Outpatient Medical Coding: 2025 Guide for Accurate Reimbursement
Outpatient visits are increasing, payer scrutiny is intensifying, and every encounter now carries financial implications. That is why the U.S. medical coding market reached $21.89 billion in 2024, a clear indication of how essential accurate coding has become for sustainable revenue operations.
For healthcare professionals across coding and RCM, outpatient medical coding is now the backbone of clean claims, audit protection, and trustworthy clinical and financial data. As more procedures shift out of the inpatient setting, the margin for error becomes smaller, and the need for precise documentation becomes sharper.
In this blog, you'll learn the essentials of outpatient medical coding, its differences from inpatient coding, key workflows, significant compliance risks, and emerging RCM trends.
TL;DR (Key Takeaway)
- Coding Accuracy Matters: Accurate outpatient coding ensures correct reimbursement, audit compliance, and workflow efficiency. Errors increase denials and revenue loss.
- Documentation Alignment: Diagnosis, procedure codes, modifiers, POS, and encounter type must match clinical documentation to support claims and compliance.
- Follow Payer Rules: Time-based E/M updates, payer edits, and bundling rules directly affect claim approval and reimbursement.
- Use Technology Wisely: AI and computer-assisted coding enhance efficiency, but they still require human review for complex or nuanced cases.
- Continuous Oversight: Regular training, structured documentation, and audits minimize errors, prevent denials, and protect revenue integrity.
Table of Contents:
- What is Outpatient Medical Coding?
- Code Sets & Documentation Standards for Outpatient Coding
- Step-by-Step Workflow for Outpatient Medical Coding
- Common Challenges & Compliance Risks in Outpatient Coding
- Key Practices to Ensure Outpatient Coding Accuracy
- Future Trends in Outpatient Medical Coding
- Conclusion
- Frequently Asked Questions (FAQs)
What is Outpatient Medical Coding?
Outpatient medical coding is the process of assigning standardized alphanumeric codes to diagnoses, procedures, and services in a healthcare setting. It applies to ambulatory care encounters such as physician offices, hospital outpatient departments, ambulatory surgery centers, and urgent care visits. These codes translate clinical documentation into billable, reportable data used for claims submission, quality reporting, analytics, and regulatory audits.
Key Components:
- Diagnosis codes (e.g., ICD‑10‑CM)
- Procedure/service codes (e.g., CPT ® and HCPCS)
- Setting designation (place-of-service, outpatient facility vs. inpatient)
- Associated modifiers, documentation of encounter, and payer grouping
Why it matters: Reimbursement is heavily dependent on accurate outpatient code assignment, as payers increasingly scrutinize ambulatory claims, audit denials, and implement value-based payment models. That leads us directly into the next section: how it contrasts with inpatient medical coding, and why that difference matters.
Outpatient vs. Inpatient Medical Coding: Key Differences
Understanding the differences between outpatient and inpatient medical coding is crucial for healthcare providers. Each setting follows distinct rules, documentation requirements, and reimbursement methodologies, which directly impact coding accuracy, claim approval, and revenue cycle efficiency.
Here are the key differences between outpatient and inpatient coding:
- Encounter type and place of service: Inpatient coding focuses on hospital admissions, length of stay, and discharge summaries. Outpatient coding covers clinic visits, same-day procedures, ambulatory surgery, and observation units.
- Coding guidelines and sequencing logic: Outpatient coding focuses on the specific visit level, including evaluation and management (E/M) services and procedures associated with each encounter. Inpatient coding relies on diagnosis-related groups (DRGs) and follows distinct sequencing rules.
- Time and documentation considerations: Outpatient E/M codes now often use minimum time thresholds for code selection, affecting how time-based services are documented and billed. Inpatient coding relies more on comprehensive stay documentation and broader clinical narratives.
- Denial risk and volume: Outpatient encounters are high in volume, with multiple visits per day across varied specialties. Even minor coding errors can accumulate, increasing the risk of denial, particularly for ambulatory procedures.
Due to these differences, outpatient coders must be proficient in visit-specific documentation, accurate code selection, payer edits, and time-based coding rules to ensure accurate reimbursement and compliance.
Code Sets & Documentation Standards for Outpatient Coding
Outpatient coding relies on specific code sets and detailed documentation to ensure accurate billing, compliance, and reimbursement. Understanding these requirements is essential for coders, revenue cycle managers, and compliance officers.

