AI Medical Coding: The Future of Healthcare Revenue Cycle Management

Medical coding is at the core of the healthcare revenue cycle, but traditional methods are slow, error-prone, and overloaded with complex claims and payer rules. Mistakes or delays can cost providers thousands in denied or delayed reimbursements.
AI medical coding is changing this by automating repetitive tasks, detecting errors before claims are submitted, and letting revenue cycle teams focus on higher-value work. From reducing denials to speeding up accounts receivable, AI makes coding faster, more accurate, and more efficient.
In this blog, we explore how AI is transforming medical coding workflows and improving revenue cycle outcomes.
Key Takeaways:
- Core Function of Medical Coding: Medical coding connects clinical documentation to billing, compliance, and reporting, ensuring accurate reimbursement and audit readiness.
- AI-Driven Accuracy: AI automates code assignment and error detection, reducing manual mistakes, claim denials, and compliance risks.
- Operational Efficiency: Automation eliminates repetitive work, enabling coders to focus on complex cases and strategic RCM initiatives.
- Proactive Denial Prevention: Predictive analytics identify high-risk claims early, preventing costly denials and improving cash flow stability.
- Data-Backed Insights: AI-generated analytics reveal trends in denials, coding accuracy, and performance, supporting smarter RCM decisions.
- Seamless Implementation: Success depends on clean data, system integration, staff training, and ongoing model updates to sustain accuracy.
- RapidClaims Advantage: RapidCode delivers fast, compliant, and adaptable AI coding, covering ICD, CPT, and E&M codes with transparent audit trails and few-shot learning for quick deployment.
Table of Contents:
- What is Medical Coding?
- How AI is Transforming Medical Coding?
- Benefits of AI Medical Coding in Revenue Cycle Management
- Applications of AI Medical Coding in Revenue Cycle Management
- How to Implement AI Medical Coding in Your Organization
- RapidClaims: Transforming Medical Coding with AI Precision
- Conclusion
- FAQs
What is Medical Coding?
Medical coding is the process of translating clinical documentation from patient encounters into standardized alphanumeric codes, such as ICD-10, CPT, and HCPCS. These codes are used for billing, insurance claims, reporting, and compliance purposes. Accurate coding ensures timely reimbursement from payers, minimizes claim denials, and maintains adherence to regulatory standards such as HIPAA and CMS guidelines.
Beyond financial purposes, medical coding also plays a critical role in quality reporting, clinical research, and operational decision-making. Precise coding provides insight into patient outcomes, service utilization, and healthcare trends, helping organizations track performance, identify gaps in care, and support audit readiness.
In short, medical coding is the backbone of revenue cycle management, linking clinical care to financial and compliance operations while supporting organizational efficiency and patient care quality.
How AI is Transforming Medical Coding?
AI medical coding RCM automates the coding process, checks documentation for accuracy, and flags missing or inconsistent information before claims are submitted. Key components include:
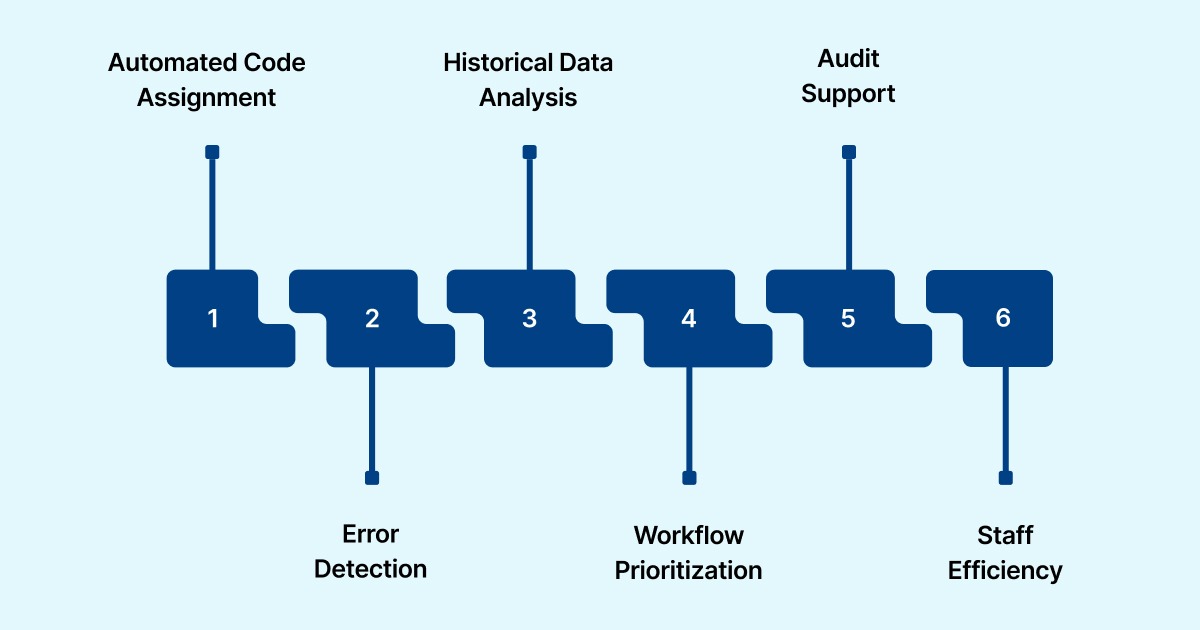
Alt text:How AI is Transforming Medical Coding?
