.webp)
How Medical Billing and Coding Help Boosts Revenue


Medical billing and coding help is more than back-office support; it’s a strategic advantage.
Whether you're running a small private practice or managing a multi-location healthcare facility, getting expert help with billing and coding ensures your claims are submitted correctly, denials are minimized, and payments come in faster. It’s how you maintain a healthy revenue cycle while staying compliant with ever-evolving payer rules and regulations.
In a time where errors, rework, and compliance audits can put your finances and reputation at risk, professional billing and coding support is essential.
In this blog, we explore what medical billing and coding help really means, why it’s vital for your revenue cycle, and how platforms like RapidClaims can simplify compliance, reduce denials, and boost reimbursements.
TL;DR (Key Takeaways)
- Medical billing and coding help support practices in submitting accurate claims, reducing denials, and increasing reimbursements.
- Expert support or automation tools can eliminate manual errors, boost efficiency, and improve compliance with CMS and private payers.
- Services typically include CPT/ICD-10 coding, claim scrubbing, denial management, and compliance auditing.
- Common pain points solved: coding complexity, payer-specific rules, time-consuming claim resubmissions, and underpayments.
- Platforms like RapidClaims use AI and CMS-based logic to automate code validation, ensure clean submissions, and accelerate revenue cycles, without adding overhead.
What Is Medical Billing and Coding Help?
Medical billing and coding are closely linked processes that work together to convert healthcare services into reimbursable claims:
- Medical coding involves translating clinical procedures, diagnoses, and treatments into standardized codes (like CPT, ICD-10, and HCPCS).
- Medical billing takes those codes and generates insurance claims, then follows up to ensure payments are processed.
When we talk about “help” in this context, we’re referring to a range of solutions, from outsourced billing services to coding audits, claim scrubbing software, and staff training. The right help provides:
- Claims accuracy to prevent denials
- Faster reimbursements
- Compliance with payers and government regulations
- Reduced admin workload for in-house teams
Without this support, practices often face delayed payments, billing errors, and missed revenue, all of which can impact patient care in the long run.
Explore more on how to protect your practice from common billing and coding errors.
Why Practices Struggle Without Medical Billing and Coding Help
Even the most experienced practices face challenges when trying to manage billing and coding in-house. Here’s why:
1. Constantly Changing Code Sets & Payer Rules
CPT, ICD-10, and HCPCS codes are regularly updated. Add to that the specific billing guidelines from each insurance provider, and it's a lot to keep up with, especially for small teams. Without dedicated help, it’s easy to fall behind, leading to coding errors and denied claims.
2. High Staff Turnover & Limited Training
Medical billing and coding require specialized knowledge, and turnover in these roles can slow your revenue cycle to a crawl. In-house staff may also lack access to ongoing training, resulting in outdated practices or compliance gaps.
3. Lack of Automation or Technology
Many practices still rely on manual processes for claim creation, submission, and follow-up. This increases the risk of errors, slows down reimbursement, and consumes valuable staff time that could be spent on patient care or operations.
4. Mounting Claim Denials
Denied or rejected claims can cost your practice thousands every month, not just in lost revenue, but in time spent on appeals and rework. Without expert help, patterns go unnoticed, and denials keep piling up.
Curious how to overcome claim processing issues? Read our blog on claims processing challenges and strategies.
5. Compliance and Audit Risk
Incorrect coding or billing isn’t just a financial issue; it can trigger audits, fines, or even fraud investigations. Help from certified coding professionals or compliance-focused services significantly lowers your risk exposure.
What Types of Help Are Available for Medical Billing and Coding?

Depending on your practice size, specialty, and internal resources, there are different forms of medical billing and coding help available. Here’s a breakdown of the most common:
1. Outsourced Billing Services
Third-party billing companies handle everything from claim creation to follow-up. These partners often provide:
- Certified coders trained in CPT/ICD-10 guidelines
- Denial management and appeals
- Claim scrubbing before submission
- Payer follow-ups and revenue cycle reporting
Ideal for practices that lack in-house expertise or want to reduce admin burden.
2. Medical Coding Audits
Audits help ensure that your coding practices align with CMS guidelines and payer requirements. They typically review:
- Coding accuracy
- Modifier usage
- Documentation sufficiency
- Risk of overcoding/undercoding
Great for compliance checks, preparing for audits, or fixing recurring denial issues.
Want to understand the nuances of medical coding modifiers and how they affect billing? Check out this comprehensive guide.
3. Claims Scrubbing & Pre-Submission Tools
Software platforms that automatically check claims for errors before submission. They catch:
- Missing codes
- Invalid combinations
- Modifier errors
- Payer-specific rejections
A good option if you prefer to keep billing in-house but want to increase claim accuracy.
4. Training & Support for In-House Staff
Some vendors offer coding workshops, webinars, or ongoing education to keep your team updated on:
- ICD-10 updates
- New payer rules
- Specialty-specific billing practices
Essential for keeping in-house teams sharp and confident.
