.webp)
ICD-10 Coding Hypertension and Chronic Kidney Disease Explained

Hypertension and chronic kidney disease (CKD) are common comorbidities in the United States, often occurring together and complicating patient care. According to the 2024 CDC report, about 14% of U.S. adults, roughly 35.5 million people, have CKD, with hypertension being a leading contributor.
Accurate ICD-10 coding for these conditions is essential for proper reimbursement, quality reporting, and regulatory compliance. The CMS and AHIMA provide detailed guidelines to support consistent and correct coding practices.
In this blog, you'll learn step-by-step how to code hypertension with CKD using ICD-10 and discover practical tips to avoid common errors.
TL;DR (Key Takeaway)
- Hypertension and CKD frequently coexist, requiring accurate ICD-10 coding to capture patient comorbidities and severity.
- Combination codes (I12, I13, I11) plus N18 stage codes are essential for proper risk adjustment and reimbursement.
- Common coding errors include misclassifying hypertension, omitting CKD stage, and missing comorbidities; always verify lab results and documentation.
- Accurate coding supports audit-readiness, compliance with CMS/AHIMA guidelines, and informs care management for high-risk patients.
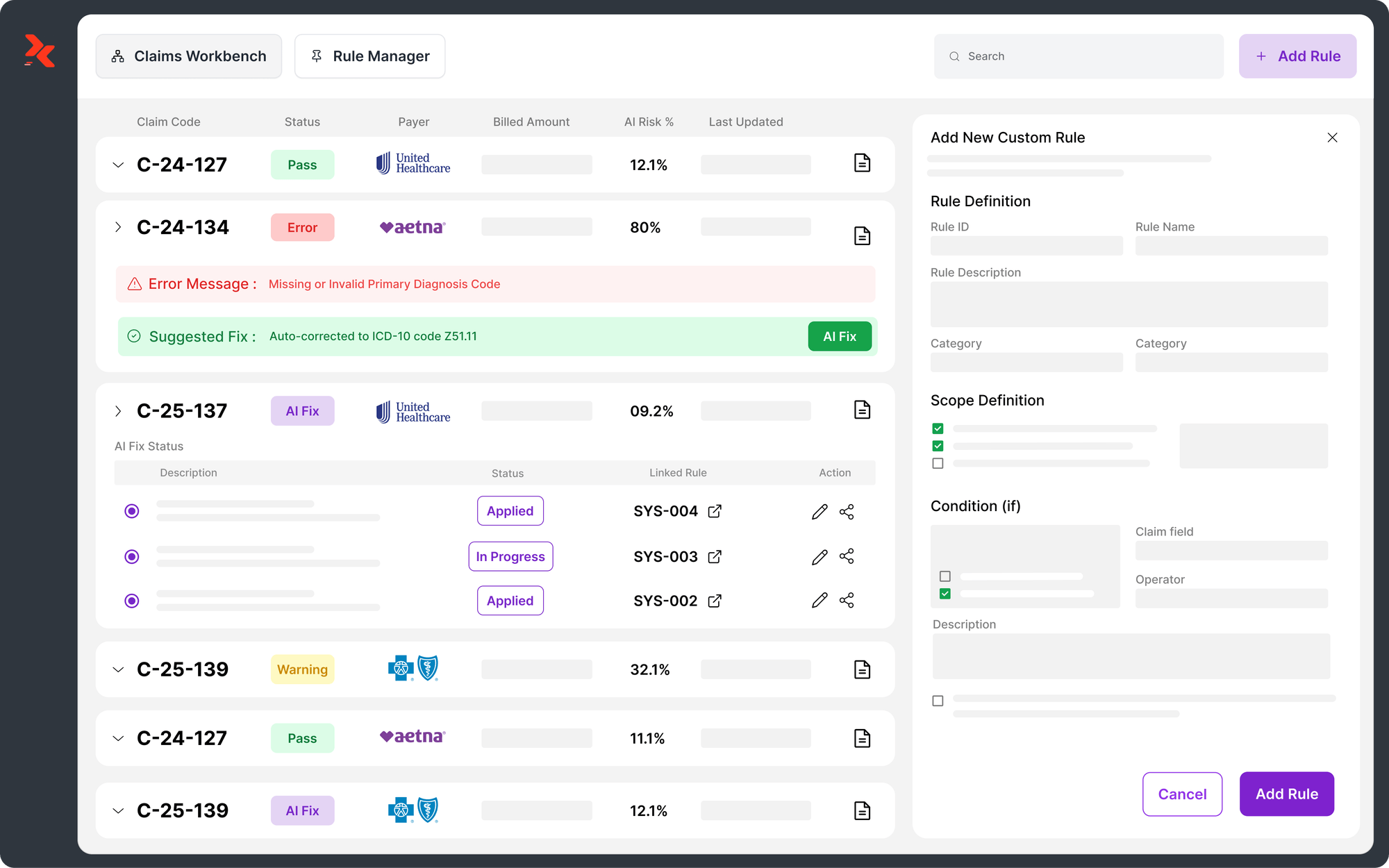
- AI-powered solutions like RapidClaims streamline coding, reduce denials by 70%, improve HCC capture, and optimize revenue while saving clinician time.
Table of Contents:
- What are Hypertension and Chronic Kidney Disease?
- Documenting and Coding Hypertensive Diseases in ICD-10
- Risk Adjustment and Reimbursement for Hypertension & CKD
- ICD-10 Coding Errors and Best Practices for Hypertension & CKD
- Conclusion
- Frequently Asked Questions (FAQs)
What are Hypertension and Chronic Kidney Disease?
Hypertension, or high blood pressure, is a chronic condition where the force of blood against arterial walls remains consistently elevated. Over time, this increases the workload on the heart, damages blood vessels, and raises the risk of cardiovascular complications. It can be classified as:
- Primary (essential) hypertension: no identifiable cause.
- Secondary hypertension: caused by underlying conditions such as CKD, endocrine disorders, or certain medications.
Chronic Kidney Disease (CKD) is a progressive loss of kidney function over time. The kidneys are responsible for filtering waste, balancing fluids and electrolytes, and regulating blood pressure. CKD is categorized into five stages based on estimated glomerular filtration rate (eGFR), with stage 5 being end-stage renal disease (ESRD). Hypertension is both a cause and a consequence of CKD:
- High blood pressure can damage kidney blood vessels and accelerate CKD progression.
- Reduced kidney function can further elevate blood pressure, creating a cycle of worsening disease.
Now, let’s take a closer look at coding hypertension and chronic kidney disease accurately using ICD-10.
Documenting and Coding Hypertensive Diseases in ICD-10

Hypertension has a relatively small set of ICD-10 codes, with nine codes for primary hypertension and five codes for secondary hypertension. This makes coding hypertension simpler compared to many other conditions. ICD-10 also no longer distinguishes between “benign” and “malignant” hypertension, which aligns better with the clinical understanding that hypertension is never truly benign.
1. Hypertensive Chronic Kidney Disease (I12)
When a patient has hypertension and CKD, ICD-10 presumes a causal relationship. This condition is classified as hypertensive chronic kidney disease. There are two main codes:
- I12.0 – Hypertensive CKD with stage 5 CKD or end-stage renal disease (ESRD)
- I12.9 – Hypertensive CKD with stage 1–4 CKD or unspecified CKD
Both codes require an additional N18 code to specify the stage of CKD, usually based on the most recent estimated glomerular filtration rate (eGFR):
- N18.1 – CKD, stage 1
- N18.2 – CKD, stage 2 (mild)
- N18.3 – CKD, stage 3 (moderate)
- N18.4 – CKD, stage 4 (severe)
- N18.5 – CKD, stage 5
- N18.6 – End-stage renal disease
- N18.9 – CKD, unspecified
Example: A 56-year-old patient with longstanding hypertension has an eGFR of 40 mL/min/1.73m². The correct codes would be I12.9 and N18.3.
