.webp)
Different Types of Medical Coding and Their Role in Healthcare

According to the World Health Organization, global healthcare spending is expected to rise from $7.8 trillion in 2020 to $10 trillion by 2030. As this growth continues, healthcare systems face the dual challenge of handling complex clinical information alongside massive volumes of financial data with precision and efficiency. Without a standardized approach, the sheer volume of medical records, claims, and reimbursements would quickly become unmanageable.
Medical coding addresses this challenge by converting diagnoses, treatments, and procedures into universal codes. These codes ensure consistent documentation, streamline billing and insurance processing, and maintain reliable health records.
In this blog, you’ll explore the different types of medical coding, their key features, and practical applications that keep modern healthcare systems organized and effective.
TL;DR (Key Takeaways)
- Medical coding standardizes healthcare data for billing, insurance, and record management.
- It utilizes universal classification systems, including ICD, CPT, and HCPCS.
- Coding ensures compliance with legal, clinical, and financial standards.
- Different coding systems serve specific domains: diagnoses, procedures, drugs, or dental care.
- The coding process involves steps ranging from reviewing records to accurately entering codes.
Table of Contents:
- What is a Medical Coding System?
- Importance of Medical Coding in Healthcare
- Top 12 Key Medical Coding Systems You Should Know
- How Medical Coding Works?
- Conclusion
- Frequently Asked Questions (FAQs)
What is a Medical Coding System?
A medical coding system is a standardized framework that assigns alphanumeric codes to medical diagnoses, procedures, services, and equipment. These codes translate clinical information into universally recognized formats, enabling accurate documentation, reporting, and data exchange across healthcare systems. Coding systems such as ICD, CPT, and HCPCS ensure that medical records are consistent, comparable, and usable for clinical, administrative, and financial purposes.
Example:
- A patient diagnosed with Type 2 Diabetes may be assigned the ICD-10-CM code E11.9 (Type 2 Diabetes Mellitus without complications).
- If the patient undergoes a knee replacement, the procedure could be recorded with ICD-10-PCS code 0SRC0J9 (Replacement of Right Knee Joint with Metal, Open Approach).
Now that you know what a classification system is, let’s explore why medical coding is indispensable in healthcare.
Importance of Medical Coding in Healthcare
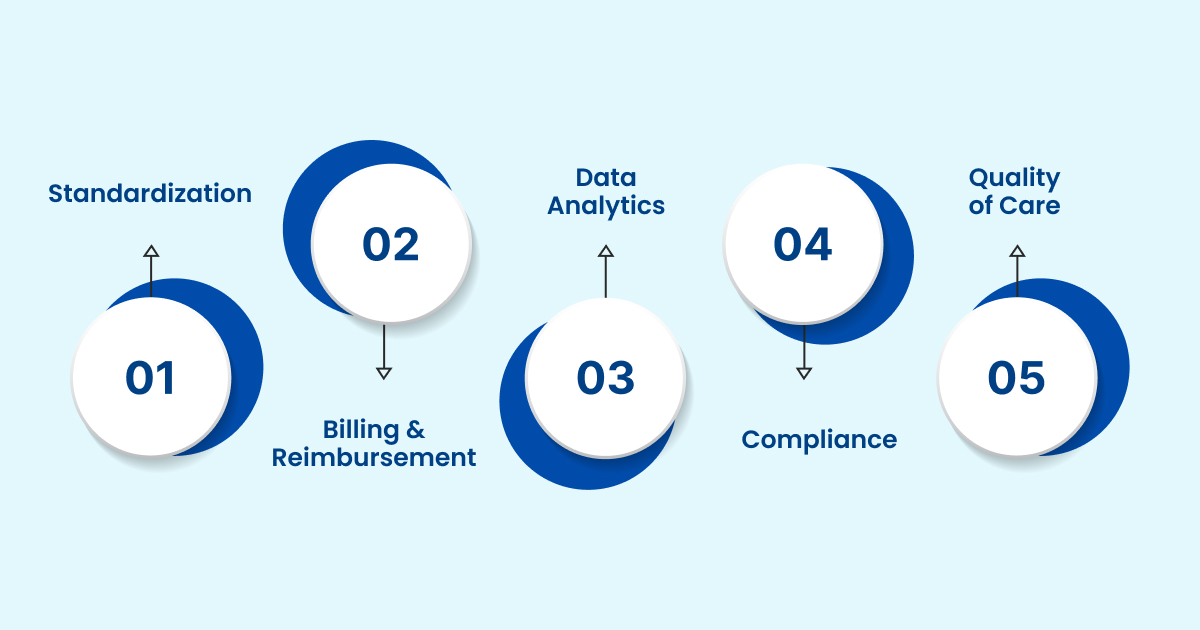
Medical coding is vital for accurate communication, billing, research, compliance, and patient care. It transforms clinical notes into recognized codes, streamlining operations and ensuring accountability across healthcare systems. Below are the key reasons why medical coding is needed:
- Standardizes Communication: Coding creates a common language for medical communication across hospitals, insurers, and regulators. This prevents misinterpretation of patient records and supports consistency across regions and healthcare facilities.
