Healthcare Revenue Cycle Outsourcing: A Complete 2026 Guide
Did you know that 41% of U.S. health system financial leaders reported claim denial rates above 3.1% in 2024? As payer rules become increasingly challenging and staffing shortages intensify, even well-managed hospitals struggle to maintain billing accuracy, compliance, and cash flow efficiency.
Rising administrative and reimbursement pressures are driving healthcare organizations to outsource revenue cycle operations to specialized partners capable of streamlining coding, claims, and payment workflows. By adopting automation, analytics, and expert teams, providers aim to reduce denials, shorten A/R days, and focus more on patient care than on paperwork.
In this blog, you’ll explore how healthcare revenue cycle outsourcing works and why more U.S. providers are turning to it for operational and financial efficiency. You’ll also learn about its key benefits, potential risks, and practical steps to choose the right outsourcing partner for long-term success in the revenue cycle.
TL;DR (Key Takeaways)
- Revenue Performance Boost: Outsourcing billing, coding, and claims management reduces denials, shortens accounts receivable days, and speeds up reimbursements.
- Addressing Staffing Gaps: Providers can fill shortages of trained coders and billing staff, maintaining accuracy and compliance.
- Technology-Driven Efficiency: Partners offer AI, automation, and analytics platforms to enhance claim accuracy and informed decision-making.
- Risk and Compliance Management: Strong governance and oversight ensure data security, regulatory adherence, and consistent revenue capture.
- Strategic Vendor Selection: Define goals, evaluate capabilities, and track metrics to maximize ROI and align outsourcing with organizational priorities.
Table of Contents:
- What is Healthcare Revenue Cycle Outsourcing?
- Why Healthcare Organizations Outsource the Revenue Cycle?
- Key Revenue Cycle Functions Typically Outsourced
- How Outsourcing Models Work in Practice?
- Key Benefits of Healthcare Revenue Cycle Outsourcing
- Key Risks & Challenges of Healthcare Revenue Cycle Outsourcing
- How to Choose the Right Revenue Cycle Outsourcing Partner?
- Conclusion
- Frequently Asked Questions (FAQs)
What is Healthcare Revenue Cycle Outsourcing?
Healthcare revenue cycle outsourcing involves hiring a specialized third-party partner to handle critical financial and administrative processes, from patient registration to final payment collection and reconciliation. These functions may include eligibility checks, coding, claims submission, denial management, and patient billing.
The goal is to enhance efficiency, ensure compliance, and improve cash flow by relying on external expertise, technology, and scalable resources. This allows healthcare providers to focus more on delivering quality care than managing complex back-office operations.
Next, let’s understand why more U.S. healthcare organizations are choosing to outsource their revenue cycle in today’s financial environment.
Why Healthcare Organizations Outsource the Revenue Cycle?
Healthcare organizations face pressure to improve financial performance while handling complex payer rules and staffing gaps. Outsourcing revenue cycle operations reduces claim denials, accelerates reimbursement, and allows staff to focus on patient care.
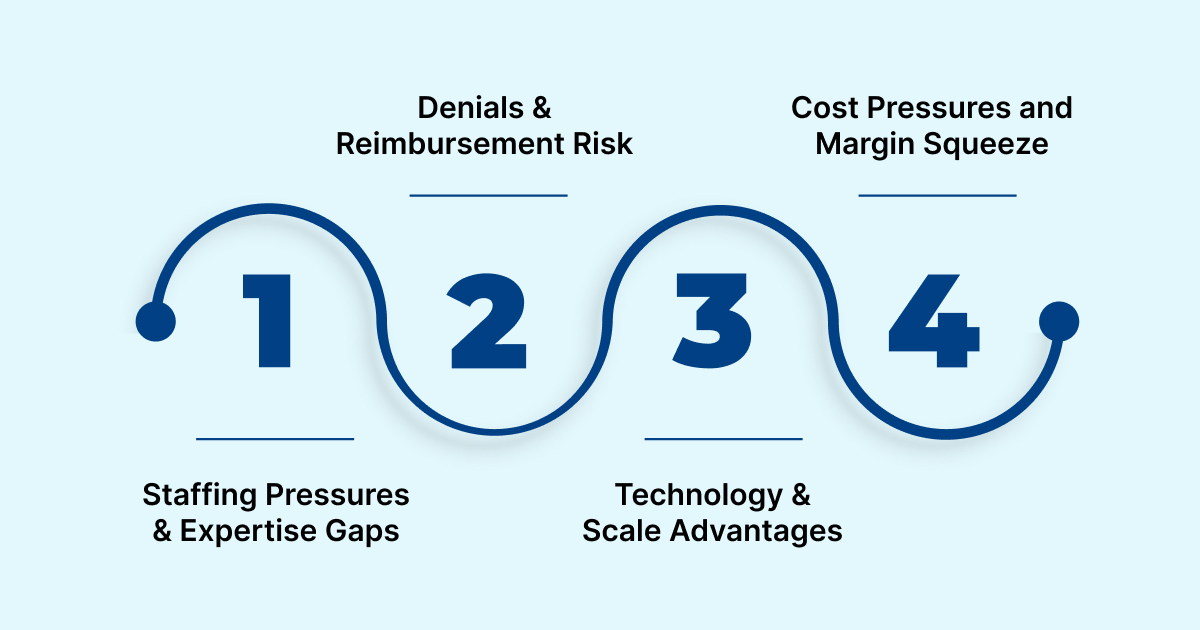
Several factors are driving the increasing adoption of healthcare revenue cycle outsourcing in the U.S.:
- Staffing Pressures and Expertise Gaps
Many healthcare organizations face shortages of experienced staff in billing, coding, and credentialing. Guidehouse’s 2024 report shows 71% of leaders are satisfied with their outsourcing partners, making outsourcing the top strategy for addressing staffing gaps.