2. Hypertension with Heart Disease (I11)
If hypertension is present along with heart disease, providers must document whether a causal relationship exists. ICD-10 offers two codes for hypertensive heart disease:
- I11.0 – Hypertensive heart disease with heart failure
- I11.9 – Hypertensive heart disease without heart failure
Heart failure type and acuity are coded separately using the I50 series:
- I50.1 – Left ventricular failure
- I50.2 – Systolic (congestive) heart failure
- I50.3 – Diastolic (congestive) heart failure
- I50.4 – Combined systolic and diastolic failure
- I50.9 – Heart failure, unspecified
3. Hypertension, CKD, and Heart Disease (I13)
For patients with all three conditions, ICD-10 requires:
- Documenting the relationship between hypertension and heart disease
- Presuming a causal relationship between hypertension and CKD
- Additional codes for CKD stage (N18) and heart failure type/acuity (I50)
Codes are numerically arranged by CKD stage rather than heart failure:
- I13.0 – Hypertensive heart and CKD with heart failure and stage 1–4 CKD
- I13.10 – Hypertensive heart and CKD without heart failure, stage 1–4 CKD
- I13.11 – Hypertensive heart and CKD without heart failure, stage 5 CKD/ESRD
- I13.2 – Hypertensive heart and CKD with heart failure, stage 5 CKD/ESRD
4. Secondary Hypertension (I15)
Some patients may have secondary hypertension due to underlying conditions. ICD-10 codes include:
- I15.0 – Renovascular hypertension
- I15.1 – Hypertension secondary to other renal disorders
- I15.2 – Hypertension secondary to endocrine disorders
- I15.8 – Other secondary hypertension
- I15.9 – Secondary hypertension, unspecified
The underlying condition must also be coded, usually listed first.
5. Tobacco Use and Hypertensive Diseases
For patients with hypertension, an additional code is required if there is tobacco use or exposure:
- F17 – Nicotine dependence (with subcategories)
- Z72.0 – Problems related to lifestyle, tobacco use
- Z77.22 – Exposure to environmental tobacco smoke
