Average Claim Denial Rate in 2025: Benchmarks and Key Drivers

Claim denials continue to rise as payer policies evolve and clinical documentation requirements become more detailed and tightly enforced. Revenue cycle teams are facing growing pressure to submit claims that are not only accurate but fully supported by clear, compliant documentation and precise coding. As review criteria expand across commercial, Medicare Advantage, and value-based programs, even minor gaps in documentation or code selection can result in denials, delays, and added rework.
Understanding the average claim denial rate and the operational factors that drive it is critical for coding, CDI, compliance, and revenue integrity leaders. Many denials originate upstream from preventable issues such as missing clinical specificity, inconsistent terminology, outdated coding logic, or incomplete authorization workflows. Manual processes struggle to keep pace with frequent guideline updates, including ICD-10-CM changes and HCC v28 requirements, which increases exposure to avoidable denials.
As a result, healthcare organizations are increasingly turning to AI-enabled medical coding and documentation intelligence to strengthen first-pass claim quality. Platforms like RapidClaims help teams identify documentation gaps early, apply coding rules consistently, and align claims with payer expectations before submission. This article explores current denial benchmarks, the most common drivers behind preventable denials, and how AI-driven coding workflows support more reliable reimbursement in 2025.
Key Takeaways
- The average claim denial rate continues to climb above 10 percent in 2025 as payer scrutiny intensifies.
- Denial trends differ by care setting and payer type, making segmented benchmarks more actionable than national averages.
- Most preventable denials originate from documentation gaps, coding inaccuracies, eligibility issues and authorization errors.
- AI-enabled platforms like RapidClaims reduce denials by improving documentation completeness, code specificity and payer alignment before submission.
- Stronger integration, clear QA workflows and updated compliance rules (ICD-10-CM, CPT, HCC v28) are essential for reducing financial exposure.
What Is the Average Claim Denial Rate?
The average claim denial rate varies significantly in 2025, influenced by care setting, payer mix, and encounter complexity. Because these variables differ widely across organizations, reviewing detailed denial patterns provides more meaningful insight than relying on a single national average.
Denial Benchmarks by Care Setting
Surveyed organizations report distinct patterns connected to clinical environment and documentation structure:
- Hospitals and health systems: Higher denial activity for encounters requiring more detailed clinical justification
- Large medical groups: Elevated denial clusters in cardiology, orthopedics, and behavioral health
- Outpatient surgery centers: Denials linked to authorization or procedural documentation
- Emergency departments: Variation tied to rapid documentation and diverse encounter types
These differences highlight why service line–level benchmarks offer more accurate performance indicators.
Variation Across Payers
Payers apply different criteria that influence denial outcomes:
- Commercial payers: Higher initial denials for eligibility, authorization, and coding checks
- Medicare Advantage: Focus on documentation sufficiency and HCC validation
- Traditional Medicare: Lower initial denials but more emphasis on post-payment review
This variation helps organizations understand which parts of the claim process require the most attention.
Why Segmented Benchmarks Matter
Segmented benchmarks help identify:
- Frequent documentation gaps
- Specialties with recurrent inconsistencies
- Payer rules influencing denial patterns
- Areas where AI platforms like RapidClaims can support accuracy and reduce rework
This approach gives leaders a clearer view of preventable denial sources.
Why Claim Denials Continue to Increase
Denials continue to rise in 2025 as healthcare organizations handle larger chart volumes and more detailed payer scrutiny. Several environmental forces contribute to this trend.
