Ambulatory Services in Medical Billing: 2026 Guide
Ambulatory care continues to expand as more services shift from inpatient facilities to outpatient settings. Providers across the United States are seeing higher volumes of same day procedures, diagnostic visits, minor surgeries, and routine care delivered outside the hospital environment.
According to a 2025 national forecast, outpatient visit volume in the United States is expected to grow by 10.6 percent over the next five years.
This growth places greater pressure on ambulatory billing teams to maintain accuracy, strengthen documentation, prevent denials, and keep pace with evolving payer rules. As volumes rise, even small inefficiencies in coding, charge capture, or claim submission can disrupt cash flow and affect overall revenue cycle performance.
This guide explains how ambulatory services fit into medical billing, the steps involved in the billing workflow, common challenges, and the best practices and technologies that help outpatient organizations maintain compliance and financial stability in 2026 and beyond.
Key Takeaways
- Ambulatory care growth is accelerating, and the organizations that modernize billing workflows now will be better positioned to handle rising volume without increasing administrative cost.
- High-accuracy coding and clean documentation are becoming competitive advantages, not routine tasks, as payer scrutiny and packaged-service rules continue to tighten.
- Revenue cycle performance in outpatient settings improves most when teams proactively manage eligibility, prior authorization, and documentation quality—not just coding after the fact.
- Data visibility and real time analytics are essential; organizations that track the right metrics (clean claim rate, denial drivers, coder productivity, HCC relevance) can prevent revenue loss before it occurs.
- AI driven platforms like RapidClaims offer meaningful operational lift by improving coding consistency, strengthening documentation, and reducing denials, helping ambulatory centers sustain financial stability as encounter volumes grow.
Table of Contents:
- What Are Ambulatory Services in Medical Billing
- How Ambulatory Billing Works
- Ambulatory Coding Guidelines You Must Know
- Key Payment Models in Ambulatory Services
- Common Challenges in Ambulatory Medical Billing
- Best Practices for Accurate Ambulatory Billing
- Technology’s Role in Ambulatory Billing
- Key Revenue Cycle Metrics for Ambulatory Settings
- Trends Shaping Ambulatory Billing in 2026 and Beyond
- Conclusion
- FAQs
What Are Ambulatory Services in Medical Billing
Ambulatory services refer to medical care delivered without an overnight hospital stay. These services cover a wide range of clinical encounters that take place in outpatient settings where patients receive evaluation, treatment, or minor procedures and return home the same day.
Ambulatory care can include:
- Primary and specialty visits
- Same day surgeries
- Diagnostic imaging
- Laboratory testing
- Urgent care visits
- Physical therapy and rehabilitation
- Preventive screenings and routine care
In medical billing, ambulatory services require accurate documentation, correct procedure and diagnosis codes, and clear alignment with payer guidelines. Billing teams must confirm the services performed, capture the correct codes, and apply payer rules for outpatient settings. This includes using CPT and HCPCS codes for procedures and supplies, as well as ICD codes for diagnoses.
Ambulatory billing differs from inpatient billing because it focuses on single encounters, shorter visits, and specific procedure codes rather than complex inpatient stays. Each visit must be documented clearly to support the billed services and ensure compliance with payer requirements.
The next section explains how ambulatory billing actually works within the revenue cycle.
How Ambulatory Billing Works
Ambulatory billing follows a structured sequence that ensures every service is documented correctly and reimbursed according to payer requirements. The process includes multiple checkpoints that help reduce errors and support accurate claim submission.
