Clinical Documentation Compliance 2026: Requirements and AI Impact
Clinical documentation compliance is a top operational priority. Audits, coding complexity, and payer scrutiny are increasing. Federal oversight, especially for Medicare Advantage and risk-adjusted reimbursement, now focuses on accurate documentation and medical necessity. CMS reports that most improper payments result from poor clinical documentation. Documentation quality directly affects coding accuracy, audit risk, and payment integrity.
For revenue cycle and compliance leaders, documentation gaps are significant risks, not just minor charting issues. Incomplete notes cause denials, inaccurate HCC capture, and costly rework. Health systems need structured, technology-driven documentation strategies to maintain compliance, protect revenue, and be audit-ready.
Key Takeaways
- Denial rates and CMS audits are rising, making documentation compliance a core revenue-protection priority.
- Most issues stem from missing specificity, weak clinical linkage, inconsistent terminology, and unstructured notes.
- Compliance depends on meeting CMS, ICD-10-CM, CPT/HCPCS, NCD/LCD, and HCC v28 documentation requirements.
- Poor documentation drives denials, downcoding, missed HCCs, audit risk, delayed claims, and heavy rework.
- Stronger compliance requires specialty-specific standards, concurrent CDI review, structured templates, and clear coder–clinician communication.
- AI improves compliance by extracting required indicators, identifying gaps, resolving encounter inconsistencies, and validating medical necessity.
- AI delivers highest value in chronic conditions, surgery, behavioral health, HCC workflows, high-volume clinics, and telehealth documentation.
- Tools like RapidClaims strengthens compliance by completing documentation, validating coding, highlighting discrepancies early, and producing audit-ready evidence.
What Is Clinical Documentation Compliance and Why It Matters
Clinical documentation compliance plays a central role in how organizations protect revenue, support accurate coding, and maintain audit readiness. Beyond meeting regulatory expectations, compliant documentation ensures that each encounter contains the clinical detail necessary to justify billed services and represent patient acuity accurately.
Health systems now rely on documentation compliance for several mission-critical functions:
- Supporting accurate clinical coding. Coders require a clear clinical foundation to assign ICD-10-CM, CPT, and HCC codes. When documentation lacks specificity, coding becomes subjective and introduces downstream risk.
- Validating medical necessity. Payers expect documentation to clearly show why a service was ordered, what clinical indicators support it, and how the patient’s condition aligns with coverage rules.
- Capturing true patient complexity. Risk-bearing organizations depend on precise documentation to represent chronic and multifactorial conditions that influence reimbursement and care planning.
- Ensuring record integrity across care settings. Accurate documentation strengthens care transitions, especially for patients moving between inpatient, outpatient, and specialty services.
- Maintaining defensible audit trails. Payer audits often require proof that each coded condition or procedure is supported within the record. Compliance depends on having clear, consistent evidence that stands up to retrospective review.
For operational leaders, these functions demonstrate that documentation compliance is not only a regulatory requirement. It is a core driver of revenue integrity, audit protection, and data accuracy across the clinical and financial ecosystem.