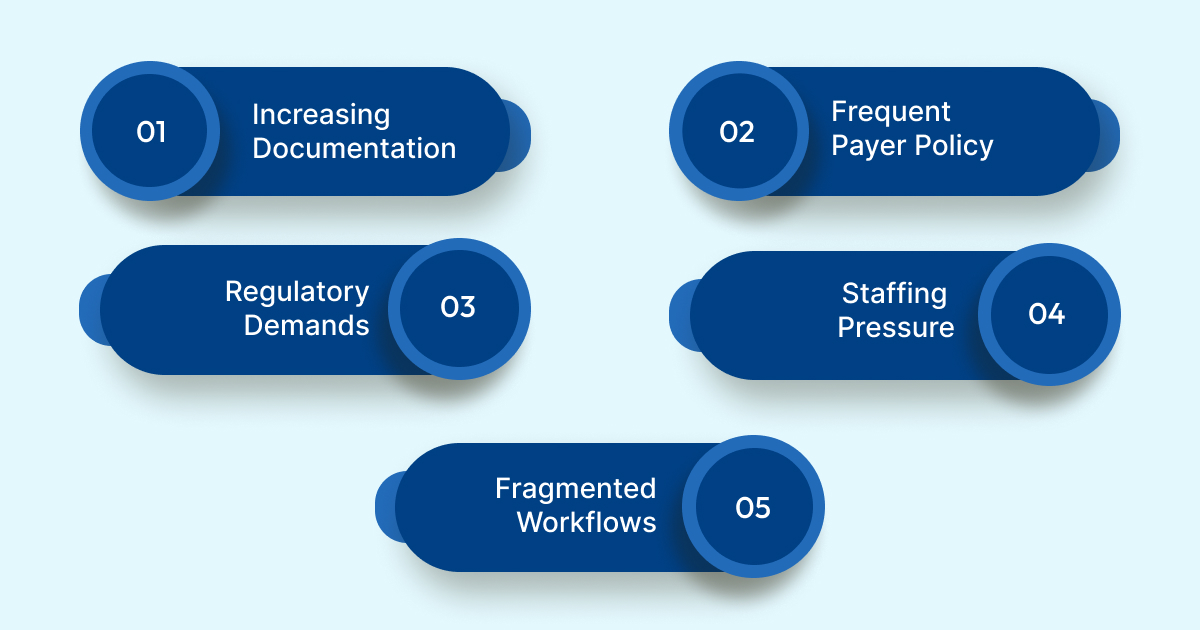
- Increasing Documentation Complexity: Clinical documentation now requires greater depth to support medical necessity and accurate code assignment. Missing or unclear details frequently result in payer requests for clarification.
- Frequent Payer Policy Updates: Coverage rules change more often across commercial plans, Medicare Advantage, and Medicaid programs. Rapid shifts make it difficult for teams to maintain alignment with current requirements.
- Growing Coding and Regulatory Demands: ICD-10-CM, CPT, and HCC v28 updates require more precise interpretation. Inconsistent application of these rules increases the likelihood of payer disputes.
- Staffing Pressure: Organizations continue to face shortages of experienced coders and CDI specialists. Higher workloads increase the risk of overlooked elements in documentation review.
- Fragmented Workflows: Manual processes struggle to manage complex encounter data at scale. Without automated checks, preventable issues often pass through to claim submission.
AI-enabled platforms like RapidClaims help address these challenges by improving documentation clarity and supporting consistent code application.
Root Causes Behind Preventable Denials
Preventable denials often originate from recognizable patterns across coding, documentation, and administrative workflows.
Coding and Documentation Issues
Common contributors include:
- Limited clinical detail that prevents accurate ICD-10-CM specificity
- Incorrect or outdated CPT code selection
- Documentation that does not support medical necessity
- Missing indicators needed for HCC capture
These issues lead to discrepancies that payers flag during claim review.
Front-End Data Accuracy
Denials frequently stem from:
- Incorrect demographic or insurance information
- Eligibility conflicts
- Missing or expired authorizations
Although they occur before coding, these issues impact first-pass claim performance.
Authorization and Medical Necessity Requirements
With stricter utilization management, payers increasingly deny services lacking required authorizations or adequate supporting documentation.
Timing and Submission Issues
Process-related problems include delayed submissions, inconsistent charge capture, and absent documentation required at billing.
Where AI Helps
Platforms like RapidClaims identify documentation gaps, strengthen code accuracy, and apply payer rules during review, reducing denials that originate upstream.
See how your denial rate compares to peer benchmarks and where preventable revenue leakage occurs. RapidClaims can analyze a sample of claims and provide an AI driven denial risk model that highlights exactly which documentation and coding workflows need attention first.
How AI Enhances Medical Coding to Lower Denials
AI strengthens denial prevention by examining clinical information more deeply and consistently than manual review.