- Enables Accurate Billing and Reimbursement: Each service or procedure is linked to a code that insurers can recognize. This ensures hospitals and doctors receive correct payment while reducing disputes and delays in claim processing.
- Supports Clinical Research and Data Analysis: Coded data allows researchers and policymakers to analyze disease patterns, treatment outcomes, and healthcare utilization. This promotes medical innovation and effective public health planning.
- Ensures Legal and Regulatory Compliance: Coding enables providers to meet the strict documentation standards required by health authorities. It reduces the risks of audits, fraudulent claims, or penalties for incomplete reporting.
- Improves Patient Care: Complete and standardized records allow clinicians to track medical histories more effectively. This helps in accurate diagnosis, treatment planning, and long-term continuity of care.
Let’s now explore the various types of medical coding, which form the foundation for accurate healthcare documentation, billing, and data standardization.
Top 12 Key Medical Coding Systems You Should Know
For healthcare professionals, medical coders, revenue cycle managers, and compliance officers, understanding medical coding systems is essential to ensure accurate documentation, smooth billing, and regulatory compliance. These standardized codes streamline workflows, optimize revenue cycles, and support quality patient care.
Below are the top 10 types of medical coding that every professional should be familiar with:
1. ICD-10-CM (International Classification of Diseases, 10th Edition, Clinical Modification)
ICD-10-CM is the primary U.S. coding system for documenting diagnoses, conditions, and symptoms. It enables clinicians and coders to record patient health data with precision, ensuring accurate billing, effective clinical tracking, and reliable public health reporting. With over 70,000 codes, ICD-10-CM accommodates both common illnesses and rare conditions.
Why It Matters:
- Detailed Diagnosis Coding: Provides a particular classification of patient conditions, enabling precise documentation.
- Billing & Reimbursement: Facilitates accurate processing of insurance claims for healthcare services.
- Public Health Tracking: Supports disease surveillance and epidemiological research at national and local levels.
- Regulatory Compliance: Ensures adherence to federal and payer documentation requirements.
Example: E11.9 represents Type 2 Diabetes Mellitus without complications, and I10 codes essential hypertension.
2. ICD-10-PCS (International Classification of Diseases, 10th Edition, Procedural Coding System)
ICD-10-PCS is the U.S. standard for coding inpatient procedures. Each seven-character code captures precise details about the procedure, including approach, body system, and device used. This granularity supports accurate billing and clinical documentation.
Why It Matters:
- Granular Procedure Documentation: Records inpatient interventions with a high level of detail to reduce errors.
- DRG-Based Reimbursement: Supports accurate payment under Medicare and private insurance programs.
- Clinical Data Analytics: Enables hospitals to track outcomes and assess the effectiveness of treatments.
- Standardization Across Hospitals: Maintains consistency in inpatient medical records across facilities.
Example: 0FB03ZX refers to laparoscopic excision of the liver’s anterior segment.