Current Trends: Audits, Denials, and Why Compliance Pressure Is Growing
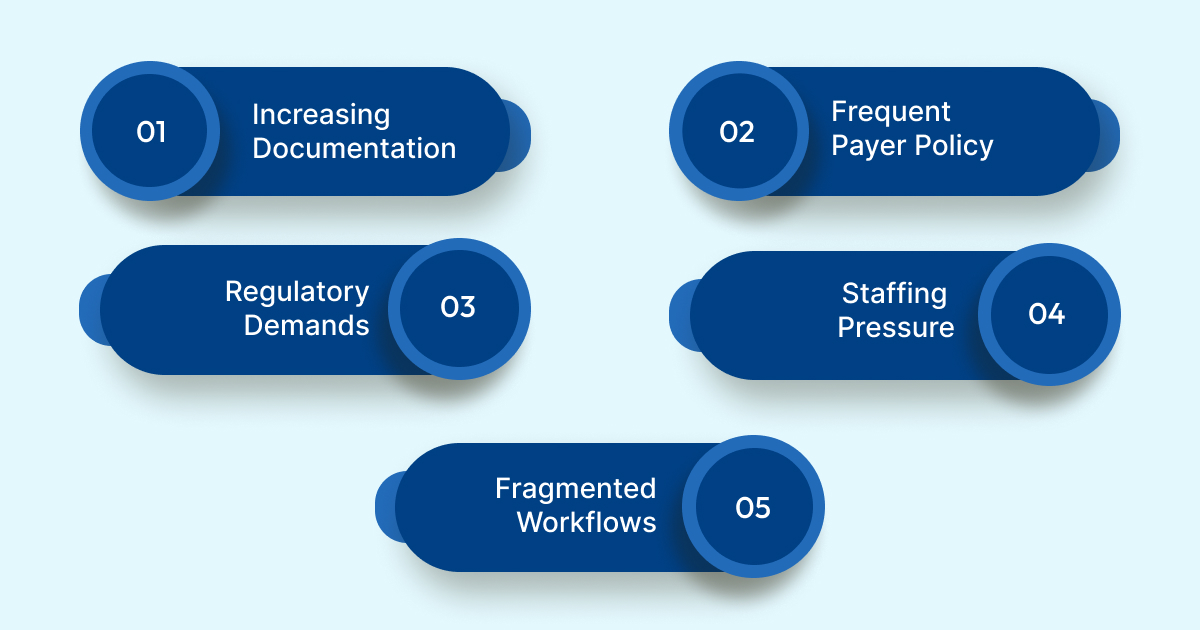
Even with strong compliance expectations, many organizations struggle with documentation consistency and completeness across service lines. These breakdowns typically occur within routine clinical workflows and can be difficult to detect until they create coding or audit issues downstream.
Key challenges include:
- Unstructured narrative documentation: Many encounters rely heavily on free-text notes. Important clinical indicators may be documented informally rather than in structured fields, which makes it harder for coding, CDI, and audit teams to locate required details.
- Insufficient clinical specificity: Providers may document a diagnosis category without capturing stage, acuity, or contributing factors. This limits a coder’s ability to assign the correct ICD-10-CM code and creates exposure during medical necessity reviews.
- Documentation that lacks clear linkage: Encounters often include diagnoses and treatments without explicit connection. Missing linkage between symptoms, findings, and clinical decisions creates gaps that auditors and payers flag as unsupported.
- Variability across providers and specialties: Different clinicians document the same condition using varied terminology or levels of detail, which leads to inconsistent coding outcomes and increased reliance on subjective interpretation.
- Copy-and-paste and templated note risks: Repeated content can mask changes in patient status or introduce contradictions in the record. These inconsistencies become significant liabilities in audits.
- Limited visibility for coding and CDI teams: When documentation is stored across multiple encounter types or modules, reviewers may not have a complete view of the clinical story. This complicates coding and increases the likelihood of overlooked conditions.
These breakdowns demonstrate that documentation compliance challenges arise not from intentional errors but from fragmented workflows, high documentation volume, and inconsistent charting habits. Strengthening compliance begins with understanding these gaps before they affect coding accuracy or payer review.
Core Requirements: Regulatory, Coding & Documentation Standards for Compliance
Clinical documentation compliance is governed by a defined set of regulatory and coding frameworks that determine what must be captured in the record and how that information supports coding and reimbursement. These standards give organizations a practical reference point for evaluating whether documentation is complete and defensible.
Key requirements include:
- CMS documentation guidelines: CMS outlines what constitutes sufficient clinical detail to justify billed services, validate diagnoses, and demonstrate the medical necessity that supports coverage.
- ICD-10-CM specificity expectations: Coding rules require documentation to capture stage, acuity, laterality, severity, and causal relationships. If the record does not include these elements, coders cannot assign the correct code.