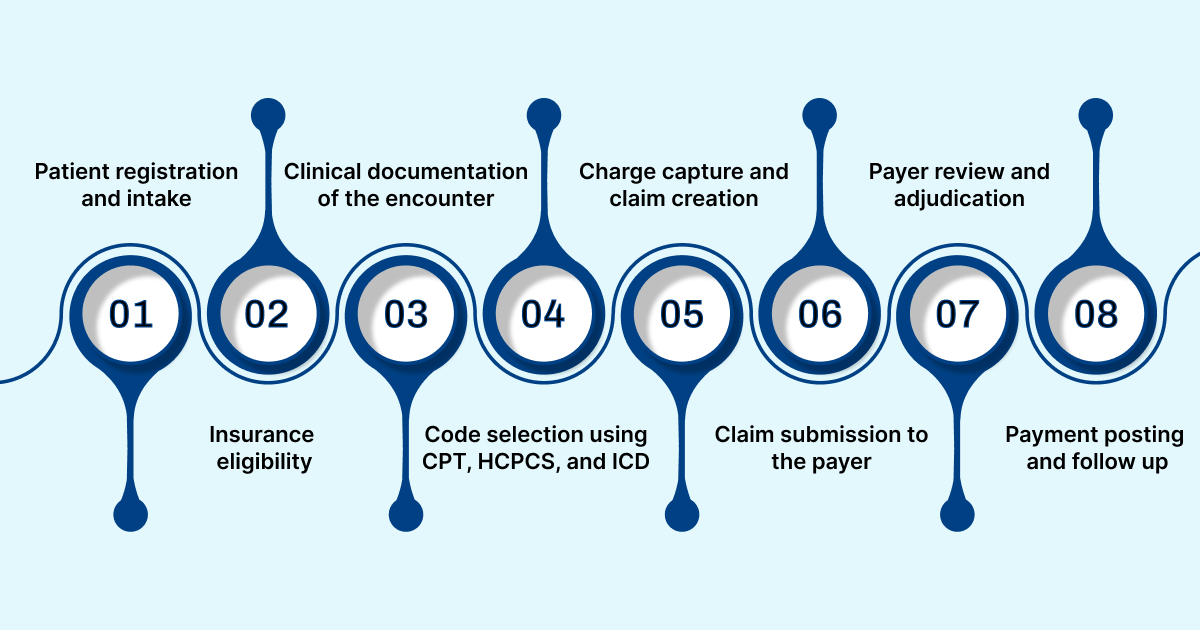
Key steps in the ambulatory billing workflow
- Patient registration and intake: Staff collect demographic details, insurance information, and visit purpose. Accurate intake prevents downstream billing issues.
- Insurance eligibility and benefit verification: Coverage, copays, prior authorization needs, and service limits are confirmed before the visit to avoid claim denials.
- Clinical documentation of the encounter: Providers record the reason for the visit, exam findings, procedures, treatments, and any supplies used. Clear documentation supports correct coding.
- Code selection using CPT, HCPCS, and ICD: Coding teams assign the appropriate procedure and diagnosis codes based on documented services. Many ambulatory encounters involve high volume, procedure driven coding.
- Charge capture and claim creation: All billable services and supplies are captured from the encounter. These details are assembled into a claim that reflects payer specific billing rules.
- Claim submission to the payer: Claims are submitted electronically through the practice management or billing system. Clean submission helps reduce delays.
- Payer review and adjudication: The payer evaluates the claim for accuracy, coverage, and medical necessity. Some claims may require additional documentation.
- Payment posting and follow up: Payments are recorded, variances are reviewed, and unpaid claims are followed up to resolve delays or discrepancies.
Many teams want to make these workflow steps more reliable without adding more manual review. RapidClaims uses an AI driven revenue cycle engine that has enabled clients to reach a reported 98 percent clean claim rate within the first month of use. Request a demo to see how similar automation can support each stage of your ambulatory billing process.
Ambulatory Coding Guidelines You Must Know
Coding in ambulatory settings requires attention to detail because most services are billed as individual procedures rather than bundled hospital stays. Accurate coding ensures proper reimbursement and supports compliance with payer expectations.
Key coding elements for ambulatory services
- CPT procedure codes: Ambulatory encounters rely heavily on CPT codes to represent surgeries, diagnostic tests, evaluations, minor procedures, and therapeutic services. Many ambulatory procedures fall under high volume surgical and diagnostic code groups.
