.webp)
CMS/HCC Medical Coding Explained: Version 28 & Risk Adjustment


As of 2025, Medicare Advantage (MA) plans are transitioning fully to Version 28 of the CMS-HCC risk adjustment model, which reflects the most current methodology for determining beneficiary risk scores. Accurate HCC coding is vital, as it directly affects plan payments and ensures compliance with CMS regulations. Missteps in coding can lead to underpayment, overpayment, or audit risks, making it crucial for medical coders, revenue cycle managers, and compliance officers to understand this model thoroughly.
This blog guides healthcare professionals through CMS/HCC medical coding and the updates introduced in Version 28. It also highlights best practices from the HCC risk-adjusted diagnosis coding guide, helping organizations optimize compliance and reimbursement accuracy.
TL;DR (Key Takeaway)
- Version 28 updates how health conditions affect risk scores and adds new categories for more accurate calculations.
- Correct coding ensures fair Medicare Advantage payments and proper use of resources for high-risk patients.
- Challenges include keeping track of all conditions, frequent updates, audit risk, and integrating with digital systems.
- Following clear steps, such as training, audits, using software, and teamwork between clinicians and coders, improves accuracy.
- AI tools like RapidClaims make coding easier, reduce mistakes, speed up claims, and keep records ready for audits.
Table of Contents:
- Understanding the CMS-HCC Risk Adjustment Model
- Components and Structure of the CMS-HCC Medical Model
- Key Changes in Version 28 of the CMS-HCC Model
- Impact of Version 28 on Medicare Advantage Organizations
- Why Accurate HCC Coding is Essential for Healthcare Success?
- Key Challenges in CMS/HCC Medical Coding
- Implementing CMS-HCC Risk-Adjusted Diagnosis Coding
- Conclusion
- Frequently Asked Questions (FAQs)
Understanding the CMS-HCC Risk Adjustment Model
The CMS-HCC (Hierarchical Condition Category) model is a risk adjustment framework used by the CMS to predict future healthcare costs for Medicare beneficiaries. It assigns risk scores based on demographics and medical conditions, coded using ICD-10-CM diagnoses. These risk scores directly impact MA plan payments, ensuring that reimbursement aligns with the expected cost of care.
Version 28 of the CMS/HCC medical model was introduced for 2024 and implemented in 2025. It incorporates significant updates, including new disease categories, revised coefficients, and frailty factors for Fully Integrated Dual Eligible Special Needs Plans (FIDE SNPs). These changes enhance the accuracy of predicted costs and better reflect patient complexity.
Beneficiary Risk Scores Influenced by Version 28

Under Version 28, the contribution of certain conditions, such as diabetic disorders, to the RAF (Risk Adjustment Factor) score has been standardized. For example, uncomplicated and complicated diabetes are now assigned the same coefficient, so the RAF contribution does not vary based solely on complication status.
Example: Jane, A 66-year-old woman with Type 2 diabetes, peripheral neuropathy, and hypertension.
- Version 24 (V24): Each of Jane’s conditions would have been assigned separate HCC codes, producing a relatively high overall risk score.
- Version 28 (V28): The model emphasizes the overall clinical impact of her diabetes rather than counting each condition individually. While her diagnosis remains significant, the total RAF score may be lower than under V24.
The effect of V28 on RAF scores depends on the combination and severity of conditions, but overall, risk scores are generally expected to decrease under the updated model. Understanding these impacts highlights the importance of examining the CMS/HCC medical model’s core components.
Components and Structure of the CMS-HCC Medical Model
The CMS-HCC model is built on several interrelated components that determine risk-adjusted payments for Medicare Advantage plans:
- Demographic Factors: Age, gender, and Medicaid eligibility of beneficiaries are considered baseline predictors of healthcare costs.
- Hierarchical Condition Categories (HCCs): Medical conditions are grouped into categories that reflect expected healthcare expenditures. Higher-severity conditions are weighted more heavily.
- ICD-10-CM Diagnosis Codes: These codes document patient conditions and map directly to HCCs, forming the basis for calculating risk scores.
- Coefficients: Each HCC has a specific coefficient representing its impact on predicted costs. These coefficients are updated periodically, with Version 28 reflecting recent clinical and cost data.
- Frailty and Interaction Factors: Additional adjustments account for frailty (especially in FIDE SNPs) and interactions between multiple comorbidities, ensuring that complex patients are accurately represented.
