Medical Reimbursement and Coding: A Complete Guide for 2026

Are coding errors costing your healthcare organization millions? High claim denial rates and delayed reimbursements are common consequences of inaccurate coding. This challenge strains resources and slows reimbursement cycles.
A recent study found that 80% of U.S. medical bills contain errors, underscoring the widespread impact of inaccurate coding. Healthcare organizations must address this to avoid revenue loss.
Medical reimbursement and coding are vital for ensuring timely payments. This guide explores how improving these processes can reduce denials and optimize financial health for healthcare providers.
Overview
- Medical reimbursement and coding are vital for ensuring accurate payments and compliance in healthcare organizations.
- Errors in coding and documentation lead to claim denials, delayed reimbursements, and financial inefficiencies.
- Automation and AI-driven tools improve coding accuracy, reduce administrative costs, and speed up claim processing.
- Following best practices like real-time claim validation, standardized coding, and regular audits can streamline workflows.
- Implementing these practices ensures faster payments, minimizes denials, and improves cash flow for healthcare providers.
Table of Contents
- What is Medical Reimbursement and Coding?
- Key Components of Medical Reimbursement and Coding
- How Medical Reimbursement and Coding Impact Healthcare Organizations
- Challenges in Medical Reimbursement and Coding
- 6 Best Practices for Efficient Medical Reimbursement and Coding
- How Can RapidClaims Help Streamline Medical Coding and Reimbursement?
- Wrapping Up
- FAQS
What is Medical Reimbursement and Coding?
Medical reimbursement and coding are critical components of the revenue cycle management (RCM) process, directly impacting a healthcare provider's cash flow.
Coding involves assigning standardized codes (ICD-10, CPT, HCC) to diagnoses and procedures, while reimbursement refers to the payment healthcare providers receive from insurers or government programs for services rendered.
The accuracy of both processes determines the speed of payment and reduces the risk of denials or audits, ensuring that healthcare organizations maintain financial stability.
Understanding the key components of medical reimbursement and coding helps identify opportunities for improvement and automation in these areas.
Key Components of Medical Reimbursement and Coding
Medical reimbursement and coding rely on several components that ensure the accurate and timely processing of claims. Each element plays a pivotal role in minimizing denials and optimizing reimbursement for healthcare providers.
- ICD-10 Codes: These are used to identify diagnoses, symptoms, and diseases. Correct usage ensures accurate classification of patient conditions for proper reimbursement.
- CPT Codes: Standardized codes for medical, surgical, and diagnostic procedures. They are vital for ensuring that healthcare services are billed correctly and reimbursements are maximized.
- HCPCS Codes: Used for services not covered by CPT codes, such as durable medical equipment (DME) and ambulance services. These codes ensure that all healthcare services, including outpatient care, are properly reimbursed.
- E&M Codes: Evaluation and management codes determine reimbursement levels for patient visits based on the complexity of care provided. Accurate E&M coding is crucial for capturing appropriate payment for consultations and patient assessments.
- HCC Codes: Hierarchical Condition Categories are used in risk-adjustment models, particularly for Medicare Advantage. Correctly assigning HCC codes can significantly impact reimbursement accuracy, especially for chronic conditions and complex care needs.
These key components form the foundation of an effective reimbursement and coding system, directly influencing the financial health of healthcare organizations.
Understanding how these elements interact can reveal their profound impact on overall operations and revenue cycle management.
Also Read: How Healthcare Reimbursement Works: 3 Key Steps Explained
How Medical Reimbursement and Coding Impact Healthcare Organizations
Medical reimbursement and coding are at the heart of a healthcare organization's revenue cycle. Accurate coding and efficient reimbursement practices ensure timely payments, reduce operational costs, and minimize the risk of audits.

Here’s how medical reimbursement and coding directly impact healthcare organizations:
1. Revenue Cycle Optimization
Efficient revenue cycle optimization accelerates claim processing and ensures timely reimbursement.
Here's how revenue cycle optimization impacts the process:
- Accelerated Claims Processing: Automation reduces manual coding, speeds up claim submissions, and ensures quicker reimbursements.
- Improved Cash Flow: Accurate and timely coding leads to faster payment cycles, reducing delays in receiving funds.
- Reduced Administrative Burden: Streamlined processes free up resources, allowing staff to focus on more complex tasks while minimizing rework.
2. Cash Flow and Financial Health
Accurate medical reimbursement and coding are crucial for maintaining steady cash flow and financial health. Proper coding ensures that healthcare providers are reimbursed fully and promptly.
- Timely Reimbursements: Correct coding prevents payment delays and ensures accurate billing, leading to faster reimbursements.
- Minimized Revenue Loss: Accurate coding helps avoid underpayments or missed claims, ensuring full compensation for services rendered.
- Predictable Financial Flow: Streamlined coding and reimbursement processes result in more consistent and reliable cash flow.
