.webp)
Essential Guide to Healthcare Data Compliance & Protection

Healthcare organizations like yours are under constant pressure to protect sensitive patient data. Yet, breaches remain all too common. According to The HIPAA Journal, in 2024, more than 276 million individuals had their protected health information exposed or stolen, with nearly 760,000 records compromised every day. These breaches have significant financial and reputational consequences for healthcare organizations.
As a compliance officer, ensuring compliance with complex regulations while safeguarding data is an ongoing challenge. With the rise of digital records, EHR systems, and third-party services, maintaining secure practices becomes more difficult. The risk of non-compliance and data loss continues to grow every day.
In this blog, we’ll explore the key regulations shaping healthcare data security, the challenges your organization may face, best practices to stay compliant, and effective strategies for managing data breaches.
TL;DR (Key Takeaways)
- Healthcare data security requires adherence to multiple complex regulations like HIPAA, HITECH, and the 21st Century Cures Act.
- Data breaches in healthcare are costly and increasingly common, impacting both patients and organizations.
- Healthcare organizations face challenges like increasing cyber threats, data breaches, and third-party vendor risks.
- Best practices for data security include encrypting data, controlling access, training employees, and conducting regular audits.
- Effective incident response and post-breach analysis are critical for managing and mitigating the effects of data breaches.
Table of Contents:
- What is Data Compliance Management in Healthcare?
- Key Regulations Impacting Healthcare Data Compliance in the USA
- Challenges to Healthcare Data Compliance
- Best Practices for Healthcare Data Compliance And Security
- Steps to Manage Healthcare Data Breaches Effectively
- How RapidClaims Supports Healthcare Data Compliance
- Conclusion
What is Data Compliance Management in Healthcare?
Data compliance management in healthcare involves ensuring that all health-related data is handled according to regulatory standards. It covers areas such as patient privacy, data security, and the proper management of health records. This management is essential to meet legal requirements, such as HIPAA, and avoid severe penalties.
The goal is to protect sensitive patient information while ensuring its accuracy, accessibility, and confidentiality across healthcare systems. Effective data compliance management involves adopting policies and practices to manage risks associated with data breaches, unauthorized access, and regulatory violations.
With a clear understanding of data compliance management, it’s time to explore the key regulations influencing your healthcare organisation’s practices.
Key Regulations Impacting Healthcare Data Compliance in the USA
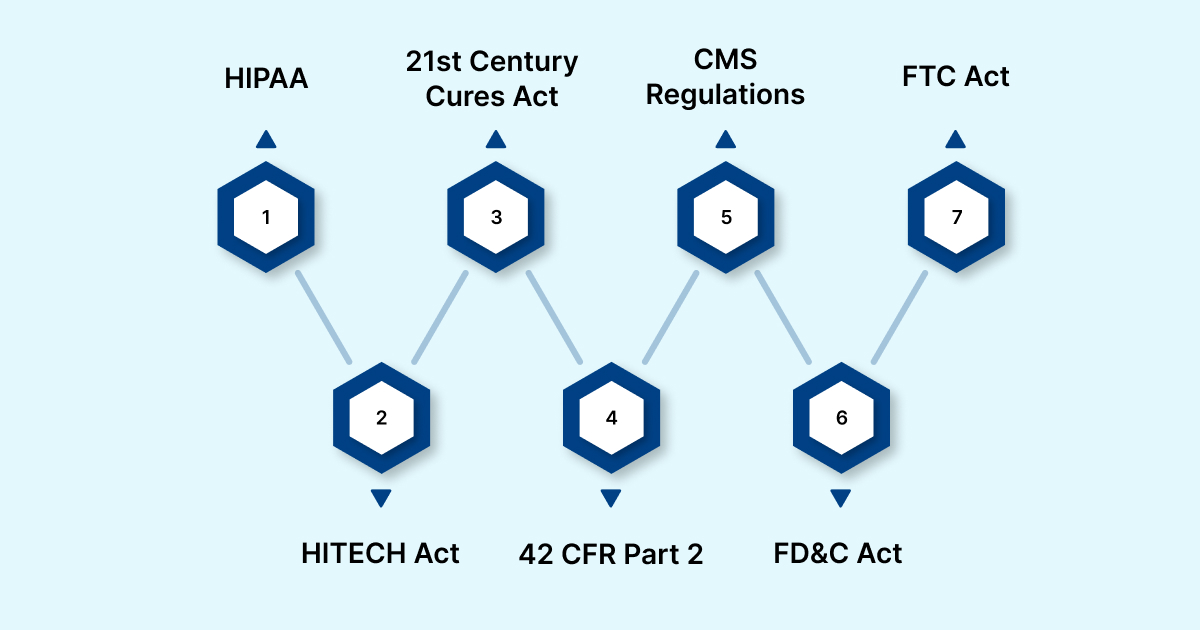
In the U.S., healthcare data security and compliance are guided by several key regulations aimed at protecting patient information and ensuring its proper handling. These regulations enforce strict standards for privacy, security, and data management, requiring healthcare providers to implement protective measures to reduce data breaches and maintain compliance.