1. Diagnosis Code Set: ICD-10-CM
The primary diagnosis code set used in the U.S. for ambulatory care is ICD-10-CM. For FY 2024, official guidelines were updated, and coders must follow sequencing rules and maintain full specificity to ensure accurate coding. Coders must also apply conventions, such as coding to the highest number of characters supported by documentation.
Documentation Implications:
- The provider’s note must clearly support the diagnosis, including laterality, complications, co-morbidities, and encounter type.
- Assigning “unspecified” codes is only appropriate when documentation lacks specificity, but may trigger payer scrutiny or affect quality metrics.
- Accurate linkage of diagnosis to procedure or service is required to demonstrate medical necessity for each outpatient encounter.
2. Procedure / Service Code Sets: CPT and HCPCS
Outpatient services use CPT Codes for physician services, office visits, and ambulatory procedures, while HCPCS codes cover supplies, durable medical equipment, and other ancillary services. According to the AMA, the 2024 CPT code set added 230 new codes, deleted 49, and revised 70, including significant changes to outpatient evaluation and management (E/M) codes.
Documentation Implications:
- Coders must select the appropriate CPT code based on either medical decision-making or total time spent, supported by clinical documentation.
- Procedure codes must accurately reflect the services performed and include proper modifiers, such as
- -25 for a significant E/M service on the same day as a procedure,
- -59 for distinct procedural services, and
- -26/-TC for professional or technical components.
- Payer-specific rules may require attachments or additional documentation for outpatient surgery, observation services, or specialized procedures.
3. Place of Service (POS) & Encounter Type
Accurate designation of place of service, such as POS 11 for office visits or POS 22 for outpatient hospital visits, is essential for reimbursement and compliance. Correct identification of encounter type, including new versus established patient or ambulatory surgery versus clinic visit, is also crucial. Both factors directly impact coding accuracy and claim approval.
Documentation Implications:
- Coders must verify that the POS and encounter type are accurately recorded, as errors may result in claim denials.
- The medical record should clearly document whether the patient is new or established to the practice. It should also specify the type of service, such as an office visit, surgery, observation stay, or other ambulatory encounter.
- Observation and same-day procedures often have bundling rules, requiring clear documentation of each service performed and its medical necessity.
4. Quality Reporting and Risk Adjustment
Accurate outpatient coding supports quality reporting, risk adjustment, and value-based care initiatives.
Documentation Implications:
- Proper coding affects preventive care compliance, chronic condition management, and patient safety indicators.
- Diagnosis codes are used to inform hierarchical condition categories (HCCs) and other risk models, which in turn influence reimbursement under value-based contracts.
- Complete documentation ensures adherence to CMS and commercial payer reporting requirements.
- Accurate coding reduces denials, payer audits, and penalties by demonstrating medical necessity and proper documentation.
Proper documentation is essential for a smooth reimbursement process. To further streamline outpatient medical coding, platforms like RapidClaims integrate with EHRs via SMART on FHIR and HL7. Its RapidCode AI assistant provides line-level rationales and coding suggestions, improving accuracy and reducing denials. Turbo Throughput processes 1,000+ charts per minute at 96 %+ audited accuracy and 170 % coder‑productivity lift, enabling faster and more reliable claim submission.
Let’s now walk through a step-by-step workflow that outpatient coders and RCM teams should follow to ensure timely reimbursement.
Step-by-Step Workflow for Outpatient Medical Coding
Efficient outpatient coding requires a structured approach to ensure accurate claims, compliance, and revenue capture. Following a clear workflow helps coders and RCM teams minimize errors, meet payer requirements, and support quality reporting.
