Denial Prevention in Healthcare: A Comprehensive Guide for 2025

Did you know? In 2024, the initial claim denial rate for hospitals increased to 11.81%, resulting in millions of dollars in lost revenue and delayed cash flow.
With rising payer challenges, changing regulations, and increasing staff workload, effective denial prevention is now more critical than ever. Even a one‑percent reduction in denials can translate into significant recovered revenue, reduced administrative burden, and improved hospital performance.
In this blog, you'll explore a roadmap for preventive denial management, guiding your team to identify root causes, implement controls, and sustain measurable performance improvements.
TL;DR (Key Takeaway)
- Identify Issues Early: Detect coding, documentation, and eligibility errors before claims submission to reduce denials.
- Ensure Accurate Coding: Use the correct ICD, CPT, and HCPCS codes, aligned with the clinical documentation.
- Leverage Technology: AI, claim scrubbing, predictive analytics, and EHR integration prevent errors and speed reimbursements.
- Train Staff & Engage Patients: Educate teams on payer rules and inform patients of financial responsibilities to reduce preventable denials.
- Utilize Data for Improvement: Track denial trends and apply insights to enhance processes and revenue outcomes continually.
Table of Contents:
- Claim Denial Prevention: What it is and Why it Matters
- Common Causes of Claim Denials in Healthcare
- 10 Key Strategies for Effective Denial Prevention in Healthcare
- Role of Technology in Claim Denial Prevention
- How RapidClaims Enhances Denial Prevention in Healthcare?
- Conclusion
- Frequently Asked Questions (FAQs)
Claim Denial Prevention: What it is and Why it Matters
Denial Prevention is a proactive approach used by healthcare providers to minimize or eliminate claim denials from insurance payers. It involves identifying potential errors, documentation gaps, compliance issues, or eligibility problems before submitting claims to ensure accuracy and completeness of the claims.
The primary objective is to ensure that claims are accurate, complete, and aligned with payer requirements, thereby enhancing the efficiency of the RCM process.
Here’s why preventing denials matters:
- Reduces Revenue Loss: Prevents avoidable claim rejections that directly lower reimbursement and increase write-offs.
- Improves Cash Flow: Ensures cleaner claims on first submission, accelerating payment cycles and reducing A/R days.
- Lowers Administrative Burden: Cuts time spent on rework, appeals, and back-and-forth with payers, improving staff efficiency.
- Strengthens Compliance: Aligns claims with payer policies, coding rules, and regulatory requirements, reducing audit and compliance risks.
Now, let's examine the most common causes of claim denials in healthcare to understand where errors occur and their impact on revenue.
Common Causes of Claim Denials in Healthcare
Claim denials disrupt cash flow and increase administrative workload. Most denials stem from preventable issues related to eligibility, coding, documentation, or payer rules. Understanding these causes is critical for identifying operational gaps.
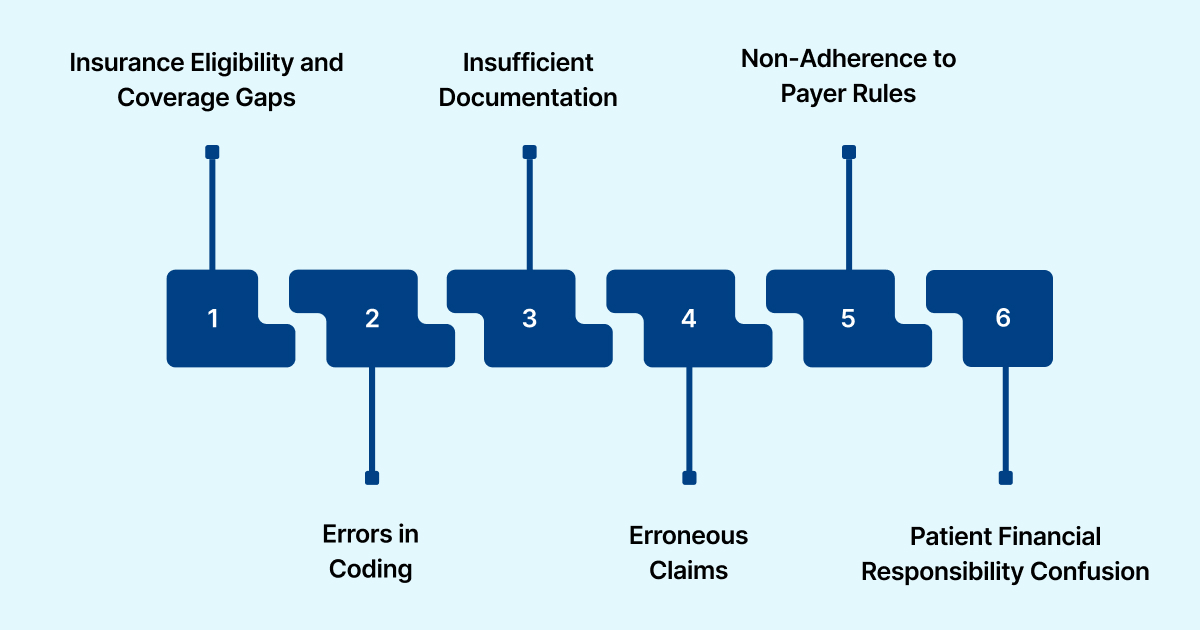
- Insurance Eligibility and Coverage Gaps
Denials often occur when patients lack coverage for specific services or their insurance information is not up-to-date. Coverage limitations or lapses trigger automatic rejections. Pre-authorization requirements that are unmet also contribute to denials.