Understanding these regulations is crucial for healthcare organizations to avoid penalties and ensure they meet all legal and security requirements. Below, we outline some of the most significant rules shaping healthcare data security and compliance:
1. HIPAA (Health Insurance Portability and Accountability Act)
HIPAA is the foundation of healthcare data security in the U.S., ensuring the privacy and security of health information. Here are the key aspects of HIPAA:
- Protects patient health information (PHI) from unauthorized access and breaches.
- Requires healthcare entities to implement security measures like encryption and access controls.
- Non-compliance can lead to hefty fines, ranging from $137,000 to $1.9 million annually.
2. HITECH Act (Health Information Technology for Economic and Clinical Health Act)
The HITECH Act strengthens HIPAA by promoting the use of EHRs and increasing penalties for data breaches. Here are the core elements of HITECH:
- Encourages healthcare organizations to adopt EHR systems for improved healthcare delivery and data management.
- Expands HIPAA enforcement to include data breaches by business associates.
- Mandates notification of breaches within 60 days of discovery.
3. 21st Century Cures Act
This act promotes health data interoperability and reduces barriers to the free flow of health information. Here’s how it impacts data sharing:
- Prohibits information blocking by healthcare providers and IT developers.
- Requires that electronic health records be accessible to patients through open application programming interfaces (APIs).
- Strengthens enforcement against providers who restrict lawful data sharing.
4. 42 CFR Part 2
This regulation specifically protects the privacy of substance use disorder (SUD) treatment records, offering stricter privacy protections than HIPAA. Here’s what 42 CFR Part 2 entails:
- Requires patient consent before sharing SUD-related health information.
- Ensures that treatment details are not disclosed without the patient’s explicit consent.
- Aligns specific provisions with HIPAA to improve compliance across treatment settings.
5. CMS Regulations (Centers for Medicare & Medicaid Services)
CMS regulations ensure healthcare organizations follow proper billing and coding practices for reimbursement under Medicare and Medicaid. Key aspects of CMS regulations include:
- Enforces quality reporting and data standards for telehealth and other healthcare services.
- Requires that healthcare providers adhere to the Promoting Interoperability Program for data sharing and reporting.
- Sets standards for data security in the context of government-sponsored health programs.
6. FD&C Act (Federal Food, Drug, and Cosmetic Act)
The FD&C Act governs the safety and effectiveness of medical devices, including software used for healthcare data management. Here’s what the FD&C Act regulates:
- Regulates Software as a Medical Device (SaMD) under the FDA’s oversight.
- Ensures that medical software, including AI-driven clinical decision tools, meets safety and effectiveness standards.
- Requires healthcare providers to comply with FDA regulations when using these devices in patient care.
7. FTC Act (Federal Trade Commission Act)
The FTC Act applies to non-HIPAA-covered entities such as health apps, wearables, and other digital health platforms. Here’s what it covers:
- Enforces consumer protection laws related to data privacy and security.
- Mandates that these entities must disclose their data practices and protect users' personal information.
- Includes provisions for the Health Breach Notification Rule, which requires health app companies to notify users of data breaches.
Now that you have an overview of the regulations, it’s essential to understand the challenges you’ll face in implementing them within your organisation.