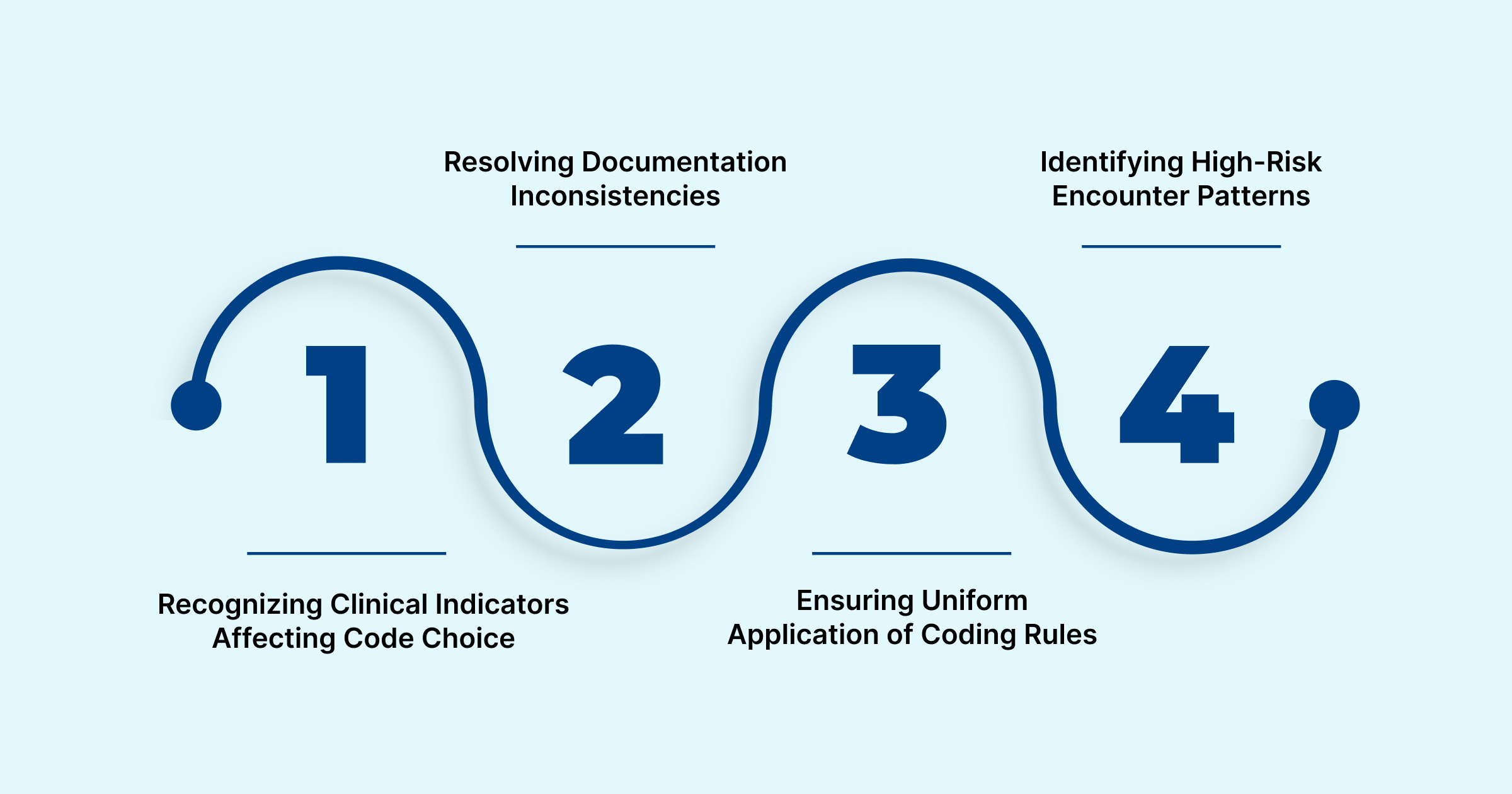
- Recognizing Clinical Indicators Affecting Code Choice: AI identifies clinical details that influence diagnosis specificity, procedure context, and HCC assignment, ensuring accurate representation of encounter complexity.
- Resolving Documentation Inconsistencies: By comparing information across notes, labs, and structured fields, AI detects mismatches that may create coding discrepancies.
- Ensuring Uniform Application of Coding Rules: AI applies guidelines consistently across encounters, minimizing variation that leads to payer challenges.
- Identifying High-Risk Encounter Patterns: AI highlights encounter types with higher likelihood of payer review, helping teams focus QA activities where they are most effective.
RapidClaims in Practice
RapidClaims uses advanced NLP and rules-based coding intelligence to surface missing elements, align documentation, and recommend accurate codes.
Practical Steps for Implementing AI in RCM Workflows
Effective AI adoption depends on clean data flow, clear review steps, and ongoing oversight. When these elements are in place, organizations see stronger improvements in accuracy and denial prevention.
- EHR Integration: AI needs complete encounter data to work reliably. Integrations through HL7 and FHIR allow real-time access to notes, labs, and procedure details, which supports continuous review instead of end-of-cycle processing.
- Structured QA Review: Teams assign review tiers for encounters flagged by the AI. This keeps attention focused on charts with higher complexity or documentation questions without slowing the entire workflow.
- Compliance Consistency: Regular updates to ICD-10-CM, CPT, and HCC v28 rules must be reflected in both AI logic and reviewer processes. This reduces the risk of outdated coding and supports audit readiness.
