Healthcare RPA Workflow Automation 2026 Guide

According to official U.S. government health expenditure data, total national health spending reached nearly $4.9 trillion in 2023 and accounted for approximately 17.6 percent of GDP, highlighting the scale and financial pressure of healthcare operations. For provider organizations, much of this pressure is concentrated in administrative and revenue cycle activities such as eligibility verification, medical coding, claims submission, and follow up. These workflows depend on accurate and timely data movement across EHRs, billing platforms, and payer systems, yet many still rely on manual steps that are slow, error prone, and difficult to scale.
As claim volumes increase and payer requirements continue to evolve, manual revenue cycle processes contribute to delayed reimbursement, higher denial rates, and inconsistent documentation quality. Revenue cycle teams spend significant time navigating systems, reconciling data, and resolving preventable issues instead of focusing on accuracy and compliance.
RPA workflow automation offers a structured way to standardize these processes, reduce administrative burden, and support more predictable revenue cycle performance when combined with AI tools that strengthen coding accuracy and documentation integrity.
Key Takeaways
- RPA workflow automation removes repetitive administrative steps across eligibility, coding preparation, claim edits, and status follow up, helping teams handle higher volumes with fewer delays.
- Pairing RPA with AI strengthens accuracy by interpreting clinical documentation, identifying coding gaps, and applying consistent payer rules across ICD 10, CPT, and HCC workflows.
- The most common barriers to manual RCM performance include fragmented data retrieval, inconsistent documentation flow, high coder variation, and complex payer requirements.
- A structured implementation approach built on workflow mapping, prioritization, integration planning, testing, and monitoring ensures smooth adoption with full HIPAA and CMS compliance.
- RPA and AI together deliver measurable gains in productivity, clean claim rates, denial reduction, reimbursement speed, and audit readiness across coding, CDI, and billing operations.
Table of Contents:
- Problem: Manual RCM and Coding Workflows Are Breaking
- Industry Challenge: Compliance, Labor Shortages, and Rising Costs
- Solution: How RPA Workflow Automation Works in Healthcare
- How AI Strengthens RPA in Coding, CDI, and Risk Adjustment
- Implementation Framework: Steps to Deploy RPA in RCM
- Benefits: Operational, Financial, and Compliance Gains
- Trends: The Future of RPA and AI in Healthcare
- Conclusion
- FAQs
Problem: Manual RCM and Coding Workflows Are Breaking
Revenue cycle performance depends on many tasks occurring accurately and on time. When these steps rely on manual work, even small inefficiencies disrupt downstream processes. Teams end up spending more time moving information than improving accuracy or preventing denials.
Key Workflow Breakdowns
- Fragmented data retrieval: Staff move between EHR screens, payer portals, and internal tools to collect information needed for eligibility, coding, and claims.
- Inconsistent documentation flow: Notes, attachments, and supplemental records arrive in different formats and at different times, creating delays in coding and claim preparation.
- Manual coding interpretation: Coders must read lengthy clinical narratives, verify historical conditions, and apply ICD 10, CPT, and HCC rules without automated support.
- High variation across coders and billers: Differences in experience and interpretation lead to inconsistent code assignment and irregular claim quality.
- Manual claim review and edit resolution: Staff compare payer rules, correct edits, and validate documentation by hand, increasing the time to final submission.
- Rework caused by upstream issues: Any errors in documentation, coding, or edits surface later as denials, requiring significant reprocessing time.
These issues make it difficult for teams to maintain consistent output and meet growing payer and compliance demands.
If these workflow pressures are creating backlogs or inconsistencies, this is often the point where organizations begin evaluating which tasks are strong candidates for automation.
Industry Challenge: Compliance, Labor Shortages, and Rising Costs
Beyond internal workflow issues, healthcare organizations face external pressures that make manual revenue cycle operations increasingly difficult to sustain. These challenges affect accuracy, capacity, and financial performance, regardless of organization size.