- HCPCS Level II codes: Supplies, implants, injectables, durable medical equipment, and certain drugs used during ambulatory visits require HCPCS codes. Billing teams must document these items clearly to avoid payer edits.
- ICD diagnosis codes: Diagnoses must reflect the reason for the visit, findings, or conditions treated. ICD codes support medical necessity and must match what is documented in the clinical note.
- Modifiers for ambulatory billing: Modifiers clarify procedure circumstances such as bilateral services, repeat procedures, or the use of assistant surgeons. Correct modifier use helps prevent denials.
- ASC specific rules: When services are performed in an ambulatory surgery center, payers may require ASC approved procedure lists, device reporting, and drug administration details. These rules influence how services are coded and paid.
- Medical necessity documentation: Payers expect documentation to support why a service was required. Coders must ensure clinical notes align with codes submitted on the claim.
For ambulatory organizations with high coding volume, small accuracy gains can have a large financial impact. RapidCode has been audited at 96 percent coding accuracy and has delivered up to a 170 percent lift in coder productivity in some programs. Request a demo to review how AI assisted coding and documentation integrity can be applied to your current caseload.
Key Payment Models in Ambulatory Services
Ambulatory reimbursement is shaped by specific payment systems that determine how services are valued and paid. These models vary by setting and payer, and understanding them is essential for accurate billing.
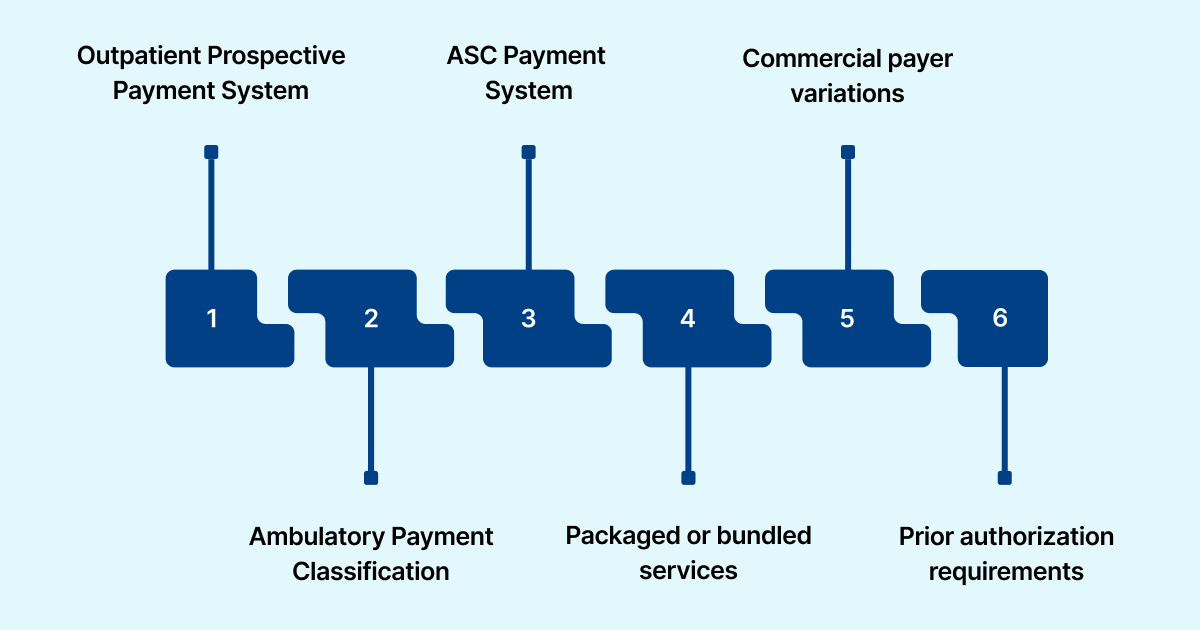
1. Outpatient Prospective Payment System: Under OPPS, Medicare assigns outpatient services to Ambulatory Payment Classifications. Each APC has a fixed payment rate that covers the procedure and related services. Hospitals use OPPS for most outpatient and ambulatory visits.