- CPT and HCPCS documentation requirements: Procedure coding depends on clear descriptions of what was performed, why it was performed, and how the service aligns with payer coverage rules.
- Medical necessity criteria and NCD/LCD alignment: National and Local Coverage Determinations define the clinical indicators required for coverage. Documentation must show these indicators clearly to avoid payer disputes.
- HCC v28 risk-adjustment documentation rules: Risk-bearing organizations must document chronic conditions with sufficient detail to validate severity and ongoing management. Unsupported conditions increase audit vulnerability.
- HIPAA expectations for documentation integrity: Documentation must be accurate, traceable, and preserved in a way that supports auditability, data integrity, and secure access.
These standards form the backbone of clinical documentation compliance and give CDI, coding, and compliance teams a shared framework for evaluating whether the record can withstand coding validation and payer review.
Operational & Financial Consequences of Poor Documentation
Documentation gaps extend far beyond coding challenges and can create measurable risk across the revenue cycle and compliance environment. When the clinical record does not fully support the care delivered, organizations face several downstream impacts that directly influence financial performance and audit exposure.
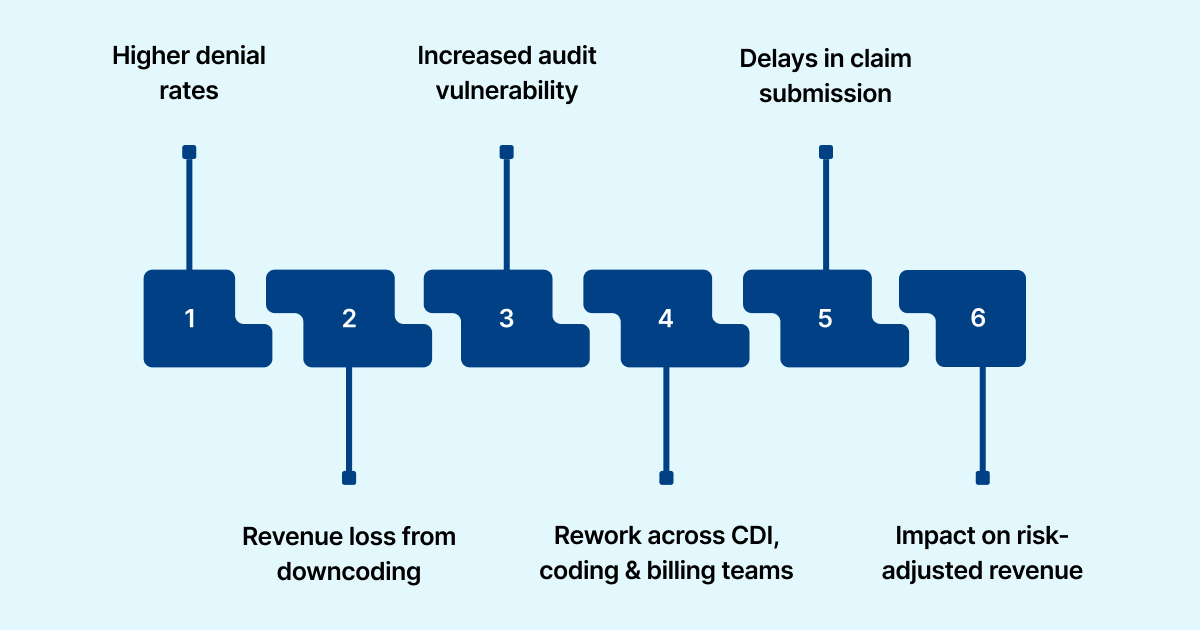
Key risks include:
- Higher denial rates: Many payer denials stem from insufficient clinical detail that fails to justify services or verify diagnosis accuracy. These cases often require additional chart reviews and appeals.
