How Behavioral Health RCM Differs From Traditional RCM?

Behavioral healthcare differs from regular healthcare in many aspects. The treatment methods are designed to rehabilitate patients with behavioral issues. Hence, the duration is longer, patient progress is prioritized over complete recovery, and therapy session outcomes are evaluated to measure success rates. On the other hand, traditional medicine deals with procedures with well-defined, fixed outcomes. The administrative tasks involved in both fields differ, as conventional medical practices and behavioral health treatments are distinct. RCM, being the heart of revenue collection for any healthcare system, also changes accordingly. In this article, we explore a few key points that distinguish behavioral RCM systems from conventional healthcare RCM and how they affect reimbursements for both parties.
What Is Behavioral RCM?
Behavioral RCM deals with the administrative and clinical aspects of behavioral healthcare, which includes the treatment of patients fighting behavioral and mental health issues. It also covers care for patients with substance abuse issues. Behavioral healthcare follows a more holistic and gradual care model as opposed to the conventional healthcare system. This forms the foundation for behavioral healthcare RCM, which is designed to streamline tasks such as documentation, coding, payer rules, reimbursement timelines, etc.
Although the core purpose of RCM in healthcare is to optimize administrative and billing tasks for faster reimbursements and just payments, behavioral RCM differs from traditional medicine RCM systems due to the distinct nature of caregiving and treatment followed by behavioral healthcare practitioners and institutions.
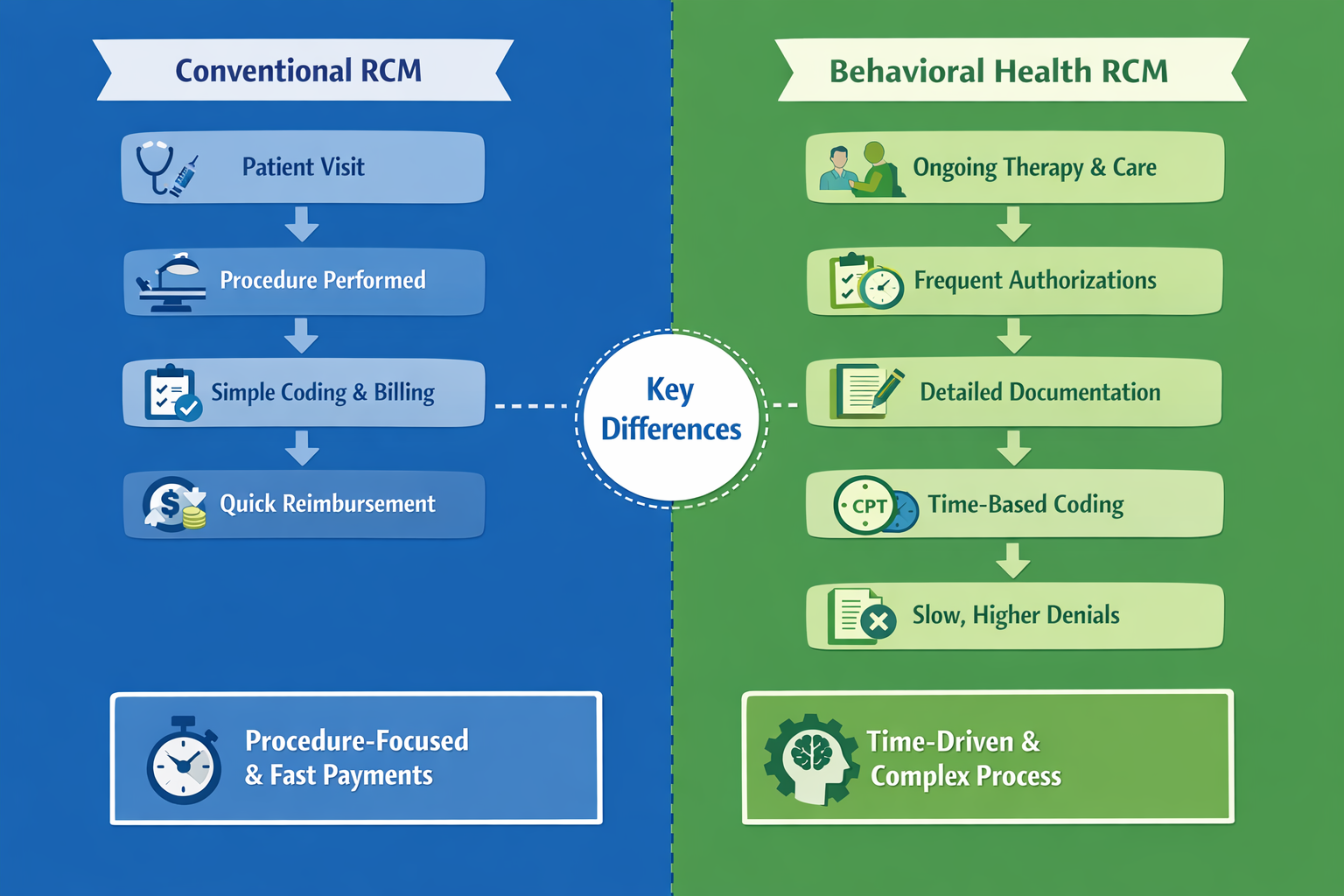
Difference between behavioral and traditional RCM systems
Before we deep dive into behavioral RCM, here is a quick recap of what conventional RCM systems are like. In conventional revenue cycle management systems, various medical procedures with well-defined actions are recorded using the CPT and ICD-10 codes. These medical procedures deliver expected outcomes within defined time periods. For example, at the end of an angioplasty procedure, a patient’s bodily functions are expected to be back to normal within a few days to a month. Conventional RCM systems are designed to accommodate the administrative requirements of traditional medical procedures.
Behavioral medicine deals with mental health, where a patient’s progress is considered to measure the effectiveness of a particular treatment plan. The behavioral medicine care model is fundamentally different from conventional medicine. Hence, the administrative process used by mental health and substance abuse disorder practitioners is different from the traditional healthcare administrative process. The ICD-10 and CPT code sets for behavioral treatments are also different. These key differences call for a separate behavioral RCM system. The above table clearly highlights the key differences between these RCM systems.
Difference in Care Delivery Models
Behavioral healthcare systems function around the primary purpose of gradual but steady progress in a patient’s condition. Mental health treatments take time and effort. This is reflected in behavioral RCM systems. The treatments often unfold over weeks, months, or even years. There is no single procedure that defines successful outcomes. Instead, care focuses on:
- Treatment plans
- Progress over time.
- Clinical outcomes depend on behavioral progress and mental health stability.
Unlike the olden days, behavioral healthcare focuses on holistic, patient-centric treatment methods. Traditional medicine follows set protocols for different types of physical ailments and traumatic injuries. This difference affects how RCM systems function in both environments. Traditional RCM systems are built for short-term processes, while behavioral RCM systems must cater to long-term, session-based procedures.
Coding and Disease Complexity