Challenges to Healthcare Data Compliance
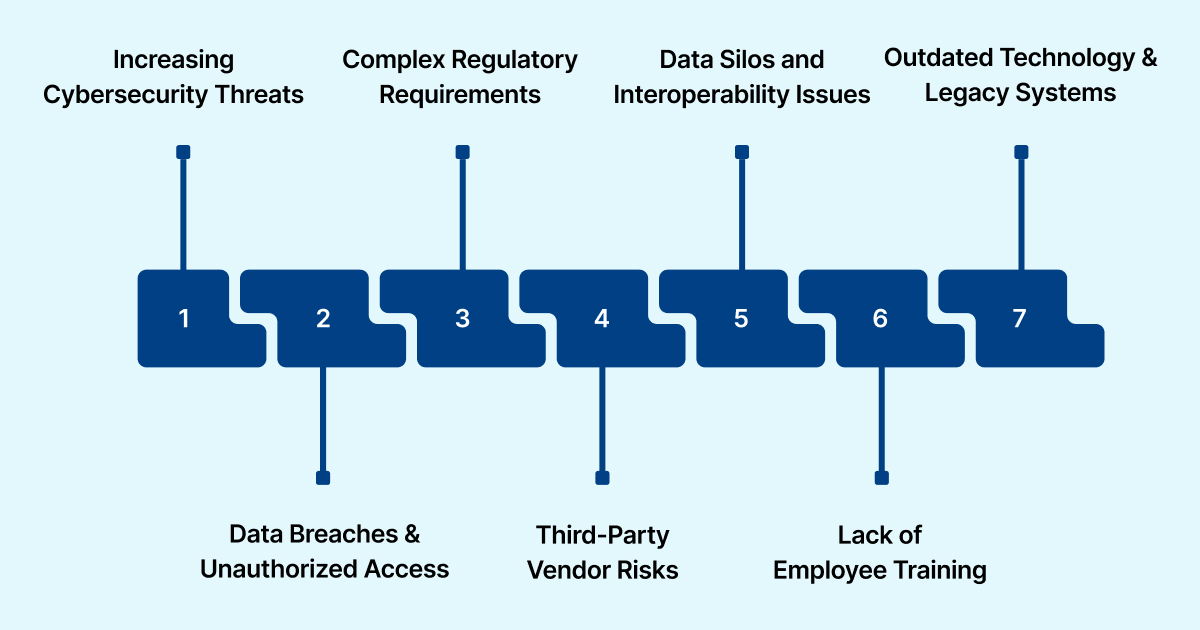
Healthcare organizations face growing challenges in protecting patient data, staying compliant, and addressing rising cyber threats. As digital health systems expand, managing and securing data becomes more complex. The need for strong security measures has never been more urgent with the increasing risk of cyberattacks.
Below are the key challenges healthcare organizations encounter in maintaining data security:
- Increasing Cybersecurity Threats: Healthcare is a frequent target for cybercriminals due to the high value of health data on the black market.
- Data Breaches and Unauthorized Access: Many healthcare providers struggle with unauthorized access to patient data, leading to breaches and non-compliance with regulatory standards.
- Complex Regulatory Requirements: Compliance with multiple regulations, such as HIPAA, HITECH, and the 21st Century Cures Act, creates significant administrative burdens.
- Third-Party Vendor Risks: Healthcare organizations often rely on third-party vendors for software and services, which can expose them to additional vulnerabilities.
- Data Silos and Interoperability Issues: Disconnected systems across departments or providers hinder the efficient sharing and protection of data, increasing security risks.
- Lack of Employee Training: Lack of proper training in security practices can lead to mistakes that result in data breaches or mishandling of sensitive information.
- Outdated Technology and Legacy Systems: Many healthcare organizations continue to rely on obsolete technology that lacks the necessary security measures to protect modern data.
As you evaluate the challenges, knowing the best practices to address these risks will be essential to your compliance strategy.
Best Practices for Healthcare Data Compliance And Security
To ensure data security and compliance in healthcare, organizations must implement a combination of proactive measures. These practices reduce risks, enhance protection, and maintain adherence to regulatory requirements. Following these best practices ensures the safety of patient data and helps organizations meet the demands of evolving regulations.
Below are essential best practices for securing healthcare data:
- Data Encryption: Encrypt data both when it's stored and when it's transmitted to protect against unauthorized access, maintaining the privacy and accuracy of sensitive information.
- Access Control and Authentication: Implement role-based access control (RBAC) and multi-factor authentication (MFA) to limit access to authorized personnel only.