- Automated Code Assignment: AI assigns ICD-10, CPT, and HCPCS codes accurately based on clinical documentation.
- Error Detection: Identifies inconsistencies, omissions, or inaccuracies in documentation before claims submission.
- Historical Data Analysis: Leverages past claim data and payer rules to predict potential denials and reduce errors.
- Workflow Prioritization: Flags high-value or high-risk claims for faster processing.
- Audit Support: Provides detailed insights and documentation checks to ensure compliance.
- Staff Efficiency: Frees coders to focus on complex cases, audits, and strategic initiatives.
Healthcare organizations using AI report faster accounts receivable, fewer denials, and higher coding accuracy, making revenue cycle management more efficient and reliable.
Also read: AI-Powered Automation in Medical Coding
Benefits of AI Medical Coding in Revenue Cycle Management
Implementing AI in medical coding delivers measurable improvements across the revenue cycle, helping healthcare organizations optimize operations, reduce errors, and improve financial outcomes.
Key benefits include:
- Faster Claims Processing: AI automates code assignment, flags missing or inconsistent documentation, and accelerates claim submission, reducing accounts receivable (A/R) days and improving cash flow.
- Higher Coding Accuracy: AI minimizes human error by cross-checking documentation against payer rules and historical data, reducing claim denials and audit risks.
- Proactive Denial Prevention: Predictive algorithms identify high-risk claims before submission, enabling teams to address potential issues and prevent costly denials.
- Operational Efficiency: By handling repetitive coding tasks, AI frees coders and revenue cycle staff to focus on complex cases, audits, and strategic initiatives. Platforms like RapidClaims’ RapidCode deliver measurable time savings, achieving a 1.7x productivity boost. This is equivalent to 2 hours saved per coder per day.
- Regulatory Compliance: AI ensures coding adheres to ICD-10, CPT, and payer-specific guidelines, supporting audit readiness and reducing regulatory exposure.
- Actionable Insights: Analytics from AI systems provide trends, error patterns, and performance metrics, empowering management to make data-driven decisions and improve workflows.
These benefits not only protect revenue but also enhance staff productivity, patient satisfaction, and overall reliability of the revenue cycle process.
