. Given the complexity of inpatient stays, proper documentation is essential to reflect the services provided accurately. Missing or vague documentation can lead to improper coding, affecting reimbursements and compliance. For example, failing to document a patient's comorbid conditions or complications could result in a lower DRG assignment, reducing reimbursement.
- Outpatient Coding: Incomplete documentation also presents a challenge in outpatient settings. For outpatient services to be accurately coded, the diagnosis must be confirmed. However, sometimes, the physician may not provide enough information about the condition, leaving the coder to work with insufficient details. This can lead to coding errors and delayed reimbursements. Coders may need to issue queries to the physician, further delaying the process.
2. Regulatory Compliance and Updates
- Inpatient Coding: Inpatient coding is subject to frequent changes in regulations and coding systems. With updates to ICD-10-PCS codes, as well as changes in the Present on Admission (POA) guidelines, keeping up with these regulations can be overwhelming for coders. The complexity of these guidelines can lead to errors or delays, especially when new policies are not properly communicated to the coding teams.
- Outpatient Coding: Outpatient coding faces similar challenges, particularly with the ever-changing CPT codes and HCPCS level II codes. Healthcare providers need to stay up-to-date with new procedures, services, and guidelines. Without proper systems in place, coders may miss updates or fail to apply the right codes, potentially leading to claim denials or compliance issues.
3. Time-Consuming Manual Processes
- Inpatient Coding: The manual nature of inpatient coding makes it a time-consuming process. Coders are often required to comb through extensive medical records, pulling out relevant details from lengthy patient stays. This can lead to human error and increased operational costs. Additionally, the reliance on human coders can slow down the overall revenue cycle, delaying reimbursements and cash flow for the hospital.
- Outpatient Coding: Though less complex, outpatient coding can still be a slow process, especially when the coding team handles a high volume of visits. The speed of coding affects the timely submission of claims, which in turn impacts the overall revenue cycle. If outpatient coders cannot process claims quickly, it can lead to cash flow issues for clinics or outpatient departments.
4. Claim Denials and Rejections
- Inpatient Coding: Due to the intricacies involved in inpatient coding, claim denials are often tied to coding errors, such as incorrect assignment of diagnosis codes, missing documentation, or inaccurate POA indicators. These denials are costly and time-consuming to resolve, requiring coders and billing departments to revisit patient records and resubmit claims, which further delays payments.
- Outpatient Coding: Outpatient coding errors can also result in claim rejections, especially when a diagnosis is uncertain or incomplete. Coders may also face denials if the proper CPT codes or HCPCS codes are not applied. With outpatient procedures, if the coding does not align with the services documented by the physician, the claim will likely be rejected by payers.
Conclusion:
Inpatient and outpatient coding play vital roles in the healthcare revenue cycle, but they come with distinct requirements and processes. While inpatient coding involves more complex documentation and longer stays, outpatient coding focuses on shorter, more focused visits. Both coding systems require accuracy to avoid claim denials, ensure compliance, and optimize reimbursements.
By understanding the key differences and challenges between these two types of coding, healthcare providers can enhance their coding practices, reduce errors, and improve the efficiency of their revenue cycle management.
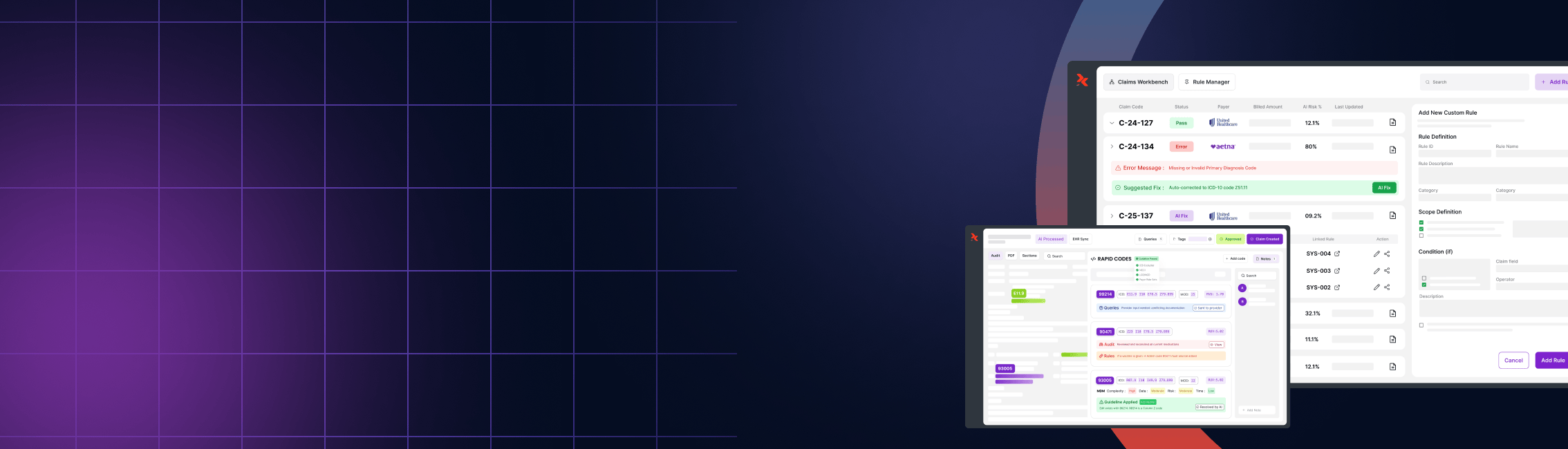
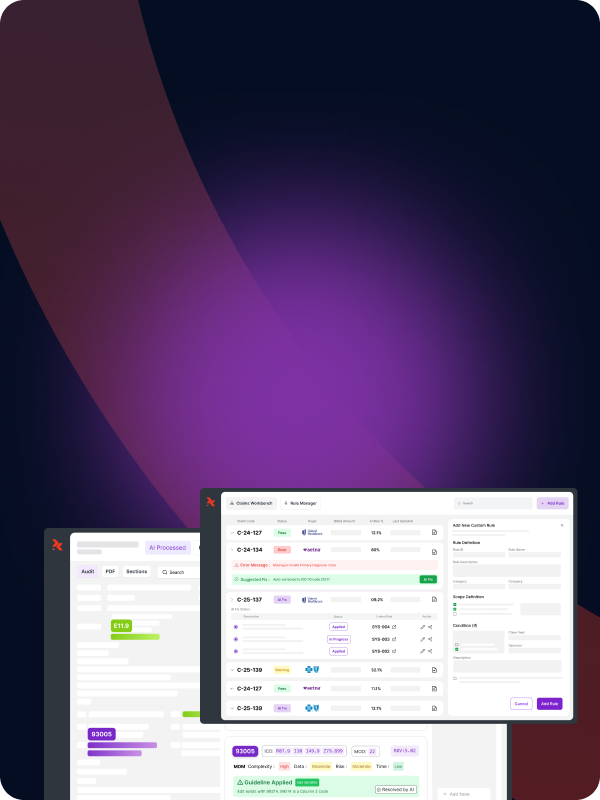