3. Compliance and Regulatory Risk Management
Medical reimbursement and coding must align with regulatory standards to ensure compliance and avoid costly penalties. Proper coding practices mitigate the risk of audits and non-compliance.
- Adherence to Regulatory Standards: Accurate coding ensures compliance with ICD-10, CPT, HIPAA, and payer-specific rules, reducing regulatory risk.
- Audit Prevention: Correct coding practices help avoid errors that may trigger audits or fines, ensuring smooth operations.
- Real-Time Compliance Checks: Automated systems can ensure that all codes are compliant with the latest regulatory updates and payer requirements.
4. Operational Efficiency
Streamlining medical reimbursement and coding processes leads to higher productivity and fewer errors. It also reduces the time spent on administrative tasks, allowing staff to focus on patient care.
- Automation of Repetitive Tasks: Automated coding and billing processes free up time for more complex, value-added tasks.
- Error Reduction: Automation reduces the chance of human error, ensuring more accurate claims and fewer rework cycles.
- Faster Billing Cycle: Streamlined workflows accelerate the billing process, improving the overall speed of claim submissions and payment collection.
5. Reducing Claim Denials
Reducing claim denials is a major priority in the medical reimbursement process. By improving coding accuracy and adhering to payer guidelines, healthcare organizations can increase the acceptance rate of claims.
- Higher First-Pass Acceptance Rate: Accurate coding ensures that claims are accepted on the first submission, reducing follow-up work.
- Real-Time Claim Validation: Automated tools help validate claims before submission, catching errors that could lead to denials.
- Fewer Denials and Rejections: Improved coding accuracy and adherence to payer rules minimize the chances of claims being rejected.
Reducing claim denials is crucial for streamlining revenue cycles, but several challenges can complicate the reimbursement process.
Identifying and addressing these hurdles is the next step in optimizing medical coding and reimbursement.
Also Read: Outpatient Medical Coding: 2025 Guide for Accurate Reimbursement
Challenges in Medical Reimbursement and Coding
From coding errors to compliance issues, healthcare organizations face obstacles that can slow down the revenue cycle and increase operational costs.
Here are the key challenges healthcare organizations face:
- High Denial Rates: Incorrect or incomplete coding leads to rejected claims, requiring time and resources for corrections and resubmission, delaying payments and increasing costs.
- Regulatory Complexity: Constant changes in coding standards, like ICD-10 updates and CMS guidelines, make compliance difficult, risking penalties and financial losses if missed.
- Manual Processes and Human Error: Manual coding increases the risk of mistakes, leading to underbilling, overbilling, or denied claims, disrupting revenue cycles.
- Inadequate Training and Knowledge Gaps: Coders must stay current with growing standards; a lack of training leads to incorrect coding, resulting in claim rejections and delayed reimbursements.
- Payer-Specific Requirements: Different payers have unique coding rules, making it time-consuming and complex to ensure each claim meets the required standards for payment.
- Documentation Gaps: Incomplete or unclear patient documentation complicates accurate coding, often resulting in claim denials and a longer reimbursement cycle.
Addressing these challenges is crucial for optimizing coding efficiency and ensuring proper reimbursement.
Effective solutions can streamline processes and improve financial outcomes across healthcare organizations.
6 Best Practices for Efficient Medical Reimbursement and Coding
Implementing best practices in medical reimbursement and coding can significantly reduce errors, improve claim acceptance rates, and streamline the revenue cycle.
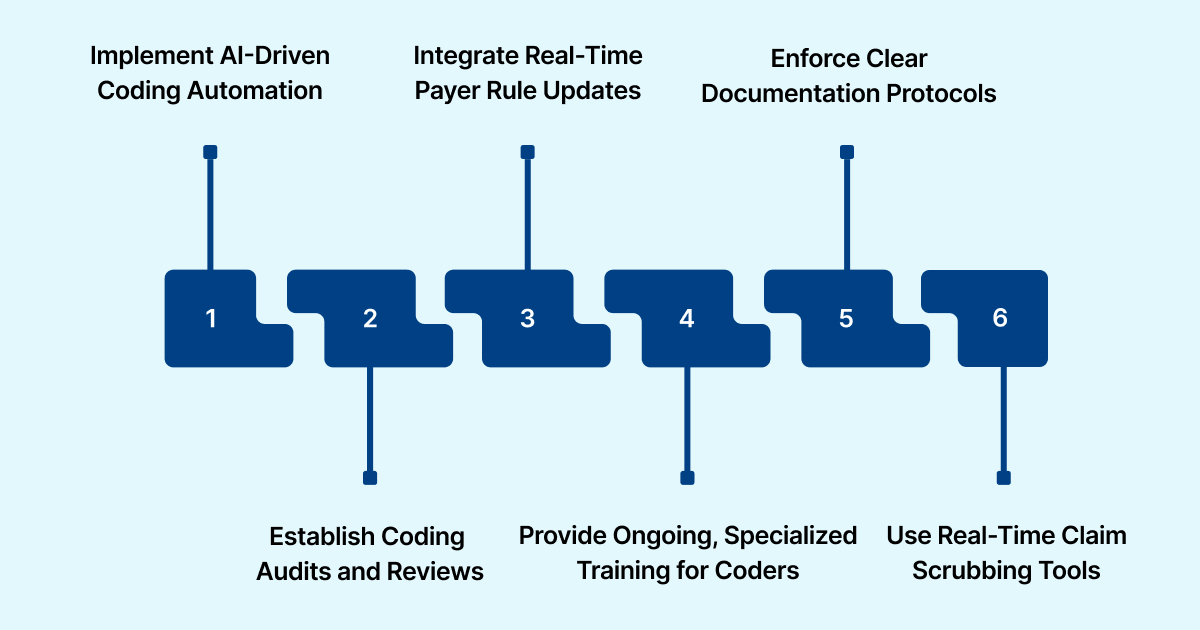
Here are some actionable best practices for improving efficiency in medical reimbursement and coding:
1. Implement AI-Driven Coding Automation
Use AI-powered tools like RapidClaim’s RapidCode to automate coding tasks, ensuring accurate code assignments at the speed of 1000+ charts per minute. This drastically reduces human error and improves claim accuracy.