Compliance Complexity
- Frequent updates to CMS billing rules, ICD 10 guidance, CPT changes, and HCC v28 requirements
- Growing documentation standards across inpatient, outpatient, and risk adjustment programs
- Increased scrutiny from payers that require precise linkage between clinical notes and assigned codes
- Higher expectations for audit readiness and consistent application of coverage policies
These evolving requirements demand a level of consistency that manual workflows struggle to maintain.
Labor Shortages
- Limited availability of certified coders, CDI professionals, and skilled RCM analysts
- Experienced staff often carry higher caseloads, which increases error risk
- High turnover disrupts workflow continuity and creates onboarding gaps
- Organizations struggle to scale operations during seasonal or service-line growth
Labor constraints directly limit throughput and slow down reimbursement cycles.
Rising Administrative Costs
- Significant staff time spent navigating payer portals and internal systems
- Increased workload to address edits, documentation gaps, and preventable denials
- Additional oversight required to maintain quality and compliance across teams
- Higher operational costs due to rework and manual exception handling
These rising costs reduce financial flexibility and place pressure on margins.
Also read: Healthcare Revenue Cycle Outsourcing: A Complete 2026 Guide
Solution: How RPA Workflow Automation Works in Healthcare
RPA allows software bots to perform structured, rule based tasks that typically require staff to navigate multiple systems, gather information, and complete repetitive steps. When applied to the revenue cycle, RPA standardizes how data moves through each stage of the encounter and reduces manual effort that often slows down reimbursement.
What RPA Automates in Revenue Cycle Workflows
- Eligibility and benefits verification: Bots extract patient and insurance information, check payer portals, and update EHR fields with verified data.
- Document gathering for coding
Bots collect notes, attachments, lab results, and relevant encounter data for coding and CDI teams. - Charge capture assistance: Structured fields such as medications, procedures, and vitals can be identified and routed for validation.
- Claim preparation and edit checks: Bots populate claim fields, run payer specific edits, and flag errors before submission.
- Claim status monitoring: Bots check payer portals, document status changes, and surface denials or requests for information.
- Exception routing: Any item that requires human review is routed to the correct team member with supporting information.
These automations create consistent workflows, reduce processing time, and support higher clean claim rates.
How AI Strengthens RPA in Coding, CDI, and Risk Adjustment
RPA alone handles rule driven tasks, but it cannot interpret clinical language or identify coding nuances. When paired with AI, automation becomes capable of supporting more complex RCM and coding functions.
Where RapidClaims Fits Into the Workflow
RapidClaims modules complement RPA by adding clinical and coding intelligence at key points in the process.
- RapidCode: Interprets clinical documentation, identifies diagnoses and procedures, and generates code suggestions for coder review.
- RapidScrub: Applies automated compliance checks, NCCI logic, modifier accuracy checks, and payer specific edits before claims are submitted.
- RapidRecovery: Supports denial recovery by prioritizing recoverable claims, assisting with appeal workflows, and helping organizations recapture revenue that would otherwise be written off. Insights from recovered denials can also be used to improve upstream prevention efforts.
- RapidCDI: Reviews documentation quality, flags inconsistencies, and highlights missing clinical elements that coders and CDI teams must validate.
When integrated with RPA, these tools create an end to end workflow where bots manage navigation and data movement while AI ensures coding accuracy, documentation completeness, and compliance alignment.
Must read: Top Affordable Billing Solutions for Small Medical Practices
Implementation Framework: Steps to Deploy RPA in RCM
A successful RPA rollout requires clear workflow structure, defined responsibilities, and careful validation. The goal is to introduce automation without disrupting ongoing revenue cycle operations.