Applications of AI Medical Coding in Revenue Cycle Management
AI medical coding is revolutionizing healthcare revenue cycle management by automating and enhancing various processes. Its applications lead to significant improvements in efficiency, accuracy, and financial outcomes:
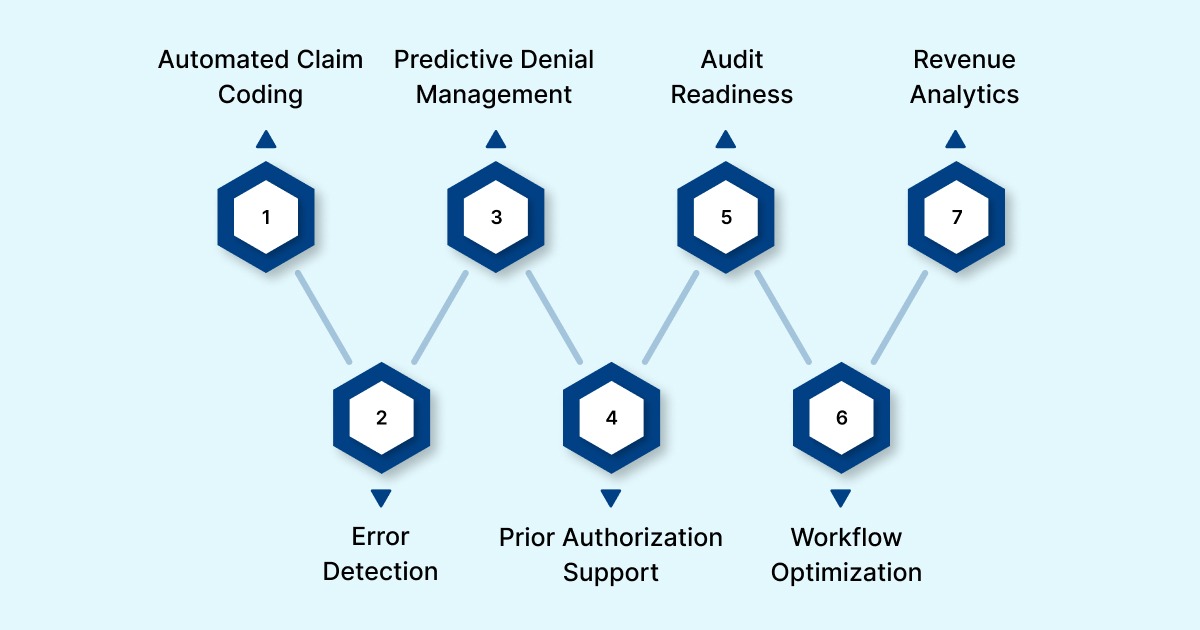
Alt text:Applications of AI Medical Coding in Revenue Cycle Management
1. Automated Claim Coding
AI systems can automatically assign ICD-10, CPT, and HCPCS codes based on clinical documentation. This automation reduces manual errors and accelerates claim submissions, improving cash flow. For instance, Auburn Community Hospital reported a 50% decrease in discharged-not-final-billed cases, a 40% improvement in coder productivity, and a $1 million positive impact on revenue, over ten times its investment
2. Error Detection and Correction
AI analyzes clinical notes to identify missing or inconsistent information before claims are submitted. This proactive approach minimizes denials and reduces the need for manual rework. A Scandinavian study found that AI tools reduced coding time by 46% for complex clinical texts, enhancing efficiency without compromising accuracy.
3. Predictive Denial Management
By analyzing historical claim data and payer patterns, AI can predict which claims are likely to be denied. This allows healthcare organizations to address potential issues proactively, reducing denial rates and improving reimbursement cycles.
For example, a California healthcare network reported a 22% decrease in prior authorization denials and an 18% reduction in denials for non-covered services after implementing AI-powered claims review.
4. Prior Authorization Support
AI streamlines the prior authorization process by verifying requirements, submitting requests, and tracking approvals in real time. This reduces delays and prevents denials due to missing authorizations, enhancing operational efficiency.
5. Audit Readiness and Compliance
AI continuously monitors coding accuracy and compliance with payer-specific rules and regulatory standards. This ensures that claims adhere to current guidelines, supporting audit readiness and reducing regulatory risk.
6. Workflow Optimization and Resource Allocation
AI prioritizes claims based on factors like revenue impact and likelihood of denial, enabling staff to focus on high-value tasks. This optimization leads to better resource allocation and improved overall efficiency.
7. Revenue Analytics and Reporting
AI provides actionable insights through dashboards and analytics, highlighting trends in claim denials, coding accuracy, and financial performance. This data-driven approach empowers healthcare organizations to make informed decisions and optimize revenue cycle processes.
These applications demonstrate how AI medical coding not only enhances operational efficiency but also contributes to improved financial outcomes and compliance in healthcare revenue cycle management.
RapidCode extends these capabilities with an advanced AI coding engine designed for speed, precision, and adaptability. It deploys quickly, adapts to each organization’s workflows through few-shot learning, and ensures complete guideline coverage across ICD, CPT, and E&M codes. With transparent audit trails, intelligent E&M analysis, and customizable rule sets, RapidCode enables confident, compliant coding.