- Risk Score Calculation: All components combine mathematically to produce a risk score, which adjusts the payment received by the Medicare Advantage plan.
Accurate documentation and coding across these components directly influence RAF scores, reimbursement, and compliance.
To improve CMS-HCC coding accuracy, organizations can utilize RapidClaims, an AI-powered revenue cycle intelligence platform. It delivers a 98% clean-claim rate, 170% lift in coder productivity, 40% reduction in denials, and 24% HCC capture uplift. The platform automates coding, documentation integrity, and denial recovery, helping providers optimize revenue and compliance.
Key Changes in Version 28 of the CMS-HCC Model

Version 28 updates the CMS/HCC medical model to enhance risk adjustment accuracy and capture patient complexity more effectively. Changes in disease categories, RAF calculations, and frailty factors make precise documentation and coding essential for Medicare Advantage organizations.
Below are the key updates introduced in Version 28:
1. Expanded Disease Categories
Version 28 increases the number of HCCs from 86 to 115, reflecting a broader spectrum of chronic and acute conditions. This expansion allows for more precise risk stratification, ensuring patients with complex or multiple conditions are accurately represented in risk adjustment calculations. Coders must now capture all relevant diagnoses to prevent underestimation of patient risk scores.
2. Revised Coefficients
RAF (Risk Adjustment Factor) coefficients have been recalibrated to better represent the actual expected costs for each condition. This adjustment improves the accuracy of payments and ensures that reimbursement aligns more closely with anticipated healthcare utilization. Coders and compliance teams need to review how these changes affect risk scoring and payment models.
3. Frailty Factors for FIDE SNPs
Frailty factors have been incorporated into Version 28 to account for patient frailty, which significantly influences healthcare resource utilization. These factors adjust RAF scores to better reflect the care needs of frail patients, particularly in Special Needs Plans (SNPs). Documentation of functional limitations and frailty indicators is now critical to ensure accurate risk adjustment.
These changes necessitate rigorous coding practices to avoid under- or over-reporting risk scores. The updates also mean that auditors and compliance teams must revise their review criteria to align with Version 28 standards.
Also Read: AI Medical Coding: The Future of Healthcare Revenue Cycle Management
Impact of Version 28 on Medicare Advantage Organizations
Version 28 of the CMS/HCC medical model has wide-ranging effects on Medicare Advantage (MA) plans, providers, and revenue cycle teams. These updates influence financial performance, compliance, documentation, workflows, and strategic planning.
Below are the key impacts of Version 28 on MA organizations:
1. Financial & Reimbursement Implications
Updated HCC categories and revised coefficients directly affect risk scores, which are used to calculate MA plan payments. Even minor coding inaccuracies can lead to underpayment, reducing available resources for patient care, or overpayment, triggering CMS recoupment audits. Organizations need to monitor historical claims to adjust for retrospective changes in risk scores.
2. Clinical Documentation Accuracy
Clinicians must accurately document all comorbidities and chronic conditions. Version 28 introduces frailty factors and new disease categories, meaning even subtle conditions, such as mild heart failure or early-stage chronic kidney disease, can influence risk adjustment scores. Accurate documentation ensures patients receive appropriate care and plans are fairly compensated.
3. Operational & Workflow Impacts
Revenue cycle managers must revise coding workflows, provide targeted training for coding staff, and update internal audit procedures to align with Version 28. Using technology-enabled coding software can automate the detection of missing or inaccurate codes, streamlining compliance while improving financial outcomes.
4. Strategic Planning
The Version 28 updates may shift overall population risk profiles. Organizations can use this data to identify high-risk patient populations, optimize care management programs, and improve preventive care strategies, aligning financial planning with clinical outcomes.
To enhance CMS-HCC medical coding under Version 28, RapidClaims automates workflows with AI-driven tools. It delivers a 25% RAF accuracy lift, 30 minutes of physician time saved daily, and $2.2M annual revenue gain, while streamlining documentation and reducing administrative burden.
Why Accurate HCC Coding is Essential for Healthcare Success?

Accurate Hierarchical Condition Category (HCC) coding is crucial for ensuring financial stability, regulatory compliance, and effective patient care within the healthcare system. Here’s why it matters:
1. Financial Accuracy
HCC coding has a direct impact on reimbursements under Medicare Advantage (MA) plans. Incorrect codes can result in overpayments or underpayments, which can have a significant impact on a provider's finances. Overpayments must be refunded, potentially leading to penalties, while underpayments can result in inadequate resources to care for high-risk patients, compromising care quality.