2. Ambulatory Payment Classification: APC groups are used to categorize services based on clinical similarity and cost. Correct APC placement depends on complete documentation and accurate coding.
3. ASC Payment System: Ambulatory surgery centers follow a separate Medicare payment schedule. Only procedures approved for ASC settings can be billed under this system. Payment includes facility services associated with the surgery, excluding certain drugs or implants.
4. Packaged or bundled services: Some services are packaged into a single APC or ASC payment. This means items such as supplies, anesthesia, or minor ancillary services may not be billed separately. Billing teams must know which items are packaged to avoid claim errors.
5. Commercial payer variations: Commercial insurers often use modified versions of OPPS or ASC fee schedules. Policies differ across plans, so billing teams must review contract specific rules for payment rates, authorization requirements, and coverage limits.
6. Prior authorization requirements: Many ambulatory procedures require authorization before the service is performed. Missing authorization can lead to full claim denial, even when clinical documentation is complete.
RapidClaims helps ensure correct grouping, packaged service identification, and authorization checks through tools such as RapidScrub and RapidRecovery. These capabilities reduce avoidable payment issues and support clean claim submission.
Common Challenges in Ambulatory Medical Billing
Ambulatory billing teams manage high visit volumes, complex payer rules, and tight turnaround times. These conditions create several recurring challenges that can slow reimbursement and reduce accuracy.
1. High procedure volume with limited review time: Ambulatory settings complete many short encounters or same day procedures. Billing teams often have limited time to validate documentation and coding before claims need to be submitted.
2. Frequent payer policy changes: Ambulatory services are subject to evolving payer rules, especially for procedures, implants, drugs, and diagnostic tests. Keeping up with these changes requires continual monitoring.
3. Prior authorization delays: Many ambulatory procedures require authorization. Incomplete or delayed submissions can cause missed appointments or full claim denials.
4. Errors in packaged or bundled services: Some services are included in a single payment group. When teams attempt to bill items that should be packaged, payers often reject the claim.
5. Documentation variability: Provider notes may vary in detail, which makes it hard for coders to select accurate codes or support medical necessity.
6. Limited integration between EHR and billing systems: Ambulatory centers may use separate platforms for scheduling, documentation, and billing. Manual handoffs increase the risk of missed charges.
7. Denial patterns that are hard to track: Ambulatory billing teams often face unpredictable denials tied to coding, authorizations, or bundled service rules. Without analytics, these patterns remain hidden.
Tools such as RapidScrub, RapidCDI, and RapidCode help reduce the operational load on billing teams.
Best Practices for Accurate Ambulatory Billing
Ambulatory billing requires precise coordination across clinical and administrative teams. Adopting structured workflows and consistent review processes helps reduce errors and improves reimbursement outcomes.
1. Standardize documentation templates: Clear templates help providers capture all essential details that support coding, medical necessity, and payer requirements. Consistency across departments reduces ambiguity for coders.
2. Use real time eligibility and benefit checks: Confirming coverage, copays, authorization needs, and service limits before the visit prevents avoidable denials.
3. Strengthen charge capture workflows: Teams should review procedure notes, supply usage, and ancillary services to ensure all billable items are captured accurately.
4. Provide ongoing coder education: Regular training helps coding staff stay updated on CPT changes, HCPCS updates, and payer specific rules that affect ambulatory billing.
5. Conduct pre submission claim review: A structured review step helps identify missing documentation, incorrect modifiers, or coding inconsistencies before sending claims to payers.
6. Perform internal audits: Routine audits uncover trends in coding errors or documentation gaps and help organizations adjust workflows before issues escalate.