Also read: What are the Benefits and Types of Medical Coding Audits?
How to Implement AI Medical Coding in Your Organization
Successfully integrating AI into medical coding requires planning, strategy, and continuous monitoring. Here’s how you can maximize results:
- Start with Clean, Structured Data: AI relies on accurate clinical documentation and historical claims data. Ensure records are complete, standardized, and free from errors to allow AI algorithms to correctly assign codes and detect inconsistencies.
- Integrate with Existing RCM Systems: Seamless integration with EHRs, practice management systems, and billing platforms prevents workflow disruption. AI should complement, not replace, existing processes, allowing coders to access insights within familiar tools.
- Pilot Before Full Deployment: Test AI solutions on a subset of claims to measure accuracy, identify gaps, and refine algorithms. Pilot programs reduce risk and provide measurable outcomes before scaling organization-wide.
- Provide Staff Training and Change Management: Coders, auditors, and RCM staff must understand how AI works and how to use its recommendations. Proper training fosters trust, encourages adoption, and ensures AI is used effectively rather than ignored.
- Monitor Performance and Update Models Regularly: AI models must evolve with payer rules, regulatory updates, and coding standards. Regular monitoring and algorithm updates ensure accuracy, prevent denials, and maintain ROI over time.
- Focus on High-Impact Use Cases First: Prioritize areas where AI can deliver immediate benefits, such as high-volume coding, claims with historically high denial rates, or complex coding scenarios. Early wins build confidence and justify further investment.
- Combine AI with Human Oversight: AI enhances efficiency, but human review is essential for complex or ambiguous cases. Coders remain critical for quality assurance, audit readiness, and handling edge cases.
Putting best practices into action requires the right tools—RapidClaims demonstrates how AI medical coding helps providers streamline workflows, increase coding accuracy, and recover revenue faster.
RapidClaims: Transforming Medical Coding with AI Precision
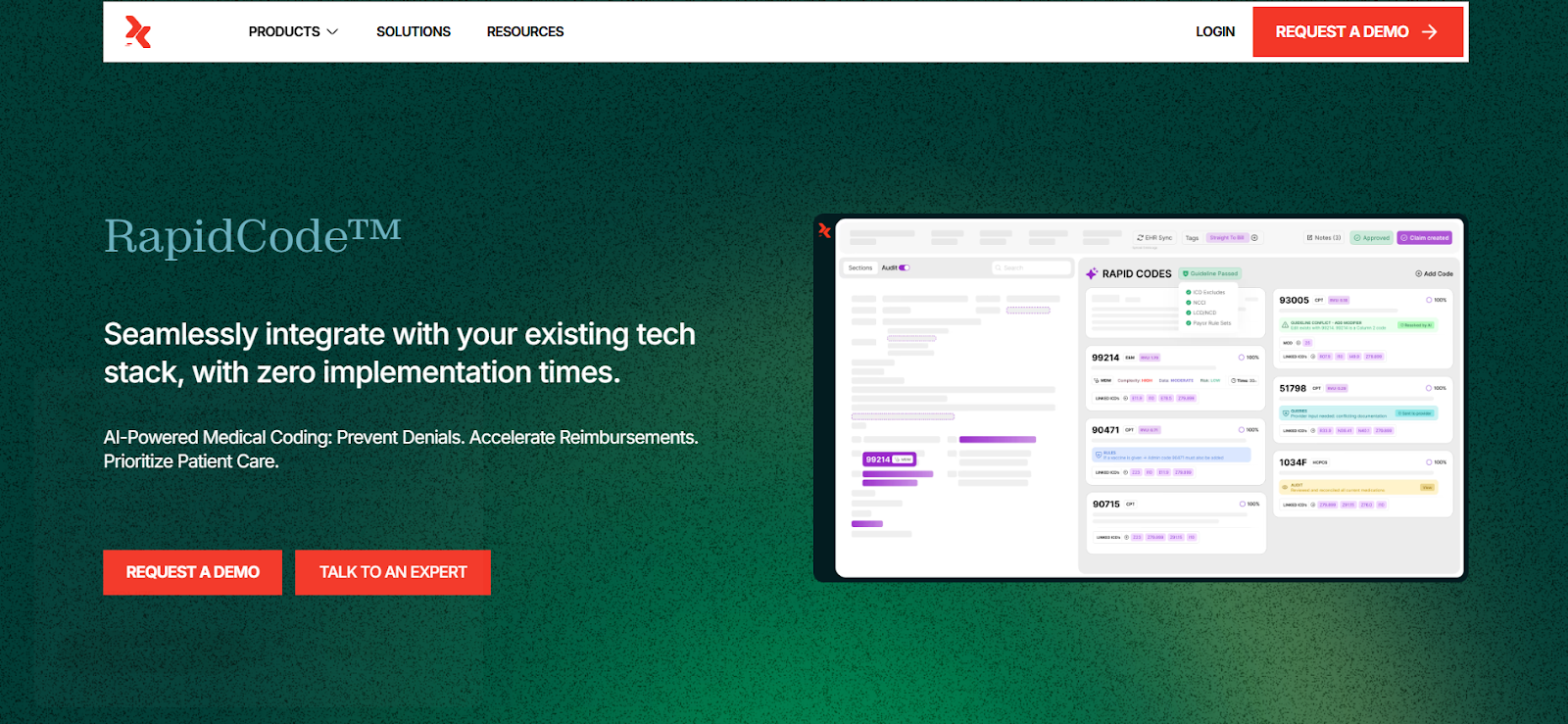
RapidClaims’s RapidCode is designed to streamline revenue cycle management by automating coding processes with exceptional accuracy and efficiency.
Key Features of RapidCode:
- Autonomous Coding with Few-Shot Learning: RapidCode utilizes a few-shot learning approach, enabling it to adapt swiftly to specific workflows with just 500 charts, unlike traditional systems that require thousands. This ensures high accuracy from day one.
- Comprehensive Coding Coverage: The platform supports a wide range of coding systems, including ICD-10, CPT, E&M, HCPCS, and HCC, across over 36 specialties. It ensures 100% adherence to official guidelines and payer requirements.