- Z87.891 – Personal history of nicotine dependence
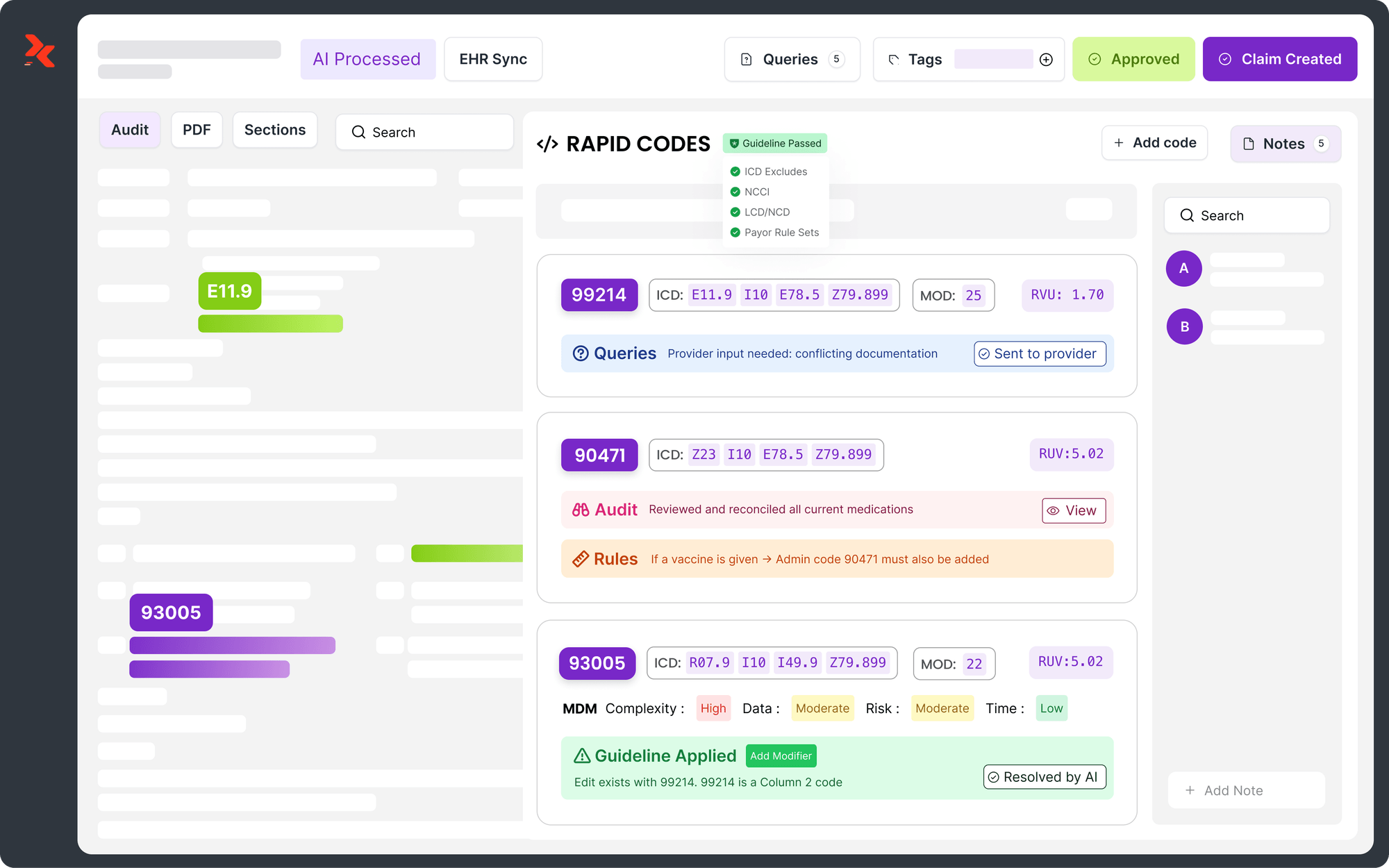
With the complexities of ICD-10 coding for hypertension and chronic kidney disease, manual processes can increase errors. AI-powered solutions, such as RapidClaims, help healthcare teams automate coding and reduce denials. Using modules such as RapidCode, RapidCDI, and RapidScrub, providers can achieve 96% coding accuracy and increase HCC capture by 24%. They can also process charts at up to 1,000 per minute, all while maintaining audit-ready compliance.
Also Read: Differences and Basics of ICD-10 and CPT Codes
Risk Adjustment and Reimbursement for Hypertension & CKD
Accurate coding of hypertension and chronic kidney disease is essential in value-based care models, where reimbursement is closely tied to patient complexity and risk adjustment scores. Proper documentation ensures fair payment for comorbid patients and accurately reflects the severity of illness for regulatory reporting purposes.
Below are a few key points to consider:
- Influences Risk Adjustment Scores
Correct ICD-10 coding, such as I13.0 for hypertensive heart and CKD with heart failure, is essential. Adding N18.3 for stage 3 CKD ensures the patient’s Hierarchical Condition Category (HCC) score is accurately captured. This score directly impacts provider reimbursement under CMS programs.
- Optimizes Reimbursement
Properly capturing comorbidities ensures that providers receive payment reflecting the complexity of care. It also helps avoid underpayment and reduces compliance risks.
- Highlights Patient Severity and Comorbidities
Accurate coding signals the presence of multiple interacting conditions, such as hypertension, CKD, and heart failure. This is critical for risk-adjusted outcome measurement and quality-of-care assessments.
- Supports Compliance and Audit-Readiness
Documented and coded comorbidities provide clear evidence for audits, reduce the risk of claim denials, and demonstrate adherence to CMS and AHIMA guidelines.