2. Regulatory Compliance
CMS requires precise HCC coding to maintain the integrity of Medicare’s risk adjustment model. Coding errors can trigger audits, fines, or exclusion from federal programs, risking a provider's ability to continue participating in Medicare Advantage. Non-compliance can also damage a provider’s reputation, leading to long-term challenges in working with CMS.
3. Optimal Resource Allocation
Accurate coding ensures that Medicare Advantage plans receive the appropriate funding to care for complex patient populations. Without correct HCC coding, plans may lack the necessary financial resources to provide quality care to high-risk patients, leading to poorer health outcomes and inefficient use of resources.
4. Improved Patient Care
Proper coding allows healthcare providers to accurately assess patient conditions, ensuring that care is tailored to their specific needs. Inaccurate coding can result in missed diagnoses, delayed treatments, and gaps in care, ultimately reducing the effectiveness of interventions and harming patient outcomes.
5. Data Integrity and Healthcare Insights
Correct HCC coding enhances the accuracy of healthcare data, which is crucial for clinical research, public health initiatives, and policymaking. Reliable data ensures that healthcare strategies are based on accurate population health information, ultimately leading to better-informed decisions and improved care delivery.
While accurate HCC coding is essential for financial, regulatory, and clinical success, implementing it under Version 28 introduces several practical challenges for healthcare organizations.
Key Challenges in CMS/HCC Medical Coding
Accurately implementing Version 28 of the CMS/HCC medical model presents multiple challenges for healthcare organizations. Coders and clinicians must manage complex documentation requirements, frequent updates, audit risks, and workflow integration to ensure precise risk adjustment and compliant reimbursement.
- Complex Documentation: Clinicians must capture all comorbidities, chronic conditions, and frailty indicators. Omissions can lower risk scores and reduce reimbursement.
- Frequent Updates: CMS regularly revises HCC categories, coefficients, and coding guidelines, necessitating ongoing staff training and monitoring.
- Audit Exposure: Inconsistent or inaccurate coding increases the risk of CMS audits, recoupments, and compliance penalties.
- Workflow Integration: Updating coding practices within existing EHR and revenue cycle systems can be technically challenging and resource-intensive.
To tackle these challenges, organizations should adopt a structured approach that enhances coding accuracy, ensures compliance, and optimizes finances. Next, we’ll explore how to implement CMS-HCC risk-adjusted diagnosis coding to achieve these results effectively.
Implementing CMS-HCC Risk-Adjusted Diagnosis Coding
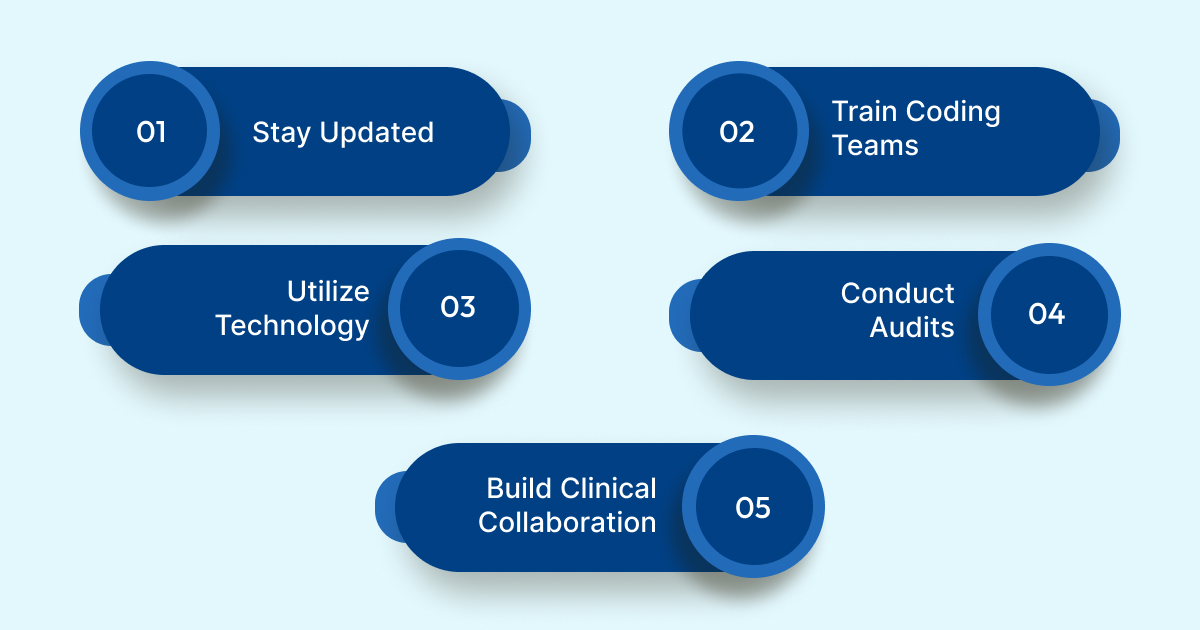
Effective implementation of HCC risk-adjusted coding requires a structured approach. Organizations should focus on staying current with CMS Version 28 updates, training coding teams, utilizing technology, conducting regular audits, and building collaboration between clinicians and coders to ensure accurate and compliant documentation.