2. Establish Coding Audits and Reviews
Perform regular internal audits to catch coding errors before submission. Set up a peer review system to verify code assignments, ensuring compliance with ICD-10 and CPT standards.
3. Integrate Real-Time Payer Rule Updates
Implement tools that automatically update payer-specific rules in your coding software, ensuring all claims adhere to the latest payer guidelines and reducing denials due to rule mismatches.
4. Provide Ongoing, Specialized Training for Coders
Ensure coders are trained in specific specialities, such as E&M coding or HCC risk adjustment, to improve coding accuracy and compliance with complex billing requirements for different medical specialities.
5. Enforce Clear Documentation Protocols
Create standard operating procedures for clinicians to ensure thorough and precise documentation.
Provide real-time feedback to healthcare providers when documentation is incomplete or unclear, minimizing documentation gaps.
6. Use Real-Time Claim Scrubbing Tools
Implement automated claim scrubbing tools like RapidScrub that catch coding errors and documentation gaps before submission, increasing first-pass claim acceptance and reducing follow-up work.
With these best practices in place, it's time to explore how tools like RapidClaims can help take these processes to the next level.
How Can RapidClaims Help Streamline Medical Coding and Reimbursement?
RapidClaims is an AI-powered medical coding solution designed to automate the coding process and improve reimbursements. With a clean claim rate of over 98% and 100% audit compliance, it helps reduce errors and streamline workflows.
Here’s how RapidClaims can help:
- Automates Coding with RapidCode: RapidCode processes 1000+ charts per minute, improving productivity by 170% and maintaining 96% coding accuracy.
- Real-Time Claim Validation with RapidScrub: RapidScrub reduces denials by 40%, accelerating the payment cycle and has 5-day faster recovery on A/R.
- Improves Compliance and Efficiency with RapidCDI: RapidCDI improves HCC capture by 24%, ensuring proper risk adjustment and maximizing reimbursement.
By incorporating RapidClaims tools, healthcare organizations can significantly improve coding accuracy, streamline reimbursement processes, and reduce operational costs.
Wrapping Up
Medical reimbursement and coding directly influence a healthcare organization's cash flow and operational efficiency. By improving coding accuracy and reducing claim denials, organizations can streamline their revenue cycles and boost reimbursements.
RapidClaims uses AI-driven solutions like RapidCode, RapidScrub, and RapidCDI to automate coding, enhance compliance, and speed up claim approvals, ensuring a more efficient reimbursement process.
Want to streamline your coding and maximize reimbursements? Schedule a Free Demo to see how RapidClaims can help!
FAQS
1. How can AI improve the accuracy of medical coding?
AI-powered tools analyze large volumes of patient data quickly, reducing human errors and ensuring more accurate code assignments, which leads to fewer claim denials and faster reimbursements.
2. What are the common reasons for claim denials in medical reimbursement?
Claim denials are often caused by incorrect coding, missing documentation, or failure to follow payer-specific rules. These issues delay payments and require additional administrative effort to resolve.
3. Can AI reduce the cost of medical coding?
Yes, AI can significantly lower coding costs by automating routine tasks, reducing the need for manual coders, and streamlining the overall coding process, leading to cost savings.
4. How does automation help with payer-specific coding requirements?
Automation ensures that the correct coding rules are applied based on payer-specific guidelines, which minimizes the risk of denials and improves claim approval rates.
5. Is real-time claim validation important for healthcare organizations?
Yes, real-time claim validation ensures that claims are accurate before submission, preventing costly rework, reducing denials, and speeding up the reimbursement cycle.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