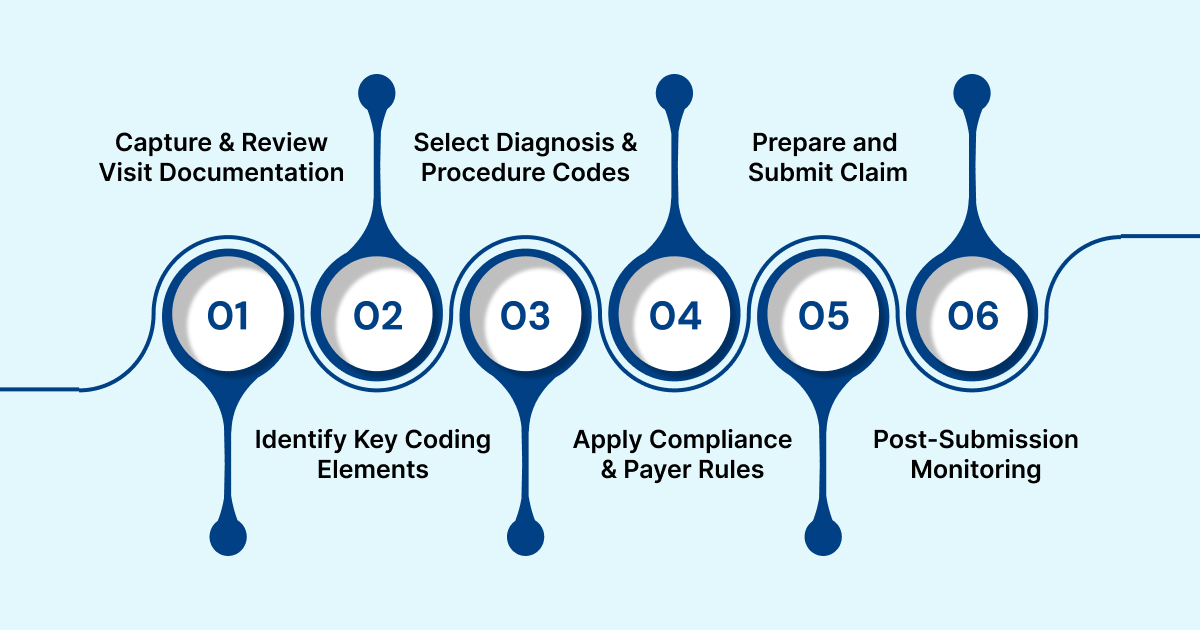
Step 1: Capture and Review Visit Documentation
Outpatient coders begin by obtaining clinician notes, order history, procedure notes, ancillary service details, and discharge or observation notes if applicable. Documentation must be complete, clearly show the patient’s status and encounter type, and support medical necessity for all services rendered.
Step 2: Identify Key Coding Elements
Coders determine the patient status (new vs. established), encounter type, diagnoses, procedures, place of service, and total time if using time-based E/M coding. They also assess the complexity of medical decision-making (MDM) to guide accurate code selection.
Step 3: Select Diagnosis and Procedure Codes
ICD-10-CM codes are assigned for the chief reason for the visit, secondary conditions, comorbidities, and symptoms, following sequencing and specificity guidelines. CPT and HCPCS codes are used to describe the services rendered. Coders must apply appropriate modifiers, such as -25, -59, -26/-TC, -GS, or -GQ, and clarify whether services are bundled or provided separately.
Step 4: Apply Compliance and Payer Rules
Coders review NCCI edits, payer-specific bundling rules, and local coverage determinations (LCDs). They ensure documentation supports code levels, aligns with provider credentials, meets medical necessity, and adheres to payer and regulatory requirements.
Step 5: Prepare and Submit Claim
Claims are prepared with the correct place of service, provider NPI, tax ID, affiliated facility if applicable, code fields, modifiers, and required attachments. The proper linkage between diagnosis and procedure codes is verified for both medical necessity and quality reporting purposes.
Step 6: Post-Submission Monitoring and Denial Management
Outpatient claims are monitored for denials, with errors such as incorrect modifiers, missing documentation, or wrong place of service identified. Coders respond to provider queries or claim revisions and utilize denial trends to enhance documentation, coding accuracy, and workflow efficiency.
Healthcare teams can further enhance efficiency and accuracy by adopting RapidClaims’ AI-powered platform. RapidCode delivers a 170 % productivity lift for coders with 96 %+ accuracy, while RapidScrub reduces denials by 40 % and accelerates A/R by five days. RapidCDI increases HCC capture by 24 % and saves physicians 30 minutes per day, reducing administrative burden and burnout. These measurable improvements enable staff to focus on higher-value tasks, enhance job satisfaction, and ensure compliance with regulations.
Also Read: Guide to Evaluation, Management, and Medical Billing Coding Services
Now, let’s explore the common challenges and compliance risks that outpatient coders and RCM teams face, and how they can impact accuracy and regulatory adherence.