- Denials and Reimbursement Risk
Payers are scrutinizing claims more closely, focusing on documentation of medical necessity, prior authorizations, and compliance with billing edits. This drives up denial rates, prolongs accounts receivable, and affects cash flow. Outsourcing vendors bring specialized workflows, analytics, and denial-resolution expertise that mitigate these risks.
- Technology and Scale Advantages
Smaller providers often cannot justify investing in advanced automation, AI, and analytics platforms internally. Outsourcing partners provide access to these technologies, enabling predictive denial management, automated claim scrubbing, and data-driven insights into the revenue cycle.
- Cost Pressures and Margin Squeeze
With operating costs rising and reimbursement growth limited, providers face pressure to control overhead. Delegating non-core revenue cycle functions to specialized partners allows predictable costs, optimized workflows, and improved net collections.
Also Read: From Chaos to Clarity: How AI in Medical Coding Enhances Accuracy
Recognizing these drivers helps us explore which revenue cycle functions are commonly outsourced and how various outsourcing models are implemented in practice.
Key Revenue Cycle Functions Typically Outsourced
Outsourcing in the revenue cycle is a targeted strategy, not a full handoff. Most U.S. healthcare organizations outsource specific areas where administrative errors, staffing gaps, or compliance risks directly impact reimbursement. These high-volume processes require payer-specific expertise and consistent execution to ensure optimal results.

Below are the key revenue cycle functions most commonly outsourced by healthcare providers to improve accuracy, compliance, and financial outcomes.
1. Eligibility and Pre-Registration
This front-end function ensures insurance coverage is verified, benefits are confirmed, and prior authorizations are obtained before services are rendered. It prevents claim denials downstream by identifying eligibility or documentation gaps early.
2. Charge Capture and Coding
Accurate charge capture and medical coding (ICD-10, CPT, HCPCS) are vital for compliant billing. Outsourced coding teams frequently utilize audit tools and computer-assisted coding (CAC) systems to enhance accuracy and mitigate compliance risks.
3. Claims Submission and Follow-Up
Vendors prepare, submit, and electronically scrub claims to payers, then monitor their progress through clearinghouses. They manage rejections, correct edits, and ensure timely resubmission to maintain a high clean-claim rate.
4. Denial Management and Appeals
Denials are analyzed at the root-cause level by payer, reason code, or department to prevent recurrence. Outsourced teams manage appeal letters, medical documentation, and follow-ups to recover lost revenue efficiently.
5. Patient Billing, Collections, and Payment Posting
Vendors handle patient statements, inbound billing calls, payment plans, and reconciliation activities. This approach improves patient experience, reduces collection delays, and ensures accurate posting to the general ledger.
6. Reporting and Analytics
Outsourced partners provide dashboards and performance metrics, including A/R days, denial rates, and collection ratios. These insights enable provider leadership to track revenue health and continuously optimize processes.
Many providers turn to AI-driven platforms to efficiently handle these outsourced functions. RapidClaims is one such platform that automates coding, denial prevention, clinical documentation, and recovery. Its modular tools, RapidCode, RapidCDI, RapidScrub, and RapidRecovery, deliver measurable improvements in cash flow, clean-claim rates, and efficiency across both FFS and value-based care models.