3. ICD-11: The ICD-10 Update
ICD-11 is WHO’s latest revision, designed for global use with improved digital interoperability. It captures rare conditions, complex disease classifications, and integrates seamlessly with electronic health records.
Why It Matters:
- Global Standardization: Enables consistent disease reporting across various countries and healthcare systems.
- Digital-Ready: Compatible with modern EHRs, facilitating electronic health data exchange.
- Expanded Clinical Detail: Provides granular coding for rare and complex conditions.
- Public Health & Research Utility: Enhances epidemiological studies and international health monitoring.
Example: 1A00 represents cholera, enabling consistent worldwide reporting. ICD-11 also supports public health initiatives, international research, and the sharing of cross-border data.
4. CPT (Current Procedural Terminology)
CPT codes, maintained by the American Medical Association (AMA), provide a standardized system for documenting outpatient procedures and physician services in the United States. They establish a common language that facilitates accurate communication among providers, payers, and regulatory agencies.
Why It Matters:
- Outpatient & Physician Billing: Ensures that procedures and services are billed accurately for reimbursement.
- Clinical Performance Reporting: Supports quality measurement and performance evaluation in medical practice.
- Regulatory Compliance: Aligns documentation with CMS and private payer requirements.
- Standardized Procedure Documentation: Creates uniformity in recording consultations, diagnostics, and surgeries.
Example codes: 99213 for an established patient office visit, 93000 for an electrocardiogram. CPT ensures accurate representation of clinical services across providers and payers.
5. HCPCS Level II (Healthcare Common Procedure Coding System, Level II)
HCPCS Level II codes provide a standardized system for documenting non-physician services, medical supplies, and durable equipment in the U.S. healthcare system. They complement CPT codes by covering items and services not included in physician procedure coding, such as medications, prosthetics, and outpatient supplies.
Why It Matters:
- Standardization of Supplies & Services: Provides consistent coding for durable medical equipment, drugs, and supplies.
- Comprehensive Claims Support: Complements CPT codes for complete and accurate billing.
- Government Payer Compliance: Required for Medicare and Medicaid submissions.
- Cross-Setting Use: Applicable in multiple care settings, including outpatient, home care, and long-term care.
Examples: J1885 for ketorolac injection, L33733 for an orthotic device. HCPCS Level II ensures uniform reporting and proper reimbursement for ancillary healthcare services.
6. CDT (Current Dental Terminology)
CDT codes, developed by the American Dental Association (ADA), provide a standardized system for documenting dental procedures. They ensure consistent communication between dental offices, insurance providers, and regulatory agencies. By using CDT, dental professionals can clearly record preventive, restorative, and surgical procedures, which supports accurate claims, clinical research, and quality reporting.
Why It Matters:
- Dental Billing Accuracy: Ensures that claims are submitted correctly for reimbursement.
- Clinical Consistency: Standardizes documentation of procedures across dental practices to ensure consistency.
- Regulatory Compliance: Meets federal and state reporting requirements.
- Data Analytics: Supports tracking procedure utilization and clinical outcomes.
Examples: D0120 for periodic oral evaluation, D2391 for resin-based composite fillings. CDT improves workflow, claims accuracy, and research in oral healthcare.
7. NDC (National Drug Codes)
NDC codes uniquely identify drugs in the U.S., specifying manufacturer, product, and package size. They provide a standardized framework for pharmacies, hospitals, and insurers to reference medications consistently and accurately. NDC also supports electronic prescribing, drug formularies, and facilitates accurate reporting in healthcare databases, ensuring each drug is tracked reliably across the supply chain.
Why It Matters:
- Medication Standardization: Provides unique identifiers to prevent errors in prescribing or dispensing.
- Billing & Reimbursement: Supports accurate processing of pharmacy claims.
- Supply Chain Management: Enables tracking and inventory control of medications.
- Regulatory Compliance: Meets FDA and payer reporting requirements.
Example: 0002-0800-01 identifies a specific insulin vial. NDC ensures consistency in prescribing, dispensing, and billing medications across pharmacies and healthcare organizations.