- Errors in Coding
Incorrect ICD, CPT, or HCPCS codes are a leading reason for denials. Even minor mistakes, like missing modifiers or invalid combinations, can cause claim rejection. Inconsistent coding practices across departments amplify the risk.
- Incomplete or Insufficient Documentation
Claims are often denied when clinical records do not adequately support medical necessity. Missing signatures, unclear notes, or incomplete treatment details often result in payer rejections. These documentation gaps can also cause coding errors.
- Duplicate or Erroneous Claims
Submitting duplicate claims or using incorrect patient or provider details often triggers denials. These errors, whether human or system-related, increase administrative burden and slow revenue processing.
- Non-Adherence to Payer Rules
Each payer maintains specific submission, coding, and documentation requirements. Claims are often denied when these rules are not followed, and frequent regulatory updates increase the risk of non-compliance.
- Patient Financial Responsibility Confusion
Denials can occur when patient obligations, including co-pays, deductibles, or non-covered services, are unclear. Miscommunication can delay processing and may lead to adjustments or write-offs.
RapidClaims addresses these issues by detecting coding errors and missing documentation before claim submission, which helps ensure smoother operations and faster reimbursements. Additionally, its AI-driven real-time insights improve claim acceptance rates while seamlessly integrating with hospitals, physician groups, medical billing companies, and Accountable Care Organizations (ACOs) to enhance overall workflow efficiency.
Also Read: How to Effectively Appeal a Denied Insurance Claim: A Step-by-Step Guide
Now, let’s connect the dots between denial causes and solutions, reviewing ten strategies that healthcare teams can use to reduce rejections and improve financial performance.
10 Key Strategies for Effective Denial Prevention in Healthcare
Claim denials are more than administrative headaches; they can disrupt cash flow, delay reimbursements, and increase operational costs. While some denials are inevitable, most can be prevented with a proactive approach.
The following ten strategies provide practical, actionable steps to strengthen claim denial prevention efforts.
1. Eligibility & Benefits Verification
Ensuring patients have valid insurance coverage and understanding their benefits before or at the point of service is foundational to denial prevention. Proactively addressing coverage gaps reduces downstream issues and avoids unnecessary rework.
- Confirm active insurance status and coverage limits.
- Identify plan-specific exclusions or special requirements.
- Utilize real-time electronic or EHR-integrated verification tools.
- Verify co-payments, deductibles, and benefit limits with patients to ensure accurate information is provided.
- Communicate potential out-of-pocket responsibilities upfront.
2. Accurate Medical Coding
Accurate coding is crucial for accurately representing the services rendered. Misapplied or outdated codes are a leading contributor to claim denials and can trigger audits or compliance concerns.
- Assign HCPCS, ICD-10, and CPT codes based strictly on clinical documentation.
- Stay current with coding guideline updates and payer-specific requirements.
- Conduct routine internal audits to identify and correct discrepancies pre-submission.
3. Pre-Authorization & Prior Approvals
Certain procedures, diagnostics, and treatments require prior approval from the payer. Failure to secure pre-authorization can result in outright claim rejections and delayed patient care.
