Revenue Cycle Management in Healthcare: A 2025-2026 Guide

Do you know that nearly half of healthcare leaders reported a net collection yield of 93% or less in 2024? In the U.S. healthcare system, managing the revenue cycle effectively means bridging the gap between clinical care, accurate coding, and financial operations.
For medical coders, revenue cycle managers, and compliance officers, understanding how coding integrates into each stage of the revenue cycle is essential. This knowledge helps ensure revenue is protected and that the organization remains compliant with regulatory requirements.
In this blog, you’ll learn the ten key stages of revenue cycle management, common challenges, and best practices to reduce denials and speed reimbursements.
TL;DR (Key Takeaway)
- Coding Accuracy: Accurate medical coding ensures the correct submission of claims, timely reimbursement, and regulatory compliance.
- Workflow Optimization: Structured workflows and proactive denial management reduce errors and accelerate revenue collection.
- Technology Integration: EHRs, coding software, analytics dashboards, and patient engagement platforms improve efficiency and compliance.
- Staff Training and Automation: Continuous training, cross-skilling, and automation help mitigate risks associated with turnover and evolving payer requirements.
- Data-Driven Decision Making: Real-time monitoring of denial trends, A/R aging, and claim metrics enables workflow optimization and revenue protection.
Table of Contents:
- What is Revenue Cycle Management (RCM)?
- How Revenue Cycle Management Benefits Healthcare Operations?
- 10 Key Stages of the Healthcare Revenue Management Cycle
- Challenges in Healthcare RCM and How to Overcome Them
- Key Technology Solutions for Optimizing Revenue Cycle Management
- Final Thoughts
- Frequently Asked Questions (FAQs)
What is Revenue Cycle Management (RCM)?
Revenue Cycle Management is the comprehensive financial process that healthcare organizations use to capture, manage, and collect payment for patient services. It covers every step from pre-registration and clinical documentation to coding, claims submission, payment posting, patient billing, collections, and reporting. RCM integrates clinical, administrative, and financial workflows while ensuring compliance, coding accuracy, and adherence to payer requirements.
In simpler terms, once clinical care is delivered, RCM ensures that the correct codes are applied and claims are submitted accurately and efficiently. It also ensures that payments are received efficiently, preventing the organization from losing any revenue it has earned.
Understanding RCM’s role highlights its importance in healthcare operations, so let’s explore the key benefits it provides to healthcare organizations.
How Revenue Cycle Management Benefits Healthcare Operations?
Effective RCM delivers measurable advantages that directly impact the financial health, operational performance, and compliance posture of healthcare organizations. By aligning clinical, administrative, and financial workflows, RCM ensures that revenue is captured accurately, claims are processed efficiently, and patient interactions remain seamless.
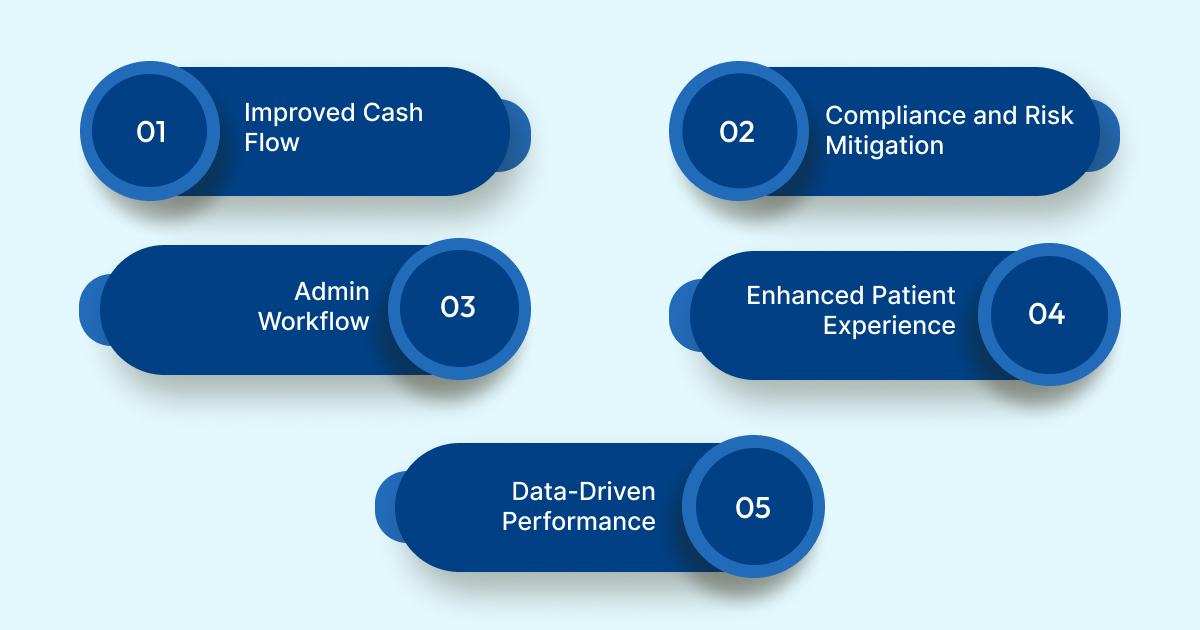
Below are a few key benefits of RCM:
- Improved Cash Flow and Financial Stability: By reducing claim denials, automating claim submissions, and ensuring accurate coding, organizations can shorten days in accounts receivable (A/R). This also helps increase net collection rates, securing a predictable and stable cash flow.
- Compliance and Risk Mitigation: Accurate ICD‑10 and CPT coding, along with complete clinical documentation, minimizes audit exposure and reduces payer penalties. It also ensures adherence to evolving regulatory requirements.
- Streamlined Administrative Workflow: Automated eligibility verification, claim scrubbing, and denial tracking reduce manual follow-ups and duplicate data entry. This allows staff to focus on complex coding exceptions and managing high-risk accounts.
- Enhanced Patient Experience: Efficient registration, transparent billing, and prompt resolution of payment inquiries all contribute to improved patient satisfaction scores. They also reduce billing disputes and strengthen trust in the organization.
- Data-Driven Performance: Real-time dashboards tracking denial trends, first-pass claim acceptance, and A/R aging enable leadership to implement targeted interventions. This helps optimize revenue cycle efficiency and identify areas for continuous improvement.
Also Read: 2025 Telehealth Updates: Key E/M Code Changes & Medicare Policies
By providing these tangible benefits, RCM elevates coding accuracy, operational control, and financial outcomes. With this context established, let’s now explore the ten crucial stages of the healthcare revenue cycle.
10 Key Stages of the Healthcare Revenue Management Cycle
The healthcare revenue cycle in the U.S. is a multi-step process that links clinical care, coding, and financial operations. Below is a practical breakdown of each stage of the revenue cycle, highlighting how medical coding interacts at every step. Understanding these stages helps healthcare professionals, coders, and revenue cycle managers see the direct connection between clinical documentation, coding accuracy, and financial performance.

1. Initial Patient Intake and Eligibility Check
Preliminary patient information is collected, and basic insurance coverage is verified to prepare accurate records for coding and billing.
Key Activities / Focus Areas:
- Patient Information Collection: Gather patient demographics, insurance details, and preliminary benefits information.
- Prior Authorization: Obtain necessary authorizations for services requiring payer approval.
- Coding Readiness: Ensure coders have accurate identifiers and coverage details to prevent errors that occur downstream.
2. Comprehensive Patient Enrollment
Complete demographic and insurance information is captured, including patient consent forms, to reduce administrative errors and support coding accuracy.
Key Activities / Focus Areas:
- Demographic Verification: Confirm date of birth, address, and contact information.
- Insurance Documentation: Record policy numbers, group numbers, and plan details accurately and precisely.
- Patient Consent: Obtain and store signed consent forms for regulatory compliance.
3. Payer Coverage Confirmation and Authorization
Detailed insurance coverage is confirmed, and pre-certifications are obtained to prevent claim rejections and support accurate coding.