- Revenue loss from downcoding or missing conditions: When documentation lacks the specificity needed to validate diagnoses, coders must assign lower-severity codes or omit conditions entirely. This reduces reimbursement and masks patient complexity.
- Increased audit vulnerability: Incomplete records are more likely to trigger RAC, CERT, and payer-specific audits. Unsupported diagnoses or procedures can result in recoupments and expanded audit review.
- Rework across CDI, coding, and billing teams: Staff must spend additional time correcting documentation gaps, obtaining addenda, and reconciling discrepancies. This slows charge capture and pushes cases into avoidable work queues.
- Delays in claim submission: Encounters often cannot progress to billing until missing or unclear documentation is resolved. These delays extend the revenue cycle and contribute to higher days in accounts receivable.
- Impact on risk-adjusted revenue: Chronic conditions that lack complete documentation cannot be captured for HCC reporting. This affects risk scores, quality measures, and payments for value-based contracts.
For operational decision makers, these risks demonstrate that documentation compliance is not only a clinical expectation. It is a core determinant of financial stability, coding accuracy, and the organization’s ability to withstand payer and regulatory review.
Best Practices to Strengthen Documentation Compliance (Processes & Governance)
Improving documentation compliance requires targeted operational changes that make complete and accurate documentation the default outcome rather than an exception. Organizations can reinforce compliance through structured processes and clearer support for frontline clinicians and coding teams.
Key strategies include:
- Define specialty-specific documentation expectations: Clinical departments benefit from clear guidelines that outline the required elements for common diagnoses and procedures within their specialty.
- Integrate concurrent review into daily workflows: Early review by CDI or coding staff helps catch missing details while the encounter is still fresh and before charges move downstream.
- Establish consistent communication channels between clinicians and coders: Direct clarification pathways reduce delays and ensure that documentation reflects the full clinical picture without multiple back-and-forth requests.
- Use standardized templates that reflect regulatory and coding requirements: Templates and smart phrases can prompt clinicians to capture necessary specificity without disrupting clinical routines.
- Embed medical necessity expectations in ordering workflows: Adding prompts within the EHR order process helps ensure that clinical justification is documented at the moment a service is ordered.
- Create internal governance for documentation quality:Routine audits, documentation scorecards, and feedback loops give departments visibility into performance and areas that require improvement.
These practices create structure around documentation workflows and give clinicians and coding teams the support needed to maintain accuracy, completeness, and compliance at scale.
Want to understand where documentation gaps are creating coding inconsistencies or audit exposure? RapidClaims can review a sample of encounters and generate a documentation integrity assessment that highlights missing clinical indicators, weak linkage, and areas driving denial risk.
Where AI and Automation Fit In – Closing the Compliance Gap
AI improves documentation compliance by addressing points of friction that human reviewers routinely struggle with, especially when working through high-volume, unstructured EHR data. Its value comes from resolving the exact gaps that lead to coding inconsistencies, medical necessity issues, and audit exposure.
Targeted contributions include:
- Locating clinical indicators buried in long encounter notes: AI can identify findings such as eGFR values, exacerbation evidence, imaging impressions, or therapy responses that clinicians often document informally. These details are essential for validating diagnoses like heart failure, COPD, and CKD but are difficult for reviewers to locate manually.
- Detecting missing components required for compliant coding: The system flags absent elements tied to ICD-10-CM logic, such as laterality for orthopedic conditions or stage documentation for pressure injuries. These omissions are common sources of coding variation and audit findings.
- Confirming that documented conditions meet HCC v28 requirements: For risk-bearing organizations, AI checks whether chronic conditions include evidence of evaluation, assessment, or management during the encounter. This prevents unsupported HCC submissions that raise audit risk.
- Reconciling discrepancies across multiple encounters: AI compares documentation across notes, consults, and diagnostic reports to highlight contradictions, outdated problems, or conditions that appear clinically active but are not documented in the current visit.