- Enhances Care Management and Population Health
Risk-adjusted data derived from accurate coding informs care coordination, disease management programs, and preventive interventions for high-risk patients.
By implementing precise coding practices, healthcare organizations can maximize reimbursement, improve risk adjustment accuracy, and maintain regulatory compliance, while providing a clear picture of patient health complexity.
Accurate ICD-10 coding for hypertension and CKD is critical for achieving these goals. RapidClaims streamlines coding, smart edits, and denial prevention, delivering a 98 % clean-claim rate and 30-day time-to-value. Its AI-driven tools save physician time, enhance HCC capture, and reduce administrative burden, helping healthcare teams focus on high-quality patient care.
ICD-10 Coding Errors and Best Practices for Hypertension & CKD
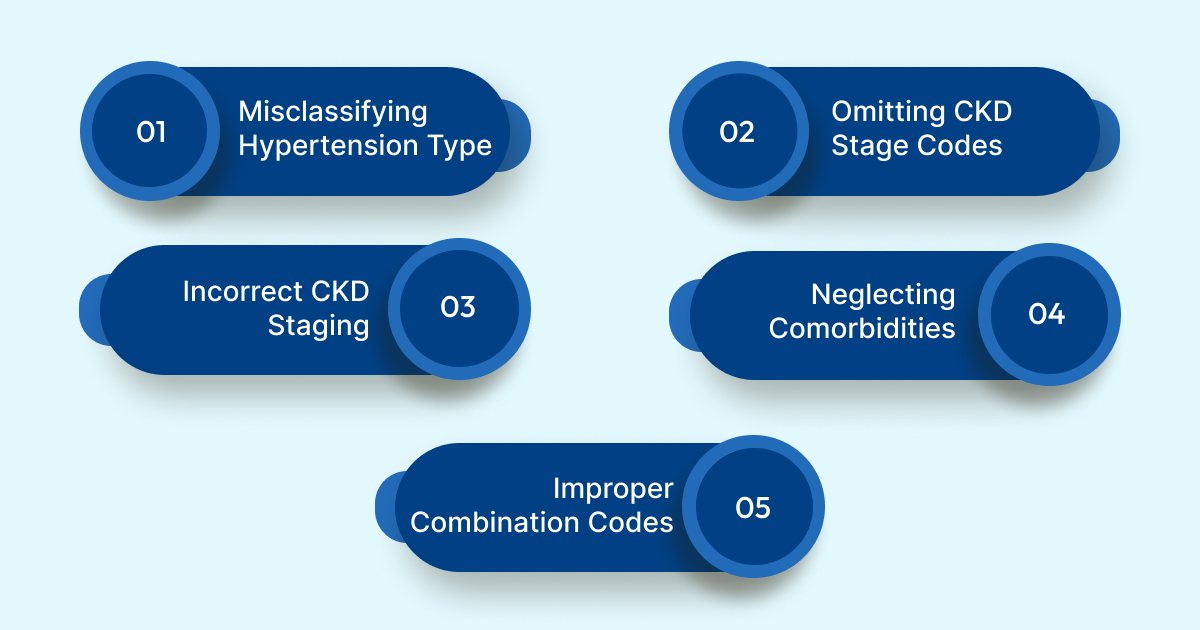
Accurate ICD-10 coding for hypertension and chronic kidney disease demands precision and careful review of clinical documentation. Common coding errors can lead to incorrect reimbursement, flawed risk adjustment, and compliance issues, making attention to detail critical for maintaining accurate patient records and audit readiness.
Below are a few of the most frequent coding challenges and best practices to address them:
1. Misclassifying Hypertension Type: Coding primary hypertension as secondary (or vice versa) can lead to incorrect risk adjustment and claim denials.
- Best Practice: Carefully review clinical documentation to determine the correct type before assigning ICD-10 codes. Query the provider if the documentation is unclear.