8. LOINC (Logical Observation Identifiers Names and Codes)
LOINC standardizes lab and clinical observations, including tests, measurements, and surveys. It enables consistent recording and sharing of results, streamlines lab workflows, reduces errors, and supports research and informed clinical decisions.
Why It Matters:
- Lab Test Standardization: Ensures consistent naming and reporting of laboratory tests to facilitate accurate interpretation.
- EHR Interoperability: Facilitates seamless sharing of clinical data between providers.
- Population Health & Research: Allows aggregation of data for clinical research and outcomes analysis.
- Public Health Reporting: Supports accurate disease surveillance and monitoring.
Example: 2345-7 represents a glucose test. LOINC enhances interoperability, data aggregation, and supports population health initiatives.
9. SNOMED CT (Systematized Nomenclature of Medicine – Clinical Terms)
SNOMED CT is a comprehensive clinical vocabulary covering diseases, procedures, and findings. It allows structured documentation in EHRs, standardizes terminology across organizations, and supports accurate reporting, clinical care, and research.
Why It Matters:
- Detailed Clinical Documentation: Captures precise information for accurate patient records.
- Interoperability: It enables structured data exchange across multiple healthcare systems.
- Clinical Decision Support: Integrates with EHR analytics and alerts for better outcomes.
- Global Adoption: Widely used in international healthcare systems for standardization.
Example: 44054006 represents diabetes mellitus. It enables the detailed recording of patient data in EHRs, supporting informed clinical decision-making and accurate reporting.
10. RxNorm
RxNorm standardizes names and unique identifiers for U.S. medications and clinical drugs. It links drug concepts across systems, enabling consistent communication between prescribers, pharmacies, and EHRs, while supporting e-prescribing, clinical decision support, and safe medication management.
Why It Matters:
- Medication Standardization: Prevents errors in prescribing and dispensing drugs.
- EHR Integration: Supports electronic prescribing and clinical decision-making.
- Billing & Formulary Management: Facilitates insurance claims and formulary tracking.
- Patient Safety: Assists in monitoring drug interactions and allergies.
Example: “Metformin 500 mg oral tablet” is mapped to a unique RxNorm code, ensuring consistent communication across prescribers, pharmacies, and insurers.
11. MS-DRG (Medical Severity Diagnosis-Related Groups)
MS-DRGs classify inpatient stays based on diagnoses, procedures, and patient severity. They standardize reimbursement, reflect clinical complexity, and provide data for outcome analysis, resource allocation, and hospital performance benchmarking.
Why It Matters:
- Inpatient Reimbursement: Guides hospital payments based on patient severity and treatment complexity.
- Severity Adjustment: Accounts for differences in clinical complexity and resource requirements.
- Cost Analysis & Benchmarking: Supports performance evaluation and operational planning.
- Compliance: Ensures adherence to CMS rules and DRG standards.
Example: 291 covers heart failure and shock with major complications. These groups determine Medicare reimbursement and provide insight into resource utilization.
12. APC (Ambulatory Payment Classifications)
APCs group outpatient services by resource use and clinical similarity. They standardize Medicare reimbursement, help hospitals manage costs, streamline billing, and support compliance with federal regulations.
Why It Matters:
- Outpatient Billing Accuracy: Ensures proper payment for outpatient procedures.
- Service Grouping: Bundles procedures by resource use to simplify billing.
- Cost Analysis & Planning: Helps hospitals manage budgets and plan resource allocation.
- Regulatory Compliance: Aligns with CMS outpatient payment standards.
Example: APC 5012 for a Level II emergency department visit. APCs support standardized reimbursement while enabling efficient cost tracking and compliance.
Beyond standard coding frameworks, modern platforms like RapidClaims, powered by RapidCDI, enhance risk adjustment and compliance. It aggregates longitudinal patient data, flags potential HCC conditions, and calculates RAF deltas in real time. Compliance is ensured through AHIMA/CMS-aligned templates and comprehensive audit logs, thereby improving reimbursement accuracy.
Also Read: Differences and Basics of ICD-10 and CPT Codes
How Medical Coding Works?