- Performance Monitoring: Tracking accuracy trends and common exception types helps teams improve documentation habits and reduce recurring denial patterns.
RapidClaims in Practice
RapidClaims connects directly to EHR data, organizes coder review workflows, and applies current coding and risk adjustment rules. This creates a structured pathway that supports accurate, consistent coding and stronger denial prevention.
Operational and Financial Impacts of Reducing Claim Denials
AI-supported coding and documentation review strengthens both daily operations and long-term financial performance. The improvements come from increased accuracy, higher throughput, and fewer downstream interruptions in the claim cycle.
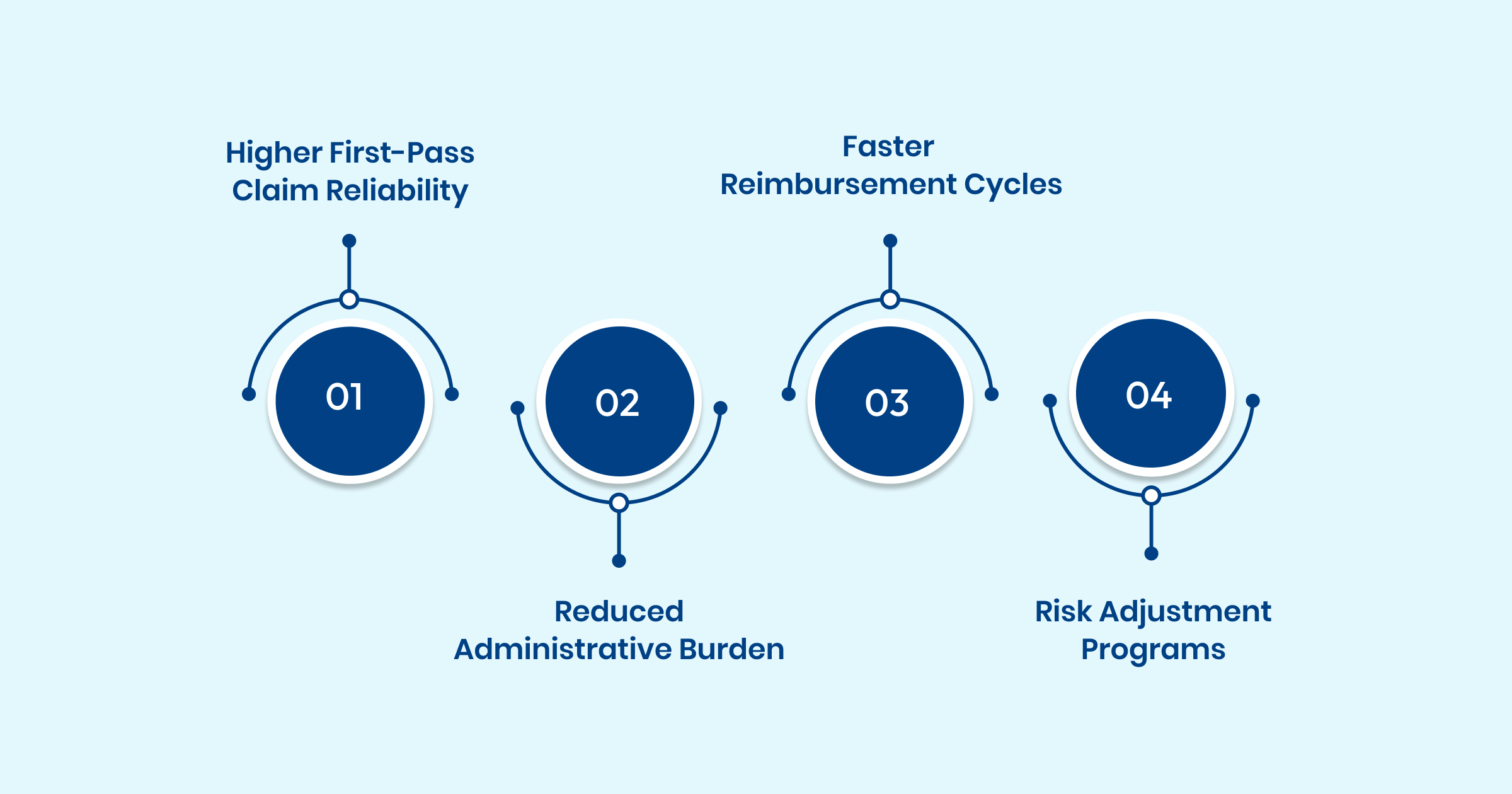
- Higher First-Pass Claim Reliability: More complete and consistent encounters reduce the number of claims routed back to coding or clinical documentation teams. This lowers rework volume and speeds overall claim progression.