- Transparent Audit Trails: Every code generated is accompanied by clear explanations, providing a complete audit trail that ensures compliance and instills confidence in the coding process.
- Intelligent Medical Decision Making: RapidCode's AI continuously learns and evolves, staying current with regulations and enhancing coding accuracy. It also features an E&M MDM solver for precise service level determination.
- Automated Claims Generation: The platform generates submission-ready claims, reducing the risk of denials by leveraging historical denials data and ensuring compliance with NCCI edits and payer requirements.
By integrating RapidClaims into your revenue cycle management, you can enhance coding accuracy, reduce denials, and accelerate reimbursements, all while maintaining compliance and improving operational efficiency.
Conclusion
AI medical coding is transforming revenue cycle management by improving accuracy, reducing denials, and accelerating claim processing. Traditional manual coding can be slow, error-prone, and resource-intensive, leaving staff overwhelmed and reimbursements delayed.
AI-powered solutions like RapidClaims automate code assignment, validate documentation, and flag inconsistencies before claims are submitted. This allows coders and revenue cycle teams to focus on complex cases, audits, and strategic tasks rather than repetitive manual work.
Schedule your demo of RapidClaims today to see how AI can streamline your coding processes, protect revenue, and optimize your RCM performance.
FAQs
Q1. What is AI medical coding RCM?
AI medical coding RCM uses artificial intelligence to automate code assignment, validate documentation, and reduce errors, improving accuracy, efficiency, and revenue cycle management in healthcare organizations.
Q2. How does AI improve coding accuracy?
AI analyzes historical claims, documentation, and payer rules to identify inconsistencies or missing information, reducing coding errors and preventing denials before claims are submitted.
Q3. Can AI reduce denials in RCM?
Yes, AI medical coding RCM predicts high-risk claims, flags documentation gaps, and ensures compliance, significantly reducing claim denials and improving reimbursement rates.
Q4. Does AI replace human coders?
No, AI supports coders by handling repetitive tasks, allowing them to focus on complex cases, audits, and strategic initiatives while boosting productivity.
Q5. What are the benefits of AI in revenue cycle management?
AI medical coding RCM accelerates claim processing, reduces errors, improves compliance, increases coding accuracy, and enhances overall operational efficiency and cash flow.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
Top Products

%201.png)