- Identify services requiring prior authorization.
- Submit requests promptly to allow sufficient processing time.
- Maintain comprehensive records of approvals to support claims and ensure accurate documentation.
4. Claim Scrubbing & Validation
Claim scrubbing serves as the final quality checkpoint before submission. Automated tools and validation protocols help detect errors, inconsistencies, or missing information that could trigger denials.
- Verify the completeness of patient and provider information.
- Validate diagnosis-to-procedure and code combinations.
- Detect duplicate or conflicting claims before submission.
5. Staff Training & Education
Even the most sophisticated systems rely on knowledgeable staff. Continuous training ensures teams are proficient in coding, documentation, and payer requirements, reducing error-prone claims.
- Educate staff on coding updates and payer-specific rules.
- Reinforce proper documentation standards and compliance protocols.
- Conduct periodic workshops on best practices for claim submission.
6. Timely & Accurate Documentation
Complete, accurate, and timely clinical documentation forms the backbone of successful claims. Delayed or incomplete records increase the likelihood of denials and create compliance risks.
- Document all services thoroughly at the point of care.
- Ensure records are structured, legible, and compliant.
- Integrate documentation seamlessly with coding and billing workflows.
7. Patient Financial Counseling
Informing patients about their financial responsibility mitigates denials resulting from non-covered services or uncollected balances. Transparent communication improves satisfaction and reduces disputes.
- Explain coverage, co-pays, and deductibles clearly and concisely.
- Offer structured payment plans for uncovered services.
- Confirm patient understanding before proceeding with care.
8. Integration of EHR and Billing Systems
Seamless integration between clinical and billing systems minimizes errors and improves first-pass claim acceptance. Automation ensures consistency and reliability across all claims.
- Automate the transfer of documentation to billing systems.
- Generate claims directly from EHR data to reduce manual errors.
- Maintain accurate audit trails for compliance and reporting purposes.
9. Prior Denial Analysis & Feedback Loops
Analyzing previous denials uncovers recurring patterns and operational gaps. Continuous feedback enables corrective actions, process improvement, and staff accountability.
- Track denials by payer, department, or service type.
- Implement corrective measures informed by data insights.
- Train staff on patterns identified to prevent repeated denials.
10. Payer-Specific Rules Awareness
Each payer has unique submission rules, coding requirements, and documentation standards. Staying informed ensures compliance and reduces preventable denials.
- Maintain a current database of payer-specific rules and guidelines.
- Adjust coding, documentation, and claim submission workflows accordingly.
- Monitor regulatory updates and implement changes promptly.
Also Read: Robotic Process Automation and AI in Healthcare Operations.
Denial prevention is not a single task but a coordinated effort across staff training, technology, patient engagement, and compliance monitoring. By systematically implementing these ten strategies, healthcare organizations can reduce claim denials, improve revenue cycle efficiency, and enhance both operational and patient satisfaction outcomes.
Role of Technology in Claim Denial Prevention
Technology helps reduce claim denials and improve revenue cycle efficiency. Automated checks, predictive analytics, and AI-driven tools enable healthcare organizations to quickly identify errors, coding issues, and compliance gaps before submission, improving claim accuracy, speeding reimbursements, and enhancing financial performance.

Below are the key technology solutions for claim denial prevention:
1. Automated Eligibility Verification
Verifying patient insurance coverage in real time prevents many denials related to ineligibility or missing pre-authorizations. Automation ensures that staff have accurate information at the point of care.
- Check patient coverage status and plan limits instantly.
- Identify plan-specific exclusions or pre-authorization requirements.
- Reduce claim rejections and patient surprise costs.
2. EHR and Billing System Integration
Integrating electronic health records (EHR) with billing systems ensures that claims accurately reflect clinical documentation. This reduces manual errors and supports faster, first-pass claim acceptance.
- Automate data transfer from clinical notes to billing systems.
- Eliminate inconsistencies between documentation and claims.
- Improve reimbursement speed and accuracy.
3. Claim Scrubbing Software
Claim scrubbing tools review submissions for errors before they reach payers, ensuring accuracy and preventing errors from reaching payers. By catching mistakes early, they prevent rework and reduce the likelihood of denials.
- Detect missing patient or provider information.
- Validate codes, diagnoses, and procedure combinations.