- Preparing documentation for downstream coding and audit workflows: Instead of producing generic summaries, AI can assemble condition-specific evidence packets that map clinical indicators to diagnoses and procedures. This ensures that coding and compliance teams receive documentation aligned with payer expectations.
- Enhancing medical-necessity documentation at the time of service: When an order is placed for imaging, cardiac testing, or infusion therapy, AI can verify that the encounter record contains the clinical findings required by NCD or LCD policies, reducing the likelihood of payer disputes.
This level of specificity is what makes AI valuable for documentation compliance. It solves the operational problems that cause denials and audit findings, rather than simply reviewing documentation at a surface level.
High-Impact Use Cases for AI-Supported Documentation Compliance
AI delivers the strongest compliance value in clinical areas where documentation requires precise detail or varies widely across providers.
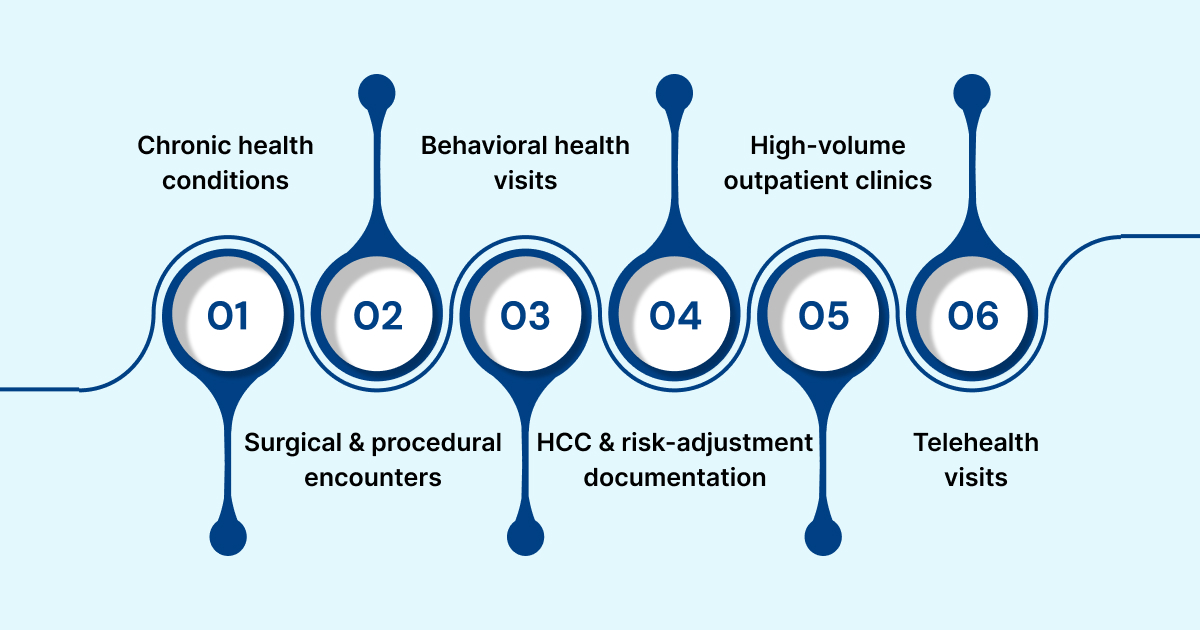
- Chronic conditions such as CHF, COPD, diabetes, and CKD: These conditions depend on specific indicators like severity, staging, and evidence of ongoing management. AI quickly extracts these details from long notes so coders and CDI teams receive complete, compliant clinical information.
- Surgical and procedural encounters: Surgical documentation spans consults, imaging, operative notes, and post-op updates. AI checks that these documents align and include the anatomical and clinical detail needed to support coding accuracy and medical necessity.
- Behavioral health visits: Behavioral health notes are highly narrative and inconsistent. AI structures key elements such as symptom changes, functional assessments, and treatment rationale to ensure documentation supports billed diagnoses and visit types.