How RapidClaims Can Improve Inpatient and Outpatient Coding
Inpatient and outpatient coding come with distinct challenges that can slow down workflows and lead to errors if not addressed properly. These challenges include the complexity of coding for extended stays, the need for precise documentation, and the continuous updates to regulatory requirements.
To overcome these hurdles, effective solutions are essential for streamlining coding processes, improving accuracy, and reducing delays. RapidClaims leverages AI-powered automation to simplify these tasks, ensuring that both inpatient and outpatient coding are faster, more accurate, and compliant with evolving guidelines.
- AI-Driven Automation for Speed and Accuracy: RapidClaims automates key parts of the inpatient and outpatient coding workflow, assisting coders in reducing errors and accelerating chart processing.
- Real-Time Regulatory Compliance: RapidClaims automatically integrates updates to coding standards, ensuring compliance with the latest guidelines.
- Faster Coding for Improved Cash Flow: By processing charts quickly, RapidClaims helps reduce delays, improving the speed of claim submissions and overall cash flow.
- Proactive Error Detection: AI-driven insights detect coding errors and documentation gaps before claims are submitted, reducing denials.
- Seamless Integration: RapidClaims integrates smoothly with existing EHR and billing systems, optimizing workflows across the healthcare environment.
Ready to streamline your coding process?
Ensure accuracy, reduce claim denials, and speed up reimbursement cycles with RapidClaims’ AI-driven medical coding solutions. Optimize your inpatient and outpatient coding today—get started with a demo and experience the difference!
Frequently Asked Questions
1. What is the main difference between inpatient and outpatient coding?
Inpatient coding involves coding for patients who are formally admitted to the hospital and stay for more than 24 hours, requiring detailed documentation of all treatments and services. Outpatient coding, on the other hand, is for patients who receive treatment or services in a single visit, usually within 24 hours, with less complex documentation.
2. What coding systems are used for inpatient and outpatient settings?
Inpatient coding primarily uses ICD-10-CM for diagnoses and ICD-10-PCS for procedures. Outpatient coding uses ICD-10-CM for diagnoses and CPT or HCPCS Level II codes for procedures, services, and supplies.
3. Why is inpatient coding more complex than outpatient coding?
Inpatient coding is more complex due to the extended length of stay, multiple treatments, and varied services provided over time. It requires more detailed documentation, including the Present on Admission (POA) indicators assignment, which is unnecessary for outpatient coding.
4. How do reimbursement systems differ for inpatient and outpatient services?
Inpatient services are reimbursed through the Medicare Severity-Diagnosis-Related Groups (MS-DRGs) system under Medicare Part A, based on the patient's diagnosis, treatment, and stay duration. Outpatient services are reimbursed under the Ambulatory Payment Classification (APC) system through Medicare Part B, which pays for procedures and services provided during short visits.
5. Can signs and symptoms be coded for inpatient or outpatient services?
In inpatient settings, unconfirmed diagnoses may be coded based on documentation such as "probable" or "suspected" conditions. However, in outpatient settings, coders can only assign a diagnosis code if the diagnosis is confirmed through testing or clinical evaluation.
6. How does the length of stay affect coding?
The length of stay is crucial for determining whether a patient is classified as an inpatient or an outpatient. Inpatients must stay longer than 24 hours, and their coding reflects a broader range of services over time. Outpatients, treated within 24 hours, have simpler coding based on the single visit or treatment.
%201.png)