Key Activities / Focus Areas:
- Coverage Verification: Check benefits, co-pays, deductibles, and network requirements.
- Authorization Management: Secure pre-certifications or prior authorizations for required procedures.
- Coordination with Coding Team: Communicate coverage details to ensure accurate claim submission.
4. Clinical Documentation Translation and Coding
Clinical services are reviewed and translated into CPT/HCPCS procedure codes, ICD-10-CM diagnosis codes, and necessary modifiers for compliance and accurate reimbursement.
Key Activities / Focus Areas:
- Documentation Review: Ensure all services and procedures are captured in the EHR.
- Procedure and Diagnosis Coding: Assign correct CPT/HCPCS and ICD-10-CM codes to ensure accurate reimbursement.
- Modifiers and Compliance: Apply modifiers and adhere to payer rules to maximize reimbursement and ensure compliance with regulations.
5. Claims Preparation and Electronic Filing
Coded services are organized into claims ready for electronic or paper submission, improving first-pass acceptance and reducing errors.
Key Activities / Focus Areas:
- Data Validation: Verify patient details, codes, and supporting documentation to ensure accuracy and completeness.
- Claim Assembly: Compile claims in standardized formats with all necessary documents.
- Submission Management: Transmit claims and confirm successful delivery.
- Error Resolution: Correct missing or inconsistent information before submission.
6. Claim Review and Denial Resolution
Denied or underpaid claims are analyzed to identify coding or documentation errors, and corrections are made to recover revenue efficiently and accurately.
Key Activities / Focus Areas:
- Denial Analysis: Identify root causes of rejected or underpaid claims.
- Claim Correction: Collaborate with coders and billing staff to fix errors.
- Resubmission and Appeals: Resubmit claims and manage appeals as required.
- Denial Trend Monitoring: Track patterns to prevent future denials.
7. Remittance Processing and Reconciliation
Payments from payers and patient responsibilities are posted and reconciled, ensuring accurate reimbursement for all services.
Key Activities / Focus Areas:
- Payment Posting: Record payer and patient payments accurately.
- Variance Identification: Spot underpayments, adjustments, or partial denials.
- Correction and Follow-Up: Resolve discrepancies with coders and billing staff to ensure accurate billing.
8. Patient Statement Generation and Billing
After payer processing, patient invoices for co-pays, deductibles, and coinsurance are generated accurately, minimizing disputes.
Key Activities / Focus Areas:
- Statement Preparation: Produce detailed and clear patient bills.
- Coding Verification: Confirm that billed services are accurately coded.
- Patient Communication: Explain charges transparently to reduce confusion and inquiries.
9. Outstanding Balance Follow-Up and Recovery
Unpaid patient balances and lingering accounts receivable are followed up systematically, with coding supporting verification of billed services.
Key Activities / Focus Areas:
- Balance Monitoring: Track unpaid accounts and initiate follow-up procedures to ensure timely payment.
- Documentation Support: Provide coded service details to substantiate patient responsibility and liability.
- Collections Coordination: Collaborate with collections teams to resolve disputes or arrange payment plans.
10. Revenue Cycle Performance Monitoring and Reporting
Key performance metrics are tracked and analyzed to optimize revenue cycle efficiency and drive continuous improvement.
Key Activities / Focus Areas:
- Metric Tracking: Monitor denial rates, days in A/R, net collection yield, and average reimbursement.
- Data Provisioning: Ensure coders provide accurate documentation for dashboards and reports to support data integrity.
- Performance Optimization: Utilize insights to implement targeted interventions and enhance workflows.
Implementing structured workflows, proactive denial management, and accurate coding practices ensures smoother claim submission and faster reimbursements. RapidClaims brings this blueprint to life with end-to-end healthcare revenue-cycle automation. It delivers a 98% clean-claim rate, 170% coder productivity lift, and 40% denial reduction, helping providers cut costs, recover revenue, and succeed in both FFS and VBC models.