- Reduced Administrative Burden: AI handles large portions of documentation review and code validation, which frees coders and CDI specialists to focus on complex encounters. Teams spend less time correcting preventable issues and more time supporting high-value cases.
- Faster Reimbursement Cycles: Cleaner submissions shorten payer review times and reduce the delays associated with avoidable denials. Organizations see faster revenue realization and fewer cash-flow disruptions.
- Stronger Support for Risk Adjustment Programs: Accurate capture of clinical indicators linked to HCC categories improves risk score integrity for Medicare Advantage populations. This helps organizations maintain program accuracy and reduces the likelihood of post-payment disputes.
RapidClaims’ Contribution
RapidClaims enhances these outcomes by providing consistent documentation analysis, precise coding recommendations, and payer-aware validation before submission. The result is a more stable operational cadence and a measurable reduction in preventable denial activity.
Use Cases Across Healthcare Organizations
AI-driven coding and documentation review supports a wide range of operational needs across different care environments. Each setting benefits in distinct ways based on encounter volume, clinical complexity, and payer mix.
Health Systems Managing High Chart Volume
Large systems use AI to coordinate coding activity across multiple service lines. Automated consistency checks help align documentation standards between hospitals, clinics, and specialty groups, which reduces variation in coding quality.
Multi-Specialty Medical Groups
Groups with diverse specialties rely on AI to manage variation in documentation styles and encounter structures. Systems surface specialty-specific coding considerations that are not always captured in manual review, particularly for cardiology, behavioral health, and orthopedic services.
Outpatient Surgery and Procedural Centers
AI supports centers with high-cost procedures by confirming that required clinical details, authorizations, and supporting documentation are present before billing. This strengthens claims for services that often receive payer scrutiny.
Emergency and Urgent Care Settings
These environments produce fast-paced documentation that varies widely between clinicians. AI assists by highlighting missing clinical elements and identifying inconsistencies that may affect coding accuracy for high-volume, rapid-turnaround encounters.
Medicare Advantage and Risk Adjustment Teams
Risk adjustment teams use AI to ensure accurate capture of clinical indicators linked to HCC categories. This supports reliable risk scoring and reduces the likelihood of retrospective documentation challenges.
RapidClaims Across Use Cases
RapidClaims adapts to each setting by analyzing encounter content, identifying documentation needs, and supporting accurate code selection. This helps organizations maintain consistent performance even when encounter types and operational demands differ.
Ready to reduce preventable denials and strengthen first pass performance? RapidClaims combines AI supported coding, documentation integrity, smart edits and payer aware validation to improve claim accuracy before submission. Request a personalized pilot to see how organizations achieve higher clean claim rates, lower denial volume and measurable improvements in cash flow.
Conclusion
Denial prevention in 2025 requires stronger documentation consistency, precise code selection, and reliable review processes across every care setting. AI-enabled coding systems now play an essential role in supporting these goals by analyzing encounter data more thoroughly and identifying issues that manual workflows often miss. When organizations combine accurate documentation, consistent rule application, and structured oversight, they strengthen first-pass claim quality and reduce operational strain on coding and revenue cycle teams.
AI platforms such as RapidClaims help organizations move toward this model by supporting accurate, compliant coding and improving the reliability of every claim submitted.
See how RapidClaims can help your organization improve documentation completeness, strengthen coding accuracy, and reduce preventable denials. Request a personalized demo to explore how AI can support your RCM team’s goals.
FAQs
Q: What is the average claim denial rate in healthcare?
A: Most providers fall between 5 percent and 10 percent, although some organizations report higher rates depending on payer mix and encounter complexity. This range represents common industry benchmarks cited across RCM resources.
Q: Is a 10 percent denial rate considered high?
A: A denial rate at or above 10 percent is typically viewed as a sign that documentation, coding, or front-end processes need review. Many revenue cycle teams use this threshold as an indicator that deeper analysis is required.
Q: How often are claim denials linked to documentation or coding errors?
A: A significant portion of denials are tied to missing clinical detail, incomplete documentation, or incorrect code selection. These issues continue to be among the most common contributors to preventable denials.
Q: Do denial rates vary by type of health plan?
A: Yes. Commercial payers often show higher initial denial activity for eligibility or authorization issues, while Marketplace and Medicare Advantage plans can vary widely based on their review criteria and documentation rules.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