How Outsourcing Models Work in Practice?
Once providers decide which revenue cycle functions to delegate, the next step is determining how outsourcing will be structured. The chosen model establishes control, visibility, and accountability across RCM operations, influencing technology use, staffing, and compliance oversight.
Below are the primary outsourcing models healthcare organizations adopt based on their scale, internal expertise, and long-term financial objectives.
1. Full-Service or End-to-End Model: In this model, the vendor manages the entire revenue cycle, from patient scheduling to collections. It is common among large health systems or physician groups seeking to reduce administrative complexity and achieve predictable revenue outcomes.
2. Selective Outsourcing: Providers outsource specific pain points such as coding, claim follow-up, or denial management while retaining other functions in-house. This model is best suited for organizations with partial internal capability but needing targeted expertise.
3. Hybrid or Shared Model: In this model, the provider and vendor share responsibilities. For example, the provider manages patient access, while the vendor handles billing, posting, and analytics. It allows flexibility while preserving visibility into core operations.
4. Technology-Platform Model: The vendor supplies a revenue cycle technology stack, including automation, analytics, and workflow tools, while the provider’s staff continues performing daily tasks. This model suits organizations that prioritize technology enablement without large-scale outsourcing transitions.
Now that you know which functions are outsourced and how models work, let’s explore the major benefits healthcare organizations achieve through revenue cycle outsourcing.
Key Benefits of Healthcare Revenue Cycle Outsourcing
Outsourcing revenue cycle functions helps providers reduce denials, accelerate cash flow, and improve coding accuracy, while delivering actionable analytics and easing internal staffing burdens. Here are some key benefits organizations typically achieve:

1. Improved Cash Flow and Collections
Outsourcing enhances revenue capture and payment turnaround through structured workflows and denial prevention.
- Higher clean-claim rates through automated claim scrubbing and expert review
- Reduced A/R days with dedicated follow-up and appeal management
- Lower write-offs due to systematic denial resolution and payment reconciliation
2. Access to Specialized Expertise and Workforce Scalability
Vendors possess in-depth knowledge of the revenue cycle and regulations across various payer segments.
- Certified coders and billing experts who stay current on CMS and payer rule changes
- Scalable staffing models that adjust to claim volume and seasonal demand
- Reduced overtime and administrative costs for in-house teams
3. Advanced Technology and Analytics Without Capital Investment
Providers gain access to enterprise-grade automation and analytics tools without incurring upfront costs.
- AI and RPA-based claim tracking, denial prediction, and workflow optimization
- Real-time dashboards for visibility into collection trends and bottlenecks
- Benchmarking and forecasting to support financial planning and compliance
4. Compliance and Risk Mitigation
Outsourced partners maintain strict oversight of regulatory and documentation standards.
- Adherence to HIPAA, CMS, and payer documentation requirements
- Regular audit support, coding quality checks, and denial prevention reviews
- Reduced exposure to penalties or payer recoupments
5. Refocused Attention on Patient Care
By offloading administrative tasks, clinical and leadership teams can redirect time toward strategic and care-related priorities.
- More resources for quality improvement and patient engagement
- Reduced administrative burden on medical and billing staff
- More substantial alignment with organizational care goals
Many providers achieve these benefits more quickly and efficiently by adopting AI-powered platforms, such as RapidClaims. Its modular suite delivers measurable results: a 98 % clean-claim rate, 170 % coder productivity lift, 40 % denial reduction, and 24 % HCC capture improvement. By automating coding, documentation, denial prevention, and recovery, RapidClaims accelerates cash flow, reduces administrative costs, and ensures compliance while supporting overall revenue cycle efficiency.
Key Risks & Challenges of Healthcare Revenue Cycle Outsourcing
Outsourcing revenue cycle functions offers efficiency and scalability but also introduces operational, financial, and compliance risks. U.S. healthcare providers must recognize these challenges early and establish strong governance, vendor accountability, and data safeguards to maintain performance integrity and compliance across outsourced processes.
- Loss of Control and Transparency: When core billing and coding operations are transferred, providers lose real-time oversight of workflows, productivity, and revenue leakage. Misaligned KPIs or opaque reporting can affect decision-making.
- Vendor Capability and Performance Risk: Some vendors overpromise collection gains but underperform due to weak offshore oversight or a lack of payer-specific expertise. Inconsistent training or gaps in coder certification can erode accuracy.
- Data Security and System Integration Gaps: Transmitting PHI and financial data across systems introduces risks related to HIPAA and cybersecurity. Poor EHR integration can cause data mismatches or claim delays.