Also Read: Healthcare Revenue Cycle Management Software and Services
Challenges in Healthcare RCM and How to Overcome Them
Healthcare revenue cycle management faces multiple hurdles that directly affect coding accuracy, reimbursement, and workflow efficiency. Here are five key challenges, along with best practices to address them:

1. Complex and Evolving Coding Requirements
Modern coding involves hundreds of thousands of ICD-10 codes, frequent CPT updates, modifiers, bundling rules, and surgical package logic. Even minor errors can trigger claim denials or audits.
Best Practices to Overcome:
- Implement continuous coding education and certification programs for staff.
- Maintain up-to-date code libraries and payer-specific guidelines.
- Use automated coding validation tools to flag inconsistencies before claim submission.
2. Payer-Specific Variability
Commercial payers, Medicare, and Medicaid have distinct rules for claims submission, pre-authorizations, modifiers, and denials. Navigating this heterogeneity increases complexity and risk of errors.
Best Practices to Overcome:
- Develop standardized payer profiles detailing submission rules, pre-certification requirements, and common denial triggers.
- Train coders and billing staff on payer-specific workflows to ensure accurate and efficient billing.
- Utilize clearinghouse solutions with payer rule logic to automate submissions.
3. Denials and Rework Burden
Denials often originate from upstream issues such as registration, eligibility verification, or coding mistakes. Reprocessing denials consumes resources, delays revenue, and reduces net collection yield.
Best Practices to Overcome:
- Implement proactive denial prevention through pre-submission claim scrubbing and automated eligibility verification to ensure accurate claims processing.
- Track denial patterns to address root causes with coders, billing, and registration teams.
- Establish clear workflows for timely appeal and resubmission.
4. Staff Turnover and Skill Gaps
Revenue cycle and coding teams face high turnover, resulting in knowledge gaps, slower claim processing, and an increased risk of errors.
Best Practices to Overcome:
- Invest in structured onboarding and continuous training programs.
- Cross-train staff to handle multiple stages of the revenue cycle.
- Utilize automation tools to reduce reliance on manual processes for repetitive tasks.
5. Balancing Technology, Analytics, and Patient Experience
Legacy EHRs, billing systems, and analytics tools often fail to integrate smoothly, resulting in bottlenecks. Simultaneously, patient financial responsibility is increasing, making billing clarity and transparency critical.
Best Practices to Overcome:
- Adopt integrated revenue cycle management platforms that connect EHR, coding, billing, and analytics.
- Implement dashboards to monitor claim status, denial trends, and accounts receivable (A/R) performance in real-time.
- Design patient-friendly billing statements and communication protocols to improve transparency and reduce disputes.
Also Read: Top Vendors for Revenue Cycle Management in Healthcare
Now, let’s examine how to determine if your revenue cycle management is performing at its best by looking at the key metrics and benchmarks that drive efficiency.
How to Evaluate Whether Your RCM Is Truly Effective?
Data is essential for understanding the effectiveness of your RCM, whether you handle it internally or work with an external RCM partner. By examining key financial and performance metrics, you can identify areas where your RCM is succeeding and pinpoint opportunities for improvement.
Some critical benchmarks to monitor include:
- Point-of-Service (POS) Cash Collections: Tracks co-payment collections at the time of service. Since contracts with payers bind healthcare providers, monitoring this revenue ensures contract compliance and highlights collection efficiency.
- Bad Debt: Reflects amounts unlikely to be recovered. Tracking bad debt helps assess the effectiveness of your collections processes and highlights areas for improvement.
- Days in Accounts Receivable (A/R): Measures how long it takes to collect payments for invoices. A lower number indicates a faster revenue cycle and stronger financial health.
- Days in Total Discharged Not Billed (DNB): Captures the time between patient discharge and billing. Monitoring this helps ensure timely invoicing and reduces delays in revenue recognition.
- Clean Claim Rate: Evaluates the accuracy of submitted claims. High clean claim rates reduce denials, streamline collections, and enable proactive error resolution.
By regularly tracking these metrics, healthcare teams can gain actionable insights, enhance financial performance, and ensure compliance throughout the revenue cycle. Next, let’s explore the key technology solutions that help healthcare organizations streamline RCM processes.