2. Omitting CKD Stage (N18) Codes: Failing to assign an additional N18 code can obscure the severity of CKD and impact HCC scores.
- Best Practice: Always verify the most recent eGFR or lab results and include the appropriate N18 stage code.
3. Incorrect CKD Staging: Using outdated or inaccurate lab values can result in misclassification of CKD stage, leading to undercoding or overcoding.
- Best Practice: Ensure documentation reflects current and repeat testing when available to assign CKD stage accurately.
4. Neglecting Comorbidities: Conditions like heart failure, tobacco use, or hypertensive heart disease may require additional ICD-10 codes. Omitting them reduces risk adjustment accuracy.
- Best Practice: Review patient charts thoroughly and code all relevant comorbidities. Include lifestyle factors such as tobacco use (F17.x, Z72.0) to improve risk-adjusted scoring.
5. Failing to Use Combination Codes Properly: Not applying codes such as I13.x for hypertension with heart disease and CKD can misrepresent disease relationships.
- Best Practice: Use combination codes when documentation shows a causal relationship, and supplement with CKD stage (N18) and heart failure type (I50) codes as needed.
Pro Tip: Always double-check clinical documentation, lab results, and comorbid conditions before assigning ICD-10 codes to ensure accuracy. Accurate combination and stage-specific coding ensures proper reimbursement, supports risk adjustment, and keeps your claims audit-ready.
Conclusion
Manual coding of hypertension and chronic kidney disease can be complex and error-prone, potentially affecting reimbursement, risk adjustment, and compliance. Accurate ICD-10 coding ensures patient comorbidities are properly documented, supports value-based care, and helps healthcare providers capture the true complexity of patient health.
With AI-powered platforms like RapidClaims, healthcare teams can automate coding workflows, reduce manual errors, and ensure claims are processed faster and more accurately. RapidClaims also helps maintain audit-ready documentation, optimize reimbursement, and support regulatory compliance.
Streamline your coding processes today with RapidClaims to improve accuracy, boost revenue, cut denials by 70 %, and focus on delivering high-quality patient care. Request a Free Demo and see how RapidClaims can transform your coding workflow.
Frequently Asked Questions (FAQs)
1. How do I know if a patient’s elevated blood pressure requires coding as hypertension?
A. If a patient consistently records systolic ≥140 mmHg or diastolic ≥90 mmHg across multiple visits, it qualifies as hypertension. Sporadic or borderline readings should be coded as R03.0 (elevated blood pressure) until a formal diagnosis is documented. Proper documentation of progression from elevated readings to hypertension is critical for accurate ICD-10 assignment.
2. Can I code hypertension differently if the patient has multiple organ complications?
A. Yes. ICD-10 allows combination codes when complications involve the heart, kidney, or both. You must carefully review documentation to link hypertension causally to each organ issue. Using the correct combination of codes ensures risk-adjusted scores and avoids misrepresentation of comorbidities.
3. How do I handle coding if I suspect CKD but the eGFR is borderline?
A. When eGFR values are borderline or fluctuating, always document clinical judgment and consider repeating the test. Coding should reflect the most recently confirmed CKD stage to maintain accuracy. If uncertain, query the provider rather than assigning unspecified codes prematurely.
4. I sometimes notice discrepancies between lab-reported CKD stage and clinical notes; how should I code?
A. Always prioritize the provider-documented CKD stage in the medical record. Lab values alone may not account for all clinical nuances. Coders should reconcile lab results with physician notes and include N18 codes that match the confirmed stage of HCC for accurate reimbursement.
5. What should I do if I notice the patient is a smoker while coding hypertensive CKD?
A. Smoking or tobacco use can influence disease progression and may require additional ICD-10 codes (F17.x or Z72.0/Z87.891). Documenting tobacco use ensures risk adjustment captures lifestyle factors and supports preventive care strategies, enhancing both compliance and quality reporting.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
Related Post
Top Products
%201.png)