In behavioral healthcare, therapy and group sessions are billed. Since these treatments are time-based, billing for the services can get tricky. Hence, individual CPT codes are assigned to therapy sessions of varying durations. For example, 30-minute sessions are defined by a specific CPT code; sessions that last for 60 minutes are defined by a different CPT code. Although the rendered service is therapy, patients are charged based on the time they spend in therapy. Any mismatch of the entered code with the time duration can cause a claim rejection from the insurance company. In behavioral health, accurate CPT and ICD-10 codes form the foundation of successful claim and billing systems. However, it is not as straightforward as general medical billing systems. Behavioral RCM systems must accommodate these requirements to ensure timely reimbursements.
In the case of traditional medicine RCM systems, the medical procedures are well-defined and less dependent on the diagnostic outcomes.
Why This Matters For Revenue?
Behavioral health billing is more detailed, it is important to include a detailed description of the therapy sessions to ensure accurate claims processing and timely reimbursements. The biggest challenge in behavioral health billing is ensuring that the entered codes match the services mentioned in the claims documents.
Behavioral health RCM is highly detailed, time-driven and highly sensitive. Traditional coding is more procedure-driven, and predictable. The possibility of hard denials spikes up if the codes entered in the system do not match with the treatment being mentioned there.
Prior Authorizations
Due to the unpredictable nature of behavioral treatment plans, hospitals and mental health practitioners are often required to ask for prior permission from insurance companies before they can start with a treatment method. Prior authorization is required for the following:
- Individual and group therapy sessions.
- Inpatient behavioral health admissions.
- Intensive Outpatient programs (IOP).
- Partial Hospitalization Programs (PHP).
- Long-term or ongoing treatment plans.
Medical Necessity Is Subjective
Treatment plans in behavioral healthcare are centered around a patient’s mental ability to adapt to a treatment plan. Hence, recovery is very gradual. Due to this, healthcare providers must employ behavioral RCM systems that are designed to cater to multiple pre-authorizations and payer inquiries, questioning the necessity of a particular treatment method. Since the evaluation of medical necessity cannot be supported by procedures such as imaging and blood tests, behavioral health practitioners establish proof of necessity with:
- Clinical notes and the patient’s mental history.
- Timely risk assessments.
- Treatment plans.
- Patient progress.
The subjective parameters influence the outcome of behavioral healthcare claim registration, because payers take longer than expected to analyze, assess and finally decide on approving certain claims.
Detailed Documentation Can Be Tedious
Behavioral treatments involve detailed documentation that describe each phase of a patient’s condition. As time progresses, observations from therapy sessions and a patient’s attendance provide sufficient data to insurance companies. However, the biggest issue in behavioral healthcare is that a patient can relapse at any point of time, rendering any advanced treatment approved by insurance companies to be ineffective. AI-powered RCM systems like RapidClaims leverage machine learning to interpret important points from session descriptions and assign appropriate CPT codes, ensuring that payers do not find loopholes in claim registration.
Slower Reimbursements and Cash Flow
Regular medical RCM systems are programmed to record medical procedures that produce the desired results in a set amount of time. On the other hand, behavioral medicine does not have a fixed list of procedures that guarantee a certain outcome. Behavioral issues are tied to a patient's personality, in addition to other physical attributes. However, while submitting claims, it becomes difficult to point out and prove to insurance companies why a certain treatment failed.
This issue has been the cause of delayed reimbursements. Whenever the insurance company is not convinced of a healthcare provider’s case, the chances of claim rejection increase.
The only solution to this problem is to place strong workflows that ensure seamless transitions from one point to another.
Patient Engagement and Collections