Key Technology Solutions for Optimizing Revenue Cycle Management
Technology forms the backbone of modern revenue cycle management, enabling healthcare organizations to seamlessly link clinical documentation, coding, billing, and payment processes. By utilizing the right tools, RCM teams can reduce errors, accelerate reimbursements, and maintain compliance across the complex U.S. payer system.
- Electronic Health Records (EHRs): Capture detailed clinical documentation to support accurate coding, claims submission, and regulatory compliance. Enables audits and reduces claim rejections due to missing or incomplete information.
- Automated Eligibility Verification: Checks patient insurance and prior authorization in real time during registration. Minimizes coverage errors and improves first-pass claim acceptance.
- Medical Coding and Claims Management Software: Integrated platforms apply coding rules, modifiers, and payer-specific logic to ensure accurate claims processing. Streamlines claim preparation, reduces errors, and enhances workflow visibility.
- Denial Management and Analytics Tools: Use automation and AI to identify high-risk claims and track denials post-submission. Supports root-cause analysis and prevents recurring revenue losses.
- Patient Billing and Engagement Platforms: Digital portals enable patients to view statements, make secure payments, and understand their charges. Improves collections, transparency, and patient trust.
Adopt platforms like RapidClaims, explicitly built for healthcare revenue cycle needs. With SMART-on-FHIR integration and continuous payer-driven learning, RapidClaims ensures compliance while scaling automation. Its modules deliver measurable results: 96% audited coding accuracy with RapidCode, 25% RAF accuracy improvement with RapidCDI, and 70% fewer claim denials with RapidScrub. These outcomes strengthen audit readiness, protect margins, and reduce repetitive documentation burdens.
Final Thoughts
Effective Revenue Cycle Management in medical coding is critical for ensuring accurate claims, timely reimbursements, and regulatory compliance. Structured workflows, precise coding, and proactive denial management help healthcare organizations efficiently maximize revenue, minimize errors, and enhance patient satisfaction.
Healthcare organizations can achieve these benefits with RapidClaims. Its AI-powered solutions streamline coding, audits, and revenue cycle processes, ensuring faster claim processing, higher accuracy, and compliance readiness. With secure, auditable workflows, RapidClaims enables organizations to manage challenging processes with confidence.
Take the next step in optimizing your healthcare revenue cycle. Request a Free Demo and see how RapidClaims’ AI-powered RPA can transform your healthcare operations and make your team more efficient, accurate, and audit-ready.
Frequently Asked Questions (FAQs)
1. How does medical coding accuracy directly impact revenue cycle performance?
A. Accurate coding ensures claims are submitted correctly with the right CPT, ICD-10, and HCPCS codes. This reduces denials, accelerates payment posting, and improves net collection yield. Even minor coding errors can delay reimbursements or trigger audits, making precision crucial for both financial and operational efficiency.
2. What role does automation play in reducing denial rates?
A. Automation tools like claim scrubbing, eligibility verification, and AI-powered pre-submission checks identify errors before claims reach payers. This proactive approach minimizes first-pass denials, reduces rework, and frees coders to focus on complex cases, improving overall revenue cycle efficiency.
3. How can healthcare organizations balance patient experience with complex RCM workflows?
A. Clear billing statements, patient portals, and transparent communication are key. By integrating patient engagement platforms with coding and billing systems, organizations can maintain accuracy and compliance while ensuring patients understand charges, reducing disputes, and increasing satisfaction.
4. Why is real-time analytics important in RCM?
A. Dashboards tracking denial trends, days in A/R, and claim acceptance rates allow leadership to identify bottlenecks, optimize workflows, and implement targeted interventions. Real-time insights enable proactive decision-making, improving both financial performance and compliance readiness.
5. How can staff turnover impact revenue cycle efficiency, and what mitigates it?
A. High turnover leads to knowledge gaps and slower claim processing, increasing the risk of errors. Mitigation strategies include structured onboarding, continuous training, cross-training, and automation of repetitive tasks to maintain workflow continuity and coding accuracy despite staffing changes.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