7. Use billing analytics dashboards: Metrics related to claim quality, denial causes, and turnaround times help leaders make informed decisions and strengthen financial performance.
Automation can increase coder productivity by up to 150 percent in ambulatory care. Explore how RapidClaims improves accuracy and reduces cycle time.
Technology’s Role in Ambulatory Billing
Technology plays a major role in supporting accuracy and efficiency within ambulatory billing. As visit volumes grow and payer rules evolve, digital tools help teams reduce manual work, streamline reviews, and improve claim quality.

1. Integrated EHR and billing systems: Connecting clinical documentation with billing systems reduces duplicate entry and prevents missed charges. Integration also improves the flow of information from intake to claim submission.
2. Automated eligibility verification: Real time checks help confirm coverage, benefits, and authorization requirements before services are delivered. This reduces delays and prevents denials tied to eligibility issues.
3. Electronic claim review and validation: Automation can identify coding inconsistencies, missing documentation, and incorrect modifiers before claims are submitted. This improves first pass accuracy and reduces rework.
4. AI supported coding and documentation: Machine learning tools assist coders by analyzing notes, suggesting codes, and highlighting potential errors. These tools help maintain coding accuracy and reduce the manual load on staff.
5. Predictive denial analysis: Analytics platforms can highlight patterns in denials and identify claims with higher risk for rejection. This allows billing teams to prioritize review and address issues early.
How RapidClaims enhances technology driven workflows
RapidClaims strengthens ambulatory billing workflows by combining AI-driven medical coding intelligence with automation that supports accuracy, speed, and compliance across outpatient revenue cycle operations.
- RapidCode: RapidCode delivers fully autonomous, AI-driven medical coding for high-volume ambulatory encounters. It analyzes clinical documentation using natural language processing to assign accurate CPT, HCPCS, ICD-10, and E&M codes while maintaining a complete audit trail for compliance and review.
- RapidAssist: RapidAssist supports coding teams with AI-generated code suggestions and real-time documentation gap analysis. This helps coders validate encounters faster, reduce manual review effort, and maintain consistency across outpatient visits.
- RapidRecovery: RapidRecovery focuses on downstream revenue protection by supporting denial recovery and follow-up workflows. It helps billing teams identify denied or underpaid ambulatory claims, prioritize recoverable accounts, and streamline follow-up actions so revenue is not lost due to avoidable administrative delays.
Together, these capabilities allow ambulatory organizations to automate repetitive tasks, improve coding and documentation accuracy, and reduce administrative burden across the billing lifecycle. By integrating seamlessly with EHRs, billing systems, and HL7 or FHIR-based workflows, RapidClaims helps outpatient teams manage growing encounter volumes while maintaining compliance with CMS, HIPAA, ICD-10, and CPT requirements.
Key Revenue Cycle Metrics for Ambulatory Settings
Measuring performance is essential for maintaining a healthy revenue cycle in ambulatory environments. These metrics help teams evaluate billing accuracy, identify weak points, and track improvement over time.
1. Clean claim rate: Shows the percentage of claims that pass through without edits. Higher values indicate strong documentation and coding quality.
2. First pass resolution rate: Reflects how many claims are paid on the first submission. This metric helps determine how effectively teams prevent common errors.
3. Days in A/R: Measures the time it takes to collect payments after claims are submitted. Lower values indicate faster reimbursement and stronger financial stability.
4. Denial rate: Tracks the percentage of claims rejected by payers. Monitoring denial categories helps teams focus on correction and prevention.
5. Productivity per coder: Shows how many charts or encounters a coder completes in a set period. This helps organizations evaluate staffing needs and workflow efficiency.
6. Case mix complexity: Indicates the clinical and coding complexity of the ambulatory population. Higher complexity requires stronger documentation and review processes.