- Regular Security Audits and Monitoring: Conduct regular audits and continuous monitoring to identify vulnerabilities and detect any potential security breaches early.
- Employee Training and Awareness: Train staff regularly on data security protocols, privacy laws, and best practices to minimize human error and reduce security risks.
- Strong Data Backup Practices: Set up automated data backups and ensure regular updates to minimize the risk of losing data during a breach.
- Third-Party Vendor Management: Assess the security measures of third-party vendors to ensure they align with industry standards and effectively protect sensitive health data.
- Incident Response Planning: Develop and regularly update an incident response plan to quickly address potential data breaches and reduce their impact on the organisation.
- Update Legacy Systems: Replace or upgrade outdated systems that lack proper security measures to safeguard against modern threats and vulnerabilities.
Now that we’ve covered the best practices, it’s essential to focus on how to handle data breaches and mitigate their impact.
Steps to Manage Healthcare Data Breaches Effectively
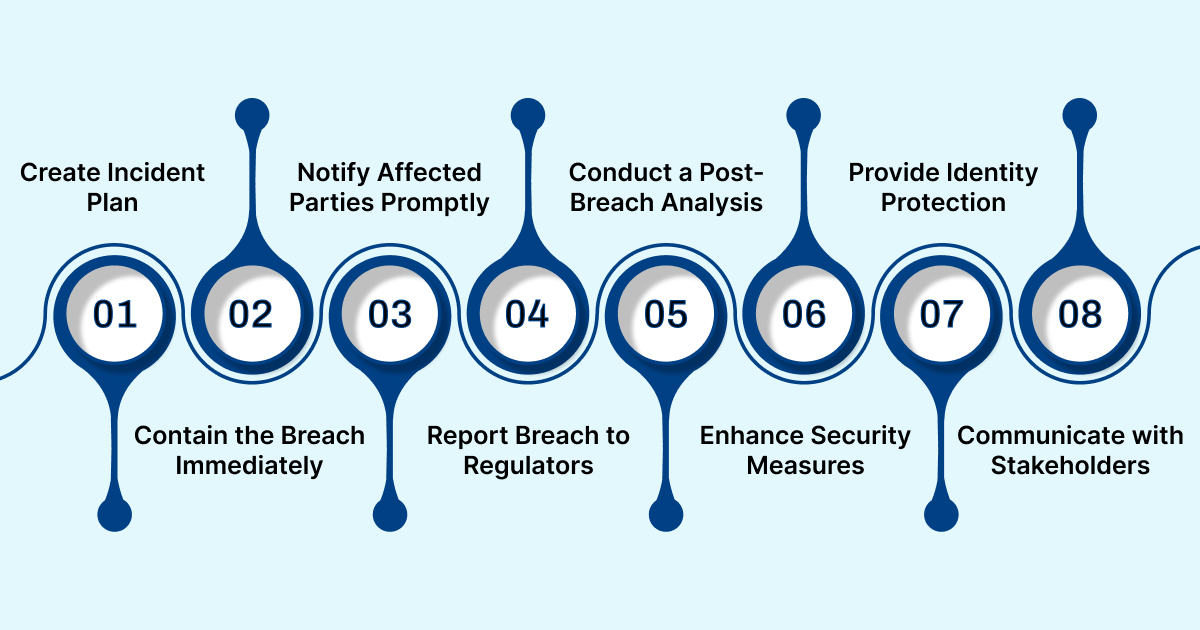
Managing data breaches in healthcare requires a swift, well-coordinated response to minimize harm and comply with legal requirements. Effective breach management reduces the impact on both patients and the organization.
The following best practices can help healthcare organizations effectively manage data breaches and mitigate their consequences:
- Develop an Incident Response Plan: Make sure your organization has a clear and detailed plan for responding to data breaches, including the necessary steps to take when an incident occurs.
- Contain the Breach Immediately: Once a breach is detected, take immediate action to limit its scope and prevent further exposure of sensitive information.
- Notify Affected Parties Promptly: Inform affected patients and stakeholders about the breach, as required by HIPAA, and guide the next steps.
- Report the Breach to Regulatory Bodies: Notify the relevant regulatory bodies, such as the Office for Civil Rights (OCR), within the required time frame to maintain compliance.
- Conduct a Post-Breach Analysis: After handling the breach, review how it happened and pinpoint areas that can be enhanced to avoid similar issues in the future.