Below are the key steps to follow:
1. Stay Updated: Regularly review CMS publications and Version 28 updates. Staying informed about new guidelines and coding clarifications ensures that your organization remains compliant with evolving standards.
2. Train Coding Teams: Ensure coding staff are trained on the latest HCC mapping changes, frailty factors, and updated coefficients. Ongoing training keeps teams accurate and minimizes coding errors.
3. Utilize Technology: Use risk-adjustment software integrated with Version 28 updates to automate coding processes and verify accuracy. Technology streamlines workflow, reduces manual errors, and enhances coding precision.
4. Conduct Audits: Perform regular audits to detect coding discrepancies before they become compliance issues. Audits help identify areas for improvement and ensure adherence to CMS standards.
5. Build Clinical Collaboration: Encourage collaboration between clinicians and coders to ensure that all relevant conditions are accurately documented. Proper communication helps capture a comprehensive picture of patient health and ensures correct coding.
By implementing these steps, healthcare organizations can strengthen coding accuracy, mitigate compliance risks, and safeguard financial integrity for Medicare Advantage programs.
Conclusion
Manual and inconsistent CMS/HCC medical coding under Version 28 can lead to underpayments, audit exposure, and compliance risks. Accurate documentation, staying updated on CMS guidelines, and implementing structured coding practices are essential to ensure precise risk adjustment and fair reimbursement.
Healthcare organizations can benefit from AI-powered solutions like RapidClaims, which streamline risk-adjusted coding, automate claims processing, and provide audit-ready documentation. Using such technology reduces manual errors, enhances efficiency, and ensures compliance with CMS standards.
Ready to reduce coding errors and streamline your revenue cycle, recover hidden revenue, and cut denials by 70%? Request a Free Demo with RapidClaims and experience AI-powered, compliant claims management.
Frequently Asked Questions (FAQs)
1. How do I ensure my coding reflects the expanded HCC categories in Version 28?
To align with the expanded 115 HCCs in Version 28, it's crucial to review patient records and identify all applicable diagnoses thoroughly. Utilize updated ICD-10-CM mappings and ensure that each condition is accurately documented and coded to capture the full spectrum of patient health status. Regular training and utilization of advanced coding software can aid in this process.
2. I noticed a decrease in my patient's RAF score under Version 28; what could be the reason?
A decrease in RAF scores may result from several factors, including the reclassification of certain conditions, changes in coefficient values, or the removal of previously used diagnosis codes. It's essential to review the updated HCC mappings and ensure that all relevant conditions are accurately captured to reflect the patient's true health status.
3. How can I stay updated with the ongoing changes in the CMS/HCC medical model?
Staying informed requires regularly reviewing CMS publications, attending relevant webinars, and participating in training sessions offered by professional organizations. Additionally, subscribing to updates from reputable healthcare information providers can help keep you abreast of the latest changes and best practices.
4. I work with a diverse patient population; how does Version 28 address this?
Version 28 aims to more accurately reflect the complexity of diverse patient populations by incorporating a broader range of conditions and updating coefficient values. This approach ensures that Medicare Advantage plans receive appropriate reimbursement for the care of patients with varied health profiles.
5. How do I handle conditions that no longer map to a payment HCC in Version 28?
For conditions that have been removed from the payment HCC list, it's important to document them accurately in the patient's medical record for clinical care purposes. However, since they no longer impact risk adjustment payments, ensure that coding practices are updated to reflect the current model and focus on conditions that are reimbursable under Version 28.
%201.png)