7. HCC relevance in ambulatory visits: Many chronic conditions are identified during ambulatory encounters.
For teams that want to understand potential impact before committing to a large rollout, RapidClaims offers an ROI model using approximately 500 historical charts. This analysis estimates savings across coding, denials, and documentation improvements in just a few days. Request a demo and share a sample data set to receive a tailored performance and savings projection.
Trends Shaping Ambulatory Billing in 2026 and Beyond
Ambulatory billing continues to evolve as clinical practices, payer policies, and technology advance. Several trends are expected to influence how organizations manage billing and reimbursement in the coming years.
1. Rising demand for same day care: More clinical services are being delivered without hospital admission. This increases the volume of encounters that require accurate outpatient billing.
2. Continued growth in ASC procedures: Ambulatory surgery centers are handling more orthopedic, cardiovascular, and gastrointestinal procedures. This increases the need for precise procedure coding and ASC specific billing expertise.
3. Expansion of bundled payment models: Payers are shifting more procedures into bundled payment structures. Billing teams must understand which services are packaged to avoid incorrect charges.
4. Greater use of AI and predictive analytics: Automated coding, documentation prompts, and real time claim checks are becoming standard tools that help reduce errors and improve claim quality.
5. New CMS updates for outpatient reimbursement: Changes in CPT codes, ASC procedure lists, and quality reporting requirements are expected each year. Ambulatory teams must stay updated to maintain compliance.
6. Increasing importance of risk adjustment: Chronic conditions identified in ambulatory settings influence reimbursement for value based programs. Accurate diagnosis capture during these visits will have a growing impact on payment models.
RapidClaims supports these emerging trends with tools that adapt quickly to payer policy updates, strengthen risk adjusted documentation, and provide automated support across coding, claim scrubbing, and denial prevention.
Conclusion
Ambulatory billing plays a central role in maintaining financial stability as more services shift from inpatient to outpatient settings. With rising encounter volumes, evolving payer rules, and increasing documentation demands, organizations need reliable workflows that support accuracy, reduce denials, and keep claims moving through the revenue cycle without delays.
Improving performance requires a combination of structured processes, timely audits, strong documentation, and the right technology. Organizations that adopt automation and data driven tools are better positioned to handle complex billing requirements and maintain steady reimbursement.
RapidClaims provides automated support across coding, documentation review, claim validation, and denial prevention. These capabilities help ambulatory teams increase accuracy, reduce administrative work, and strengthen overall revenue cycle performance.
Request a demo to see how RapidClaims can support your ambulatory billing workflows and help your organization maintain financial stability as outpatient volumes continue to grow.
FAQs
Q: What is considered an ambulatory service for billing purposes?
A: Ambulatory services include any medical care delivered without an overnight stay; such as same-day surgeries, minor procedures, diagnostic imaging, lab tests, urgent care visits, and routine outpatient evaluations. These services must be documented, coded, and billed according to outpatient reimbursement rules.
Q: How is ambulatory billing different from inpatient billing?
A: Ambulatory billing focuses on single encounters and procedure-specific CPT/HCPCS codes, while inpatient billing uses DRGs, bundled stays, and more complex documentation. Outpatient claims require precise coding for each procedure performed on the same day.
Q: What are the biggest billing challenges in ambulatory care?
A: Common issues include prior authorization delays, packaged/bundled service confusion, inconsistent documentation, ASC-specific rules, payer policy changes, and high denial rates tied to coding and medical necessity.
Q: What is an APC in ambulatory billing?
A: An Ambulatory Payment Classification (APC) is a reimbursement grouping under Medicare’s Outpatient Prospective Payment System (OPPS). Each APC has a fixed payment rate based on similar clinical intensity and cost.
Q: What tools help automate ambulatory medical billing?
A: Organizations use solutions for coding assistance, documentation integrity, predictive denial prevention, authorization checks, and claim scrubbing. Platforms like RapidClaims automate key steps such as coding, documentation review, and error detection to reduce denials and improve first-pass accuracy.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