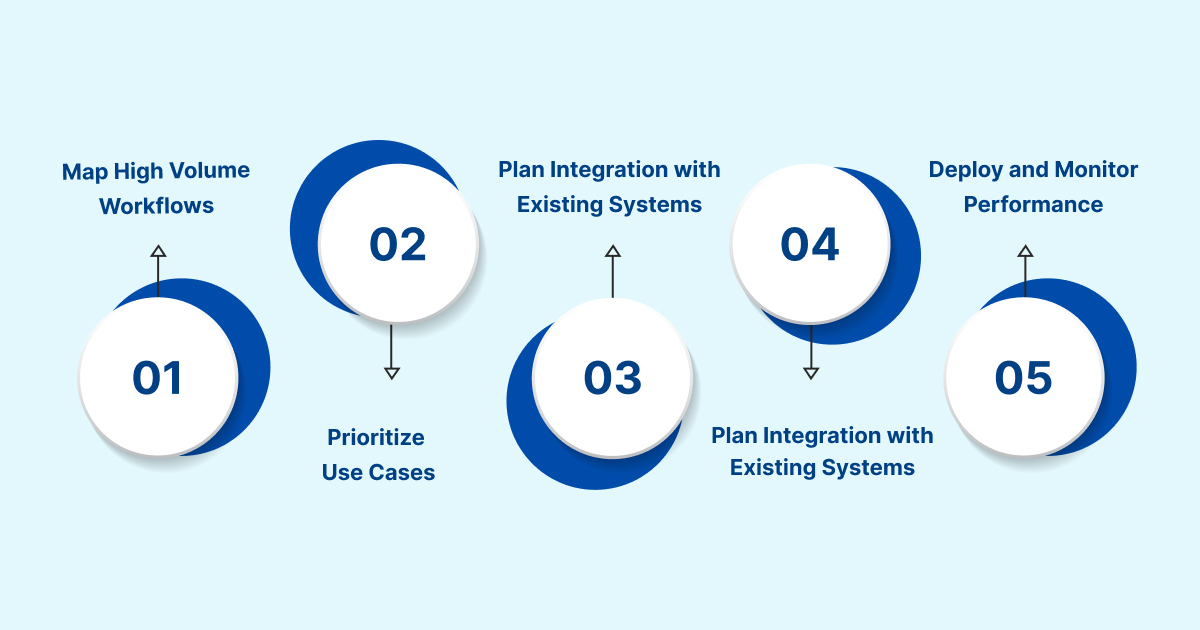
1. Map High Volume Workflows
Identify tasks that follow consistent rules and create the most administrative burden. Document required inputs, system steps, and handoffs. This establishes the baseline for automation design.
2. Prioritize Use Cases
Select workflows that offer measurable impact, such as eligibility checks, claim status review, coding preparation, or denial handling. Start with processes that have predictable logic and meaningful time savings.
3. Plan Integration with Existing Systems
Determine how bots will access the EHR, billing platforms, and payer portals. Confirm alignment with HIPAA, user permissions, and audit logging. Validate compatibility with HL7 and FHIR connections where needed.
4. Build and Test Bot Behavior
Develop the step by step logic the bot will follow. Test in a non production environment to confirm data accuracy, system stability, and proper routing of exceptions. Refine rules based on coder and RCM feedback.
5. Deploy and Monitor Performance
Roll out automation in phases and monitor throughput, accuracy, and exception volume. Use operational dashboards to track improvements and adjust workflows as payer rules evolve.
If you are planning an RPA project, a structured framework like RapidClaims helps teams adopt automation with minimal disruption while maintaining compliance and data integrity.
Benefits: Operational, Financial, and Compliance Gains
RPA provides measurable improvements across the revenue cycle by reducing manual effort, improving consistency, and strengthening accuracy. When paired with AI, these gains expand across coding, documentation, and risk adjustment workflows.
Operational Benefits
- more predictable throughput across coding and billing
- fewer delays caused by manual data collection
- reduced dependency on portal navigation and repetitive system steps
- faster movement of encounters from documentation to claim submission
Financial Benefits
- lower cost to process high volume administrative tasks
- improved clean claim rates through standardized edits and fewer errors
- reduced denial frequency due to more complete and consistent submissions
- shorter reimbursement timelines as workflows become more efficient
Compliance Benefits
- consistent application of payer rules and CMS guidelines
- improved documentation alignment with ICD 10, CPT, and HCC requirements
- stronger audit trails for both automated and human actions
- fewer compliance risks from variation in manual decisions
If these outcomes align with your organizational goals, a targeted automation pilot like RapidClaims can help validate impact before expanding to additional workflows.