Common Challenges & Compliance Risks in Outpatient Coding
Outpatient coding involves high-volume workflows across multiple specialties and care settings, creating challenges in documentation and code assignment. Coders, compliance officers, and RCM managers must address these challenges to ensure accuracy, proper reimbursement, and regulatory compliance.
- High Volume and Diverse Services: Outpatient coders manage a wide variety of encounters, including clinic visits, telehealth services, observation, and ambulatory surgery across multiple specialties. This diversity increases the potential for workflow errors.
- Time-Based E/M Changes: The 2024 CPT update changed outpatient office visit codes from time ranges to minimum time thresholds. Failure to document time or medical decision-making accurately can trigger audits.
- Place of Service and Setting Issues: Incorrect assignment of the place of service, such as reporting POS 11 instead of POS 22 for outpatient hospital visits, is a common error. This mistake can lead to underpayment or claim denials.
- Modifier Misuse: Outpatient codes often require modifiers for shared visits, split-billing, assistant surgeons, or multiple procedures. Misuse of modifiers frequently results in denials.
- Bundling and Unbundling Errors: Applying incorrect codes or billing separately for services that are bundled can trigger NCCI edits or payer denials, which can impact revenue and compliance.
Also Read: How to Choose the Right Practice Management System for Medical and Legal Workflows
Having understood these risks, we now move on to mitigation strategies and best practices in outpatient coding.
Key Practices to Ensure Outpatient Coding Accuracy
Implementing structured approaches helps coders maintain precision and efficiency. Here are five best practices to improve accuracy, revenue capture, and compliance in outpatient coding:
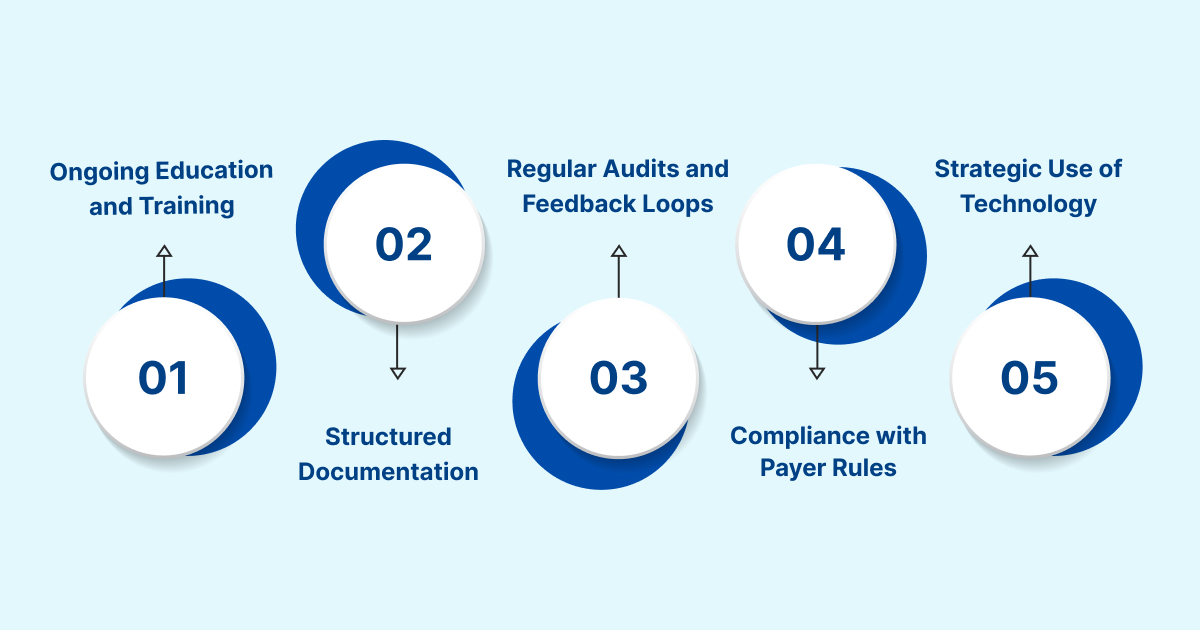
1. Ongoing Education and Training: Ensure coders and providers stay updated with annual CPT and ICD updates, payer-specific changes, and outpatient workflows, including time-based or MDM requirements for E/M coding.
2. Structured Documentation and Clinician Collaboration: Utilize reliable documentation templates to capture key elements, including time, MDM, procedures, modifiers, and place of service. Engage providers to clarify gaps and support medically necessary coding decisions.