- HCC and risk-adjustment documentation: For risk-bearing organizations, AI confirms that chronic conditions include evidence of evaluation or management and flags active conditions missing from the current encounter, protecting risk-adjusted revenue.
- High-volume outpatient clinics: With many providers documenting differently, clinics face wide variability. AI standardizes the capture of clinical indicators across encounters, giving coding and CDI teams consistent and complete data.
- Telehealth visits: Virtual encounters often miss required documentation elements. AI checks for clinical linkage, assessment details, and medication updates to ensure telehealth notes meet payer and compliance standards.
How RapidClaims Supports Documentation Compliance
RapidClaims strengthens documentation compliance by ensuring the clinical record is complete, consistent, and coding-ready before it moves into CDI or billing workflows.
- Improves documentation completeness: AI extracts key clinical indicators from narrative notes and aligns them with diagnoses and procedures, reducing gaps that cause denials or audit issues.
- Validates coding against documented evidence: RapidClaims checks ICD-10-CM, CPT, and HCC codes for alignment with the clinical record, supporting accurate coding and regulatory compliance.
- Flags inconsistencies across encounters: The system highlights conflicting notes, outdated problems, or missing chronic conditions so teams can correct issues early.
- Prepares audit-ready evidence: RapidClaims organizes condition-specific clinical details into clear packets that support payer audits and medical-necessity reviews.
- Reduces rework across CDI, coding, and billing: Standardized documentation inputs decrease clarification requests and help cases move cleanly through the revenue cycle.
Ready to strengthen documentation compliance and reduce preventable denials? RapidClaims applies AI supported documentation analysis, coding validation, and audit ready evidence preparation to improve accuracy before claims move downstream. Request a personalized demo to see how your team can achieve stronger compliance and better revenue protection.
Conclusion
Clinical documentation compliance is now a determining factor in how well organizations protect revenue, avoid audit exposure, and maintain coding accuracy as payer scrutiny intensifies. Gaps in specificity, linkage, and encounter completeness continue to create preventable denials and rework, especially in high-volume and high-complexity service lines. AI offers a practical path forward by identifying missing clinical detail, standardizing documentation inputs, and supporting consistent, audit-ready records across encounters.
As health systems look to strengthen documentation integrity at scale, solutions that improve upstream accuracy have the greatest operational impact. RapidClaims helps organizations achieve this by ensuring documentation is complete, consistent, and aligned with coding and compliance requirements before it reaches the revenue cycle.
If you are evaluating AI-driven approaches to improve documentation quality and reduce compliance risk, request a demo of RapidClaims to see how it supports your organization’s clinical, coding, and revenue integrity goals.
FAQs
Q: What is clinical documentation compliance?
A: Clinical documentation compliance refers to ensuring that provider notes are complete, accurate, specific, and aligned with coding, regulatory, and payer requirements so that billed services are fully supported.
Q: Why is clinical documentation compliance important?
A: Compliance protects organizations from denials, coding errors, and audit findings while ensuring that clinical data reflects true patient acuity.
Q: What are common clinical documentation compliance issues?
A: Frequent gaps include insufficient specificity, missing linkage between diagnoses and treatments, inconsistent terminology, and documentation that does not meet payer medical necessity rules.
Q: How does clinical documentation affect coding accuracy?
A: Coders rely entirely on what is documented. If key clinical details are absent, coding becomes limited, which can result in downcoding or missed HCC conditions.
Q: What regulations influence clinical documentation compliance?
A: Key frameworks include CMS documentation guidelines, ICD-10-CM coding rules, CPT/HCPCS requirements, HIPAA documentation integrity expectations, and NCD/LCD medical necessity criteria.
Q: How can organizations improve clinical documentation compliance?
A: Effective strategies include concurrent CDI review, specialty-specific documentation expectations, structured templates, consistent coder-clinician communication, and internal documentation audits.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