Trends: The Future of RPA and AI in Healthcare
The next phase of RCM modernization is driven by the combination of structured automation and advanced clinical intelligence. Several trends are shaping how organizations plan their automation strategies.
Intelligent Automation Becomes Standard
RPA is increasingly combined with AI tools that interpret clinical documentation, identify coding gaps, and predict billing outcomes. This creates workflows where routine tasks are automated and complex decisions are supported with data driven insights.
Shift Toward Unified RCM Platforms
Health systems are consolidating separate tools for coding, scrubbing, CDI review, and denial prevention. Integrated platforms reduce handoffs, minimize system switching, and improve data flow from documentation to claim submission.
Broader Adoption of FHIR for Integration
More organizations are adopting FHIR based interfaces to streamline data exchange between EHRs, payer systems, and automation tools. This supports cleaner claims and reduces the effort required to maintain integrations.
Workforce Augmentation Becomes a Priority
Rather than replacing staff, automation is being used to stabilize workloads and reduce burnout. Teams rely on RPA for repetitive steps while focusing their expertise on coding quality, documentation review, audits, and complex cases.
If you are preparing for the next stage of automation, understanding these trends can help identify where to focus your modernization efforts.
Conclusion
RPA and AI are reshaping how healthcare organizations manage coding, billing, and the broader revenue cycle. As payer requirements evolve and administrative workloads grow, manual processes create delays, inconsistencies, and preventable denials. Automation offers a structured way to support accuracy, strengthen compliance, and create predictable throughput across high volume workflows.
By combining RPA for system navigation and task automation with AI tools that understand clinical documentation and coding requirements, organizations can move toward a more resilient and efficient revenue cycle. This approach supports staff, enhances documentation quality, and reduces the time and effort needed to move encounters from clinical notes to clean claims.
If your organization is evaluating how to modernize RCM performance, improve coding accuracy, or reduce avoidable denials, RapidClaims can help map an automation plan that fits your existing workflows and compliance needs. Connect to explore how a combined RPA and AI approach can support your team’s goals.
FAQs
Q: How do organizations decide which RCM workflows to automate first?
A: Most teams begin with repetitive, rule based tasks that create predictable backlogs, such as eligibility checks, claim status review, coding preparation, and basic denial routing. These workflows offer clear logic, high volume, and fast measurable impact, which makes them ideal entry points for RPA.
Q: Can RPA support coding accuracy without replacing coders?
A: Yes. RPA handles structured tasks like gathering documentation and preparing chart components, while coders apply clinical judgment. When paired with AI tools that interpret provider notes and surface coding clues, RPA helps coders work more consistently and with fewer manual steps.
Q: How does automation reduce avoidable denials?
A: RPA supports consistency by ensuring payer edits, documentation requirements, and coding rules are applied the same way every time. This reduces errors that commonly lead to technical denials, such as missing attachments, incorrect member information, or incomplete coding details.
Q: What does RPA integration look like with major EHRs?
A: Bots typically access the EHR through user level permissions and follow defined process steps, similar to a staff member. Organizations may also use HL7 or FHIR where available to streamline data flow. The design is structured around security, audit trails, and minimal workflow disruption.
Q: How do teams monitor automated workflows to ensure accuracy?
A: RCM leaders use dashboards and audit logs to track bot throughput, exception volume, and error rates. Any items that require escalation are routed to the appropriate team member. Regular reviews ensure workflows remain aligned with payer updates and policy changes.
Q: What skills do teams need to manage RPA after deployment?
A: Most organizations assign operational leads who understand the workflows and can validate exceptions. Technical support may be needed for bot updates or integration changes, but day to day oversight focuses on workflow performance, quality, and compliance alignment.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