- Identify duplicates or inconsistencies before submission.
4. Analytics and Reporting Tools
Advanced analytics track denial trends, high-risk payers, and departmental patterns. Insights from these tools guide process improvements and proactive staff training.
- Highlight recurring denial patterns by payer or service.
- Provide actionable insights for revenue cycle optimization.
- Support data-driven decision-making for workflow efficiency.
5. Patient Financial Engagement Platforms
Digital patient engagement tools educate patients on their financial responsibilities and simplify payment processes. Clear communication reduces denials caused by misunderstandings or delayed payments.
- Inform patients about co-pays, deductibles, and non-covered services.
- Offer online payment plans or pre-service cost estimates.
- Improve patient satisfaction and reduce claim disputes.
By utilizing AI and automation, RapidClaims helps reduce claim denials through coding accuracy, accelerates the revenue cycle by processing over 100 charts per minute, and ensures compliance with regulatory requirements via built-in rule sets. Streamline your workflow and enhance your revenue cycle management with RapidClaims today!
How RapidClaims Enhances Denial Prevention in Healthcare?
RapidClaims is an advanced AI-powered platform that automates medical coding, streamlines operations, and cuts administrative costs. It optimizes reimbursement processes and ensures full compliance with ever-evolving healthcare standards. With a 70% reduction in preventable denials and a 5-day faster A/R recovery, RapidClaims improves financial performance.
- Explainable & Compliant AI: RapidClaims provides a full audit trail and transparent AI for all codes, achieving 96% coding accuracy and 99% compliance. This reduces errors that commonly trigger claim denials.
- Customized AI & Rule Sets: The platform continuously updates coding rules in accordance with payer policies and NCCI/LCD/NCD requirements, ensuring compliance across 36+ specialties. This prevents denials due to non-adherence or outdated rules.
- Real-Time Eligibility & Pre-Authorization Checks: RapidClaims checks patient coverage and pre-authorizations instantly through API integrations, minimizing denials from coverage gaps or unapproved services. It also reduces administrative burden on staff.
- Predictive Denial Scoring: AI assigns a denial probability score to prioritize high-risk claims for review and expedite the review process. This proactive approach prevents avoidable denials and optimizes collection efficiency.
- Closed-Loop Feedback and Analytics: Insights from RapidRecovery feed back into RapidScrub, continuously improving claim accuracy. Real-time analytics track denial trends and provide CFO-ready ROI, safeguarding future revenue.
With automated coding, AI-driven workflow optimization, and real-time insights, RapidClaims ensures accuracy and efficiency throughout the claims process.
Conclusion
Many claim denials could be avoided; yet, they continue to disrupt healthcare providers’ revenue cycles and increase administrative burdens. Errors in documentation, coding, or prior authorization often lead to delayed reimbursements and lost revenue.
An AI-powered platform like RapidClaims addresses these challenges by automating coding, streamlining workflows, and providing real-time insights. By proactively identifying and resolving potential issues before submission, RapidClaims reduces denials, enhances first-pass claim acceptance rates, and strengthens overall financial performance.
Take the next step in preventing claim denials and optimizing your revenue cycle. Schedule a Free Demo to see how RapidClaims ensures accurate, compliant claims and improves first-pass acceptance.
Frequently Asked Questions (FAQs)
1. How long do I have to appeal a denied claim?
A. Most payers allow 30–180 days to appeal a denied claim. Timely submission safeguards revenue and maintains smooth cash flow.
2. Can I file a claim denial appeal without a denial notice?
A. No. You need the official denial notice, which details the reason for denial and outlines the appeal process.
3. How can I handle a claim denial due to timely filing issues?
A. If a claim is denied for late submission, check for exceptions or extensions. Provide valid reasons to support your appeal and minimize revenue loss.
4. What should I do if my claim exceeds benefit limits?
A. Review the policy for annual or lifetime caps. Discuss with the insurer and consider secondary coverage or alternate funding options for medically necessary services.
5. How do I handle denials for out-of-pocket expense reimbursement?
A. Verify expenses against the policy and submit detailed receipts and medical documentation. This ensures proper consideration and improves the first-pass claim acceptance rate.
6. Can I file multiple appeals for a denied claim?
A. Yes. File multiple appeals if you have new or additional supporting evidence, and track all submissions and communications for compliance and audit readiness.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