- Enhance Security Measures: Following a breach, strengthen security measures to address identified vulnerabilities and implement more effective controls to protect against future breaches.
- Provide Identity Protection for Affected Individuals: Offer affected individuals identity protection services, such as credit monitoring, to mitigate potential harm from the breach.
- Maintain Communication with Stakeholders: Keep open communication with patients, regulatory authorities, and third-party vendors throughout the breach resolution process.
Given the complexities of managing data security and compliance, adopting automation solutions like RapidClaims can help you address these challenges more effectively.
How RapidClaims Supports Healthcare Data Compliance
RapidClaims is a B2B enterprise-grade SaaS platform designed to help healthcare organizations improve compliance, reduce coding errors, and enhance revenue cycle management. By automating the medical coding process, RapidClaims ensures accuracy while significantly reducing human errors and claim denials.
Below are the key features and benefits of using RapidClaims for healthcare compliance:
- Automated Medical Coding: RapidClaims automates the generation of accurate medical codes, reducing manual coding efforts and increasing operational efficiency.
- EHR Integration: It integrates directly with Electronic Health Records (EHR) systems, ensuring seamless data flow and eliminating errors during coding and claims submission.
- HCC Risk Adjustment: The platform enhances Hierarchical Condition Category (HCC) coding, improving risk adjustment factor (RAF) scores and ensuring accurate reimbursement.
- Claims Denial Reduction: Automating the coding process helps minimize claim denials caused by incorrect or incomplete codes.
- Real-time Compliance Checks: Provides real-time compliance verification, helping organizations stay updated with changing guidelines and reducing the risk of violations.
- NLP in Medical Billing: By using Natural Language Processing (NLP), RapidClaims enhances the ability to detect coding errors, improving accuracy and reducing denials.
- Scalable Solutions: Whether for small practices or large healthcare networks, you get flexible solutions that can be tailored to fit various organizational sizes.
- Cost Savings: By reducing manual efforts, it helps lower operational costs while improving the accuracy of claims submissions.
- Audit-readiness: The system ensures accurate coding and compliance, making it easier for healthcare organizations to remain ready for audits at all times.
By adopting RapidClaims, you can tackle compliance challenges head-on while improving your organization’s overall efficiency and accuracy.
Conclusion
Ensuring data security and compliance in healthcare requires a comprehensive approach that addresses operational challenges while adhering to regulatory standards. Accurate coding, error-free claims, and actionable data insights are essential not only for compliance but also for maximizing revenue and improving patient care.
RapidClaims helps organizations achieve this by offering solutions tailored to these needs. RapidCode enhances coding accuracy, reducing the risk of compliance issues. RapidScrub identifies and corrects errors, helping recover lost revenue efficiently. Meanwhile, RapidCDI transforms healthcare data into actionable insights, supporting informed decisions while maintaining regulatory compliance.
If you’re ready to improve your medical coding process and ensure compliance across your organization, contact us today.
FAQs
1. What are the key areas of focus in healthcare compliance?
Healthcare compliance primarily focuses on three key areas: privacy, security, and the proper management of healthcare data. These areas ensure patient confidentiality, safeguard against data breaches, and regulate how healthcare organizations handle sensitive information.
2. What are the three key parts of HIPAA compliance?
HIPAA compliance is centered on three major components: the Privacy Rule, which protects patient information; the Security Rule, which sets standards for data security; and the Breach Notification Rule, which mandates timely reporting of data breaches.
3. What is CMS compliance in healthcare?
CMS compliance in healthcare refers to adherence to the regulations set by the Centers for Medicare & Medicaid Services. It ensures that billing, reporting, and quality standards are met for services provided to Medicare and Medicaid recipients.
4. What is the US equivalent of the GDPR?
The U.S. does not have a single federal law equivalent to the GDPR. However, HIPAA, which governs healthcare data privacy and security, serves as a primary regulation for health data, while various state laws, like the CCPA in California, address broader data privacy concerns.
5. Is GDPR compliance mandatory?
Yes, GDPR compliance is required for any organization that processes the personal data of EU residents, regardless of the organization's location. Failure to follow compliance regulations can result in hefty fines and serious legal consequences.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
Related Post
Top Products

%201.png)