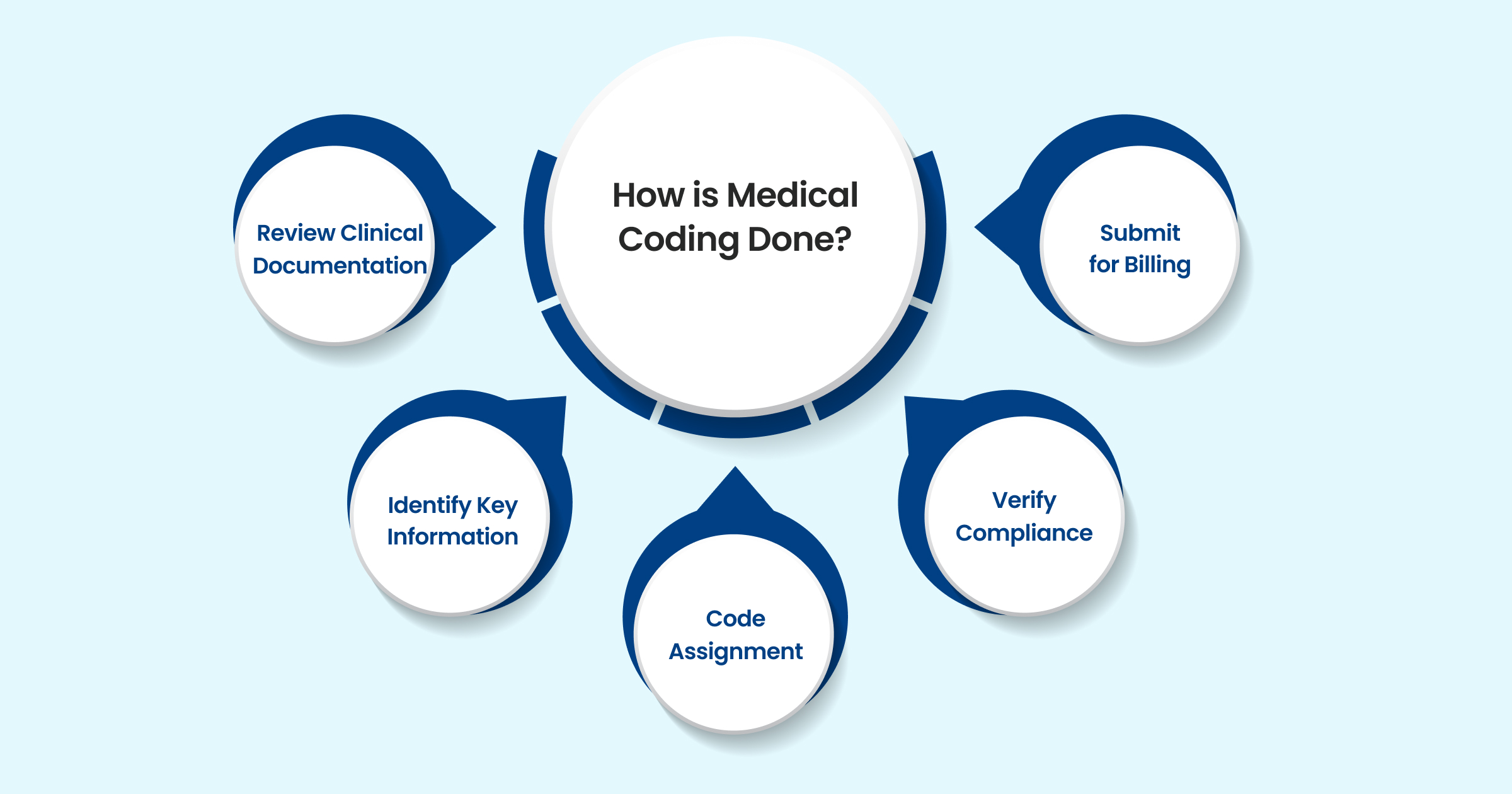
Medical coding follows a systematic workflow to ensure that patient records are accurately converted into standardized codes. Each stage is crucial for error-free documentation, compliance, and smooth reimbursement.