- Hidden Costs and Contractual Complexity: RCM outsourcing often includes complex fee structures (percentage of collections, gain-share, or transaction-based pricing). Unclear terms can inflate the total cost of ownership.
- Impact on Workforce and Organizational Culture: Outsourcing may lead to internal job displacement, a decline in morale, and fragmented collaboration between onshore staff and vendor teams. Knowledge gaps about local payers may persist.
Also Read: Guide to Evaluation, Management, and Medical Billing Coding Services
Understanding these risks is essential, but effective mitigation begins with selecting the right outsourcing partner. Let’s take a closer look at how to evaluate and choose the best fit.
How to Choose the Right Revenue Cycle Outsourcing Partner?
Selecting the ideal outsourcing partner is crucial for mitigating risks and achieving tangible financial and operational improvements. A structured evaluation process helps align vendor capabilities with your organization’s strategic goals, compliance requirements, and operational needs.
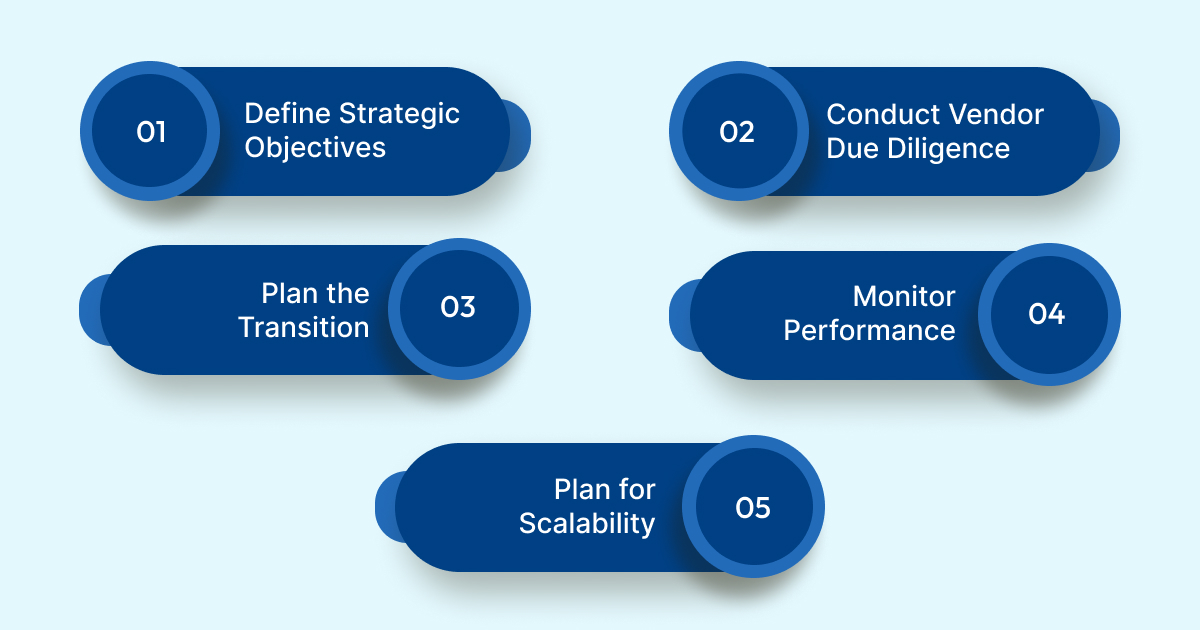
Step 1: Define Strategic Objectives and Metrics
Before engaging vendors, clearly outline your goals and the metrics you will use to measure success.
- Set Specific Targets: Reduce A/R > 90 days by 20%, improve clean-claim rates to 95%, or lower denial rates below 2%.
- Establish Governance: Agree on KPIs, reporting cadence, and escalation protocols.
- Ensure Compliance Alignment: Align with internal audit, compliance, and data security policies to ensure seamless integration and adherence to regulations.
Step 2: Conduct Vendor Due Diligence
Thoroughly assess potential vendors to ensure capability and fit.
- Track Record Review: Assess experience with U.S. provider organizations of similar size and scope.
- Performance Metrics: Analyze net collection rate, clean-claim submission rate, days in A/R, denial appeals success, and cost per claim.
- Certifications Verification: Confirm HIPAA, HITRUST, SOC 2, and internal audit compliance.
- Technology Stack Assessment: Review claim scrubbing tools, automation, analytics, and dashboards.