3. Regular Audits and Feedback Loops: Conduct audits on claims to verify the correct place of service, code selection, modifier usage, bundling errors, and denial trends. Utilize audit findings to deliver targeted training and implement workflow enhancements.
4. Compliance with Payer Rules and Quality Reporting: Maintain updated references for payer-specific edits, observation and telehealth codes, and claim scrubbing logic. Accurate coding also supports quality reporting, population health analytics, and risk adjustment, aligning revenue with institutional strategy.
5. Strategic Use of Technology: Apply computer-assisted coding (CAC) or AI tools for high-volume, straightforward cases to improve efficiency. Human oversight remains critical for complex outpatient scenarios and nuanced documentation.
RapidClaims utilizes AI to automate revenue-cycle management, integrating clinical data with billing workflows. By minimizing manual errors and administrative burden, RapidClaims enables healthcare leaders to focus on strategic initiatives and enhance overall workflow efficiency.
Also Read: Guide to Evaluation, Management, and Medical Billing Coding Services
With those best practices in mind, it is essential to look ahead at what the future holds for outpatient coding.
Future Trends in Outpatient Medical Coding
Looking ahead, outpatient medical coding is expected to undergo significant evolution as care models expand and technology reshapes workflows. Key trends include:
1. Increased Automation and AI Adoption: Advanced natural language processing (NLP) and AI engines are being developed to handle outpatient coding at scale, thereby reducing manual effort and enhancing accuracy.
2. Greater Payer Scrutiny and Shifting Payment Models: Payers are expanding audits of outpatient claims and promoting value-based reimbursement models. They are also linking coding accuracy to metrics such as risk-adjusted outcomes and population health management.
3. Growing Role of Telehealth and Remote Encounters: As telehealth usage rises, coders must manage new code sets, modifier requirements, and documentation standards specific to virtual visits.
4. Integration of Data Analytics: Outpatient coded data increasingly feeds institutional analytics platforms, supporting quality improvement, workflow efficiency, and predictive modeling for denials, patient risk, and revenue leakage.
5. Workforce Evolution: The role of coders will shift from manual data entry to overseeing automation tools, managing exceptions, reviewing analytics, and ensuring compliance with changing regulations.
These emerging trends highlight that outpatient coding will become increasingly technology-driven and data-focused.
Conclusion
Outpatient medical coding is crucial for accurate reimbursement; however, errors in documentation, code selection, or modifier use can lead to denials and revenue loss. Following setting-specific rules, updated code sets, and audit requirements helps minimize these risks.
Integrating AI-driven platforms, such as RapidClaims, further optimizes workflow. With automated medical coding processes and seamless EHR integration, RapidClaims reduces errors, streamlines claims handling, and supports timely reimbursement.
Optimize your outpatient medical coding workflow with RapidClaims. Request a Free Demo today and see how AI can improve coding accuracy, identify missing details, and streamline documentation.
Frequently Asked Questions (FAQs)
1. How do observation stays affect outpatient coding and reimbursement?
A. Observation stays require distinct coding from full admissions, reflecting time, services, and setting. Accurate coding ensures correct reimbursement, prevents denials, and aligns with payer requirements for short-term monitoring. Documentation must clearly indicate medical necessity and duration of observation.
2. What are common coding errors in telehealth visits, and how can they be prevented?
A. Errors often involve incorrect CPT codes, missing telehealth modifiers, or incomplete documentation. Prevent errors by following updated telehealth guidelines, applying proper modifiers, and ensuring all virtual services are fully supported in the record.
3. How do NCCI edits influence outpatient coding decisions?
A. NCCI edits prevent the billing of mutually exclusive or bundled services. Coders must review edits to avoid denials, ensure compliance, and correctly sequence procedures, particularly when multiple services are performed on the same day.
4. Why is documentation of medical decision-making (MDM) essential for outpatient E/M codes?
A. MDM documentation guides the correct E/M code selection and justifies service complexity. Accurate recording protects against audits, supports medical necessity, and ensures proper reimbursement for outpatient encounters.
5. What are the risks of misusing CPT and HCPCS modifiers?
A. Incorrect modifiers can cause underpayment, claim denials, or audits. Proper use ensures accurate reimbursement, compliance with payer rules, and correct linkage between procedures and diagnoses.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