1. Review Medical Records
Before coding begins, coders gather all relevant documents, including physician notes, patient histories, lab results, discharge summaries, and imaging reports. This step ensures no clinical detail is overlooked.
- Provides the foundation for identifying diagnoses and treatments.
- Helps detect inconsistencies or missing documentation.
- Ensures coders have complete patient information before assigning codes.
2. Identify Key Information
Once the records are reviewed, coders highlight essential clinical data, including diagnoses, procedures, medications, and follow-up instructions.
- Focuses on essential clinical facts needed for billing.
- Prevents confusion from redundant or irrelevant notes.
- Aligns information with payer and compliance requirements.
3. Select Appropriate Codes
Using classification systems such as ICD-10-CM, CPT, HCPCS, or NDC, coders map clinical information into standardized codes.
- Ensures universal language across providers and insurers.
- Requires familiarity with coding guidelines and code updates.
- Example: Mapping “Type 2 Diabetes without complications” to E11.9.
4. Ensure Accuracy
Accuracy is crucial in preventing claim denials and compliance penalties. Coders verify that codes match clinical documentation and payer rules.
- Double-checks modifiers, sequencing, and coding rules.
- Reduces risk of billing fraud or underpayment.
- Involves cross-checking with compliance software and coding audits.
5. Enter Codes
The final step is entering validated codes into Electronic Health Records (EHRs) or billing systems to submit claims.
- Automates claim generation for insurers.
- Links codes with provider, patient, and payer details.
- Completes the revenue cycle and ensures reimbursement.
Proper documentation is essential for a smooth reimbursement process. To further streamline coding and ensure compliance, Platforms like RapidClaims integrate with EHRs via SMART on FHIR and HL7. Its RapidCode AI assistant provides line-level rationales and coding suggestions, improving accuracy and reducing denials. Turbo Throughput processes 1,000+ charts per minute at 96 %+ audited accuracy, enabling faster and more reliable claim submission.
Conclusion
Different types of medical coding ensure clear communication, accurate billing, and standardized healthcare documentation. They help physicians, hospitals, insurers, and government agencies maintain consistency across treatments, payments, and research. By mastering these coding systems, healthcare professionals can ensure compliance, improve patient outcomes, and maintain financial transparency.
Integrating AI-driven platforms, such as RapidClaims, into the reimbursement workflow further enhances efficiency and effectiveness. With automated coding processes and seamless EHR integration, RapidClaims reduces errors, streamlines claims handling, and supports timely reimbursement.
Optimize your medical coding workflow with RapidClaims. Request a Free Demo today and see how AI can improve coding accuracy, identify missing details, and streamline documentation.
Frequently Asked Questions (FAQs)
1. What skills are required to become a medical coder?
A. A medical coder needs strong knowledge of anatomy, medical terminology, and coding systems like ICD, CPT, and HCPCS. Attention to detail, analytical skills, and compliance awareness are equally important. Proficiency in Electronic Health Records (EHR) systems also helps coders work efficiently.
2. How do medical coding errors affect healthcare providers?
A. Errors can delay insurance reimbursements, cause claim denials, and lead to compliance penalties. They also impact hospital revenue cycles and patient trust. Regular audits and proper coder training help minimize mistakes.
3. Is medical coding the same worldwide?
A. No, coding systems vary by country. While ICD is globally standardized, systems like CPT and HCPCS are specific to the U.S. Many nations adapt ICD with localized modifications for regulatory needs.
4. What is the difference between medical billing and coding?
A. Medical coding converts clinical information into codes, while billing applies those codes to prepare and submit claims. Coding ensures accuracy, and billing ensures proper financial transactions between providers and payers.
5. How is AI being used in medical coding?
A. AI assists coders by automatically extracting diagnoses and procedures from clinical notes. It improves accuracy, reduces workload, and speeds up claims processing. However, human coders remain essential for ensuring compliance and validating context.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
Related Post
Top Products

%201.png)