5. End-to-End RCM Platforms
These solutions combine billing, coding, patient payments, and analytics into one interface, often using AI to speed up processes and reduce human error. Some platforms even integrate with your EHR/PM system.
Key Benefits of Getting Medical Billing and Coding Help
Investing in medical billing and coding support can bring measurable improvements across your practice’s financial health, workflow efficiency, and compliance. Here’s what you can expect:
1. Faster Reimbursements
Clean, accurately coded claims get paid faster. Whether you're billing Medicare, Medicaid, or private payers, expert coding and scrubbing reduce back-and-forth delays and speed up the revenue cycle.
2. Fewer Denials and Rejections
Help from trained billing professionals or smart claim scrubbing tools can significantly reduce errors that trigger denials, like missing modifiers, mismatched codes, or invalid procedures.
3. Improved Cash Flow
More timely payments and fewer rejected claims mean predictable revenue and better financial control. Practices that get billing help often see a substantial reduction in accounts receivable (A/R) days.
4. Reduced Administrative Burden
By outsourcing or automating repetitive billing and coding tasks, your team has more time to focus on patients and operational improvements, without getting bogged down in paperwork or manual follow-ups.
Learn how AI is transforming medical coding accuracy and speeding up reimbursements.
5. Better Compliance and Audit Readiness
Certified coders and audit-focused tools help ensure your documentation aligns with CMS and payer guidelines. This reduces the risk of fines, audits, and reputational damage.
6. Scalability as You Grow
As your practice expands or adds services, professional billing support can scale with you. You don’t have to hire and train new staff just to keep up with claim volume.
How to Choose the Right Medical Billing and Coding Support

Not all solutions are created equal. Whether you're considering a billing service, software platform, or training program, it's important to assess your practice's needs and choose help that fits. Here are key factors to evaluate:
1. Experience in Your Specialty
Billing for cardiology, dermatology, orthopedics, or mental health all requires specialty-specific coding expertise. Look for partners or tools that understand the unique rules, modifiers, and payer nuances relevant to your field.
2. Certifications and Compliance Knowledge
Verify that billing professionals are certified (e.g., CPC, CCS, or CPB) and trained in HIPAA compliance. For software, ensure it aligns with CMS guidelines and undergoes regular updates to coding libraries and payer rules.
3. Technology Integration
Does the billing support integrate with your EHR, PM, or claims clearinghouse? Seamless integration helps avoid double entry, improves visibility, and accelerates workflows.
4. Track Record with Denials and Reimbursements
Ask for data or case studies. A reputable service should be able to show how they’ve reduced denial rates, improved clean claim rates, or shortened A/R days for similar practices.
5. Flexibility and Scalability
Whether you're a solo provider or multi-site practice, your needs may evolve. Choose a solution that can grow with you, offering add-on services, analytics, or automation as your volumes increase.