Individuals with behavioral issues must attend therapy sessions regularly. Their interaction and responsiveness provide caregivers with sufficient data to determine their progress. In reality, such patients require multiple sessions before they even start engaging with their therapists. Due to the intensity and complexity of mental health issues, healthcare facilities often find it challenging to receive just reimbursements from insurance companies. This is where behavioral healthcare RCM systems like RapidClaims, which are powered by AI and related technologies, come in handy. This system leverages machine learning to interpret doctor’s notes to extract session descriptions and assign appropriate CPT codes.
In traditional RCM, many medical services are one-time encounters where patient balances can be collected at or near the time of service.
Behavioral RCM must balance financial performance with patient-centric care.
Payer Policies Variability and Compliance
The coverage rules of insurance companies for behavioral health vary with respect to the following factors:
- Payer
- State
- Diagnosis
- Provider type
Even with mental health parity laws in place, there are high chances of payment rejection owing to confusion regarding the authorization of certain mental health services.
RapidClaims RCM is programmed to constantly check payer-specific rules and regulations to avoid claim rejections.
Why One-Size-Fits-All RCM Systems Fall Short?
Traditional RCM systems are pre-fed with standardized codes for general medical procedures. Behavioral health RCM systems must be designed to facilitate timely payer policy checks to ensure compliance and timely payments.
RapidClaims RCM systems leverage AI to enable:
- Real-time eligibility checks.
- Automated authorization alerts.
- Documentation audits.
- Denial prediction and prevention
Conclusion
Behavioral RCM and traditional RCM systems are fundamentally different because the care models are distinct. Time-based authorization assessments, subjective medical necessity, frequent authorizations, and heavy documentation present challenges that traditional RCM systems cannot handle. With the growing demand for mental health services, the need for a well-programmed behavioral RCM is higher than usual. The RapidClaims system is powered by AI-based algorithms that leverage machine learning to intuitively navigate behavioral health bills, ensuring compliance and timely payments.
FAQs
How is behavioral health RCM different from traditional systems?
Behavioral health RCM is different from he traditional systems due to distinct care delivery models. Behavioral treatments are more subjective and require heavy documentation, which can be complicated for traditional RCM systems. Behavioral health RCM systems must be designed to accommodate these requirements to ensure compliance and timely reimbursements.
Why do behavioral health claims take longer to be processed?
Behavioral healthcare follows a different care model than the traditional medical care models. They are more subjective and the services are time-based, and recorded over time. Patients are billed based on the longevity of their sessions (1 hour, 2 hours, etc) with specific CPT codes defining therapy of different durations. Behavioral RCM systems must be able to balance between the financial requirements and patient-centered care delivery while adhering to compliance requirements.
How does RapidClaims RCM help with behavioral healthcare billing?
RapidClaims RCM leverages AI-based algorithms to automate crucial activities such as behavioral medical coding. The system uses machine learning to parse clinical notes and assign the appropriate CPT code for each therapy session category. Real-time checking of compliance regulations is conducted regularly to ensure adherence to behavioral healthcare rules.
.png)
Ayeesha Siddiqua
Ayeesha Siddiqua is a highly experienced medical coding professional with 22 years of expertise in E/M Outpatient, Radiology, and Interventional Radiology (IVR), ensuring coding accuracy, regulatory compliance, and optimized reimbursements at RapidClaims.
Latest Post
Related Post

What Is Charge Capture and How Charge Capture Audits Streamline the Process

What Are Clinical Workflows and Why Do They Matter in Modern Healthcare Systems?

What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
Top Products

%201.png)