- Staffing Model Evaluation: Understand onshore vs offshore staff, payer expertise, and language/time-zone alignment.
- Contract Analysis: Examine pricing models, gain-share elements, SLAs, termination rights, confidentiality, and data ownership.
Step 3: Plan the Transition and Change Management
A structured transition reduces disruption and ensures continuity of operations.
- Detailed Transition Plan: Map knowledge transfer, system integration, process mapping, testing, and cut-over.
- Internal Oversight: Assign a revenue cycle manager, IT liaison, and compliance officer to oversee vendor activities.
- Stakeholder Communication: Inform coding, billing, clinical, and compliance teams; communicate with patients if applicable.
- Contingency Planning: Prepare for go-live issues, system delays, or data discrepancies.
Step 4: Monitor Performance and Governance
Ongoing oversight ensures that the vendor meets expectations and continually improves its processes.
- Joint Governance Committee: Review KPIs, address issues, and drive continuous improvement.
- Data-Driven Tracking: Utilize dashboards and analytics to pinpoint the root causes of denials or delays.
- Compliance Audits: Maintain audit trails, coding quality reviews, and periodic compliance checks.
- Annual Contract Review: Reassess vendor performance against benchmarks and market standards.
Step 5: Plan for Scalability and Innovation
Ensure the vendor can support evolving business and regulatory requirements.
- Adaptation to Policy Changes: Ensure vendor keeps pace with payer policy updates, automation, AI adoption, and value-based workflows.
- Scalable Operations: Confirm the vendor can expand or adjust staffing and services in response to growth or service shifts, such as telehealth, ambulatory expansion, or bundled payments.
- Strategic Analytics: Access actionable insights on payer performance, patient liability trends, and denial root causes.
Also Read: AI and Automation in Denial Management for Healthcare
Through careful evaluation and structured selection, providers can optimize revenue recovery, ensure compliance, and minimize operational risk. Next, we’ll examine future trends and considerations shaping healthcare revenue cycle outsourcing.
Conclusion
Healthcare Revenue Cycle Outsourcing enables providers to tackle staffing gaps, reduce claim denials, and expedite reimbursements. Revenue cycle managers, coders, and compliance officers should establish clear goals, thoroughly assess vendors, and closely monitor performance. When done effectively, outsourcing enables teams to focus on efficient financial operations while supporting high-quality patient care.
Platforms like RapidClaims make this process even more efficient by streamlining claims processing, reducing denials, and maintaining audit readiness while ensuring regulatory compliance. Using AI-powered automation across charge capture, denial prediction, and appeals, RapidClaims optimizes every step of the revenue cycle.
Ready to increase revenue, cut denials by up to 70%, and streamline your healthcare operations? Request a free demo today to see how RapidClaims empowers your staff and strengthens your revenue cycle.
Frequently Asked Questions (FAQs)
Q. How do I determine whether I should outsource only part of my revenue cycle or the entire cycle?
A. Start by mapping your internal processes and identifying significant inefficiencies, such as high denial rates or long A/R days. Compare these gaps with vendor capabilities to determine whether to opt for partial or full outsourcing. The choice depends on your organization’s risk tolerance, available resources, and strategic goals.
Q. What benchmarks should I use to evaluate the vendor once I’ve outsourced?
A. Track metrics like first‑pass claim acceptance, average days in A/R, denial trends, cost‑to‑collect, and patient balance resolution time. These measures help you compare vendor performance against your historical baseline and industry standards, ensuring the partner delivers real improvements.
Q. Can I retain control over patient communications if I outsource revenue cycle operations?
A. Yes. A credible outsourcing partner will support you in defining clear governance, escalation paths, reporting frequency, and communication protocols. Maintaining control over strategy and patient‑facing messaging remains your responsibility, and the vendor should operate as an extension of your team rather than a black‑box service.
Q. What risks do I face around data security and compliance when I outsource the revenue cycle?
A. You face potential risks around PHI breaches, HIPAA violations, SOC 2 or ISO 27001 non‑compliance, and a lack of audit trail transparency. To mitigate this, you should require vendor certifications, regular third‑party audits, clear data handling processes, and contractual rights to audit their systems and controls.
Q. How do I estimate the cost‑benefit of outsourcing versus keeping the revenue cycle in‑house?
A. You should calculate the total cost of your current operations, including staff, training, software, and infrastructure. Compare this to the vendor’s cost plus expected gains, such as lower denials, faster cash flow, and fewer write-offs. Include transition costs and analyze the payback period and ROI to make an informed decision.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