6. Transparent Pricing and SLAs
Make sure the cost structure (percentage-based, flat fee, etc.) aligns with your financial model, and clarify what’s included. Look for clear service-level agreements (SLAs) on turnaround times, response windows, and performance benchmarks.
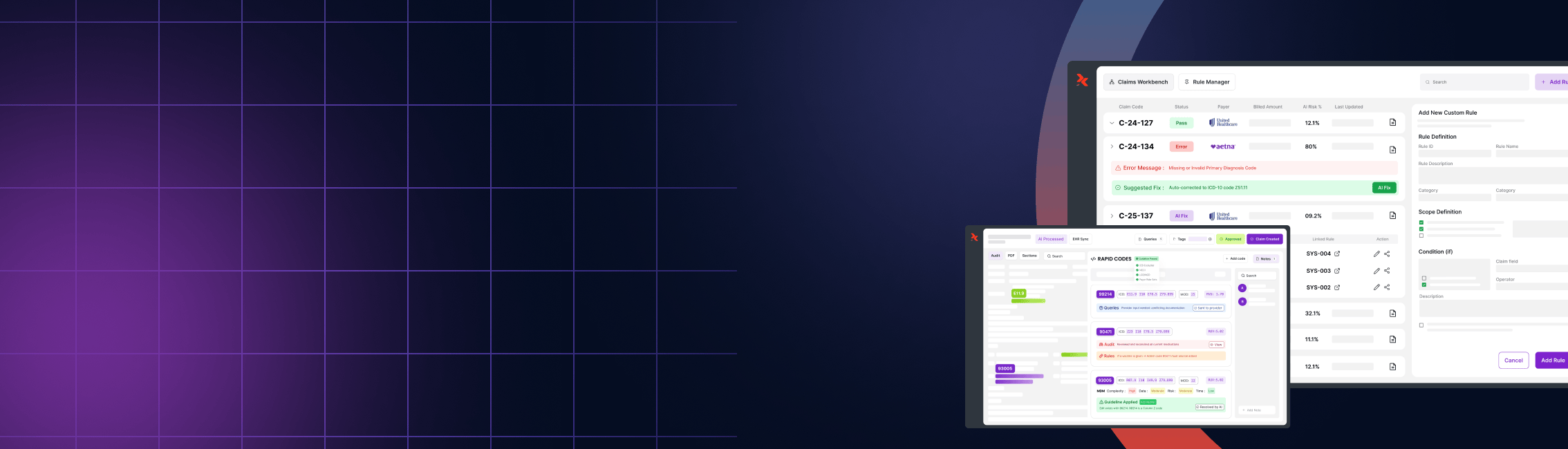
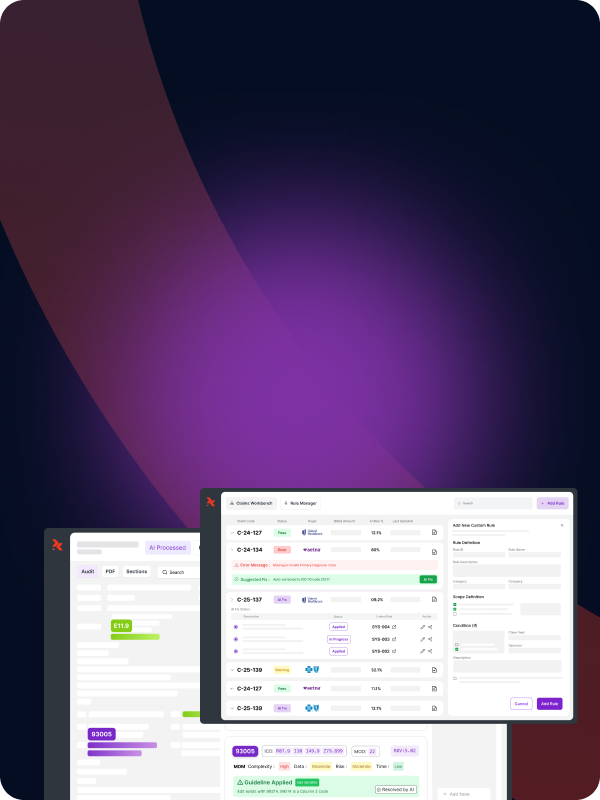
How RapidClaims Simplifies Medical Billing and Coding Help
If you're looking for a streamlined, AI-powered solution to simplify your billing and coding process, RapidClaims delivers end-to-end support built for modern healthcare practices.
What RapidClaims Offers
- NCCI-Driven Validation: Automatically applies CMS rules, including PTP and MUE edits, to ensure clean claims and reduce denials.
- AI-Powered Claim Scrubbing: Identifies coding errors, modifier misuse, and payer-specific issues before submission.
- Audit-Ready Documentation: Built-in rationale and audit trails for every compliance decision, keeping your practice protected.
- Seamless Integration: Works with leading EHR and PM systems using HL7 and FHIR standards.
Why It Matters
By reducing denials, improving coding accuracy, and automating repetitive tasks, RapidClaims helps providers:
- Increase reimbursements
- Speed up A/R cycles
- Maintain compliance without added manual work
- Get measurable results in as little as 30 days
Whether you're a small clinic or a multi-specialty group, RapidClaims offers scalable, results-backed billing and coding help that fits your workflow.
Schedule a demo to see how RapidClaims can improve your revenue cycle.
Conclusion
Medical billing and coding are the financial backbone of your healthcare practice, but they don’t need to be a burden. Whether you're overwhelmed with denied claims, struggling to keep up with coding updates, or simply looking to scale efficiently, getting expert help is the smartest step forward.
With the right support, like that offered by RapidClaims, you can ensure your claims are accurate, compliant, and submitted on time. That means fewer headaches, faster payments, and more time to focus on what matters most: patient care.
Looking for reliable medical billing and coding help?
Explore how RapidClaims can improve accuracy, reduce denials, and make your revenue cycle more efficient - starting day one.
Frequently Asked Questions (FAQs)
Q1: Why is medical billing and coding help important for providers?
A: It ensures accurate claims, reduces denials, speeds up payments, and keeps your practice compliant with CMS and private payer rules.
Q2: What types of practices benefit from billing and coding support?
A: All types, from solo physicians and group practices to urgent care centers and specialty clinics.
Q3: Can software like RapidClaims replace human coders?
A: Not replace, but augment. AI tools like RapidClaims reduce manual effort, catch coding errors early, and provide audit-ready validation to support in-house or outsourced coders.
Q4: How do I know if I need outside billing help?
A: If you’re seeing frequent claim rejections, delays in payment, high A/R, or compliance risks, professional help can offer a measurable improvement.
Q5: How quickly can RapidClaims show results?
A: Many providers report seeing improvements in claim accuracy and reduced denials within the first 30 days of implementation.
%201.png)