How to Use ICD-10 Codes for Altered Mental Status Diagnosis Without Risking Denials

Altered mental status is a term that shows up frequently in inpatient and emergency documentation. But for healthcare organizations, it can be a costly blind spot. Clinical teams may use it to describe symptoms like confusion or unresponsiveness, but for those managing revenue integrity, this phrase is often the start of a bigger problem.
Without a clearly documented cause or diagnostic workup, altered mental status becomes a vague, non-specific entry in the chart. This forces coders to rely on fallback options like R41.82, which may be billable but rarely defensible. Over time, patterns like this put pressure on compliance metrics, trigger payer audits, and delay reimbursements.
For revenue cycle and compliance teams, the question isn’t whether AMS was present; it’s whether the documentation justifies how it’s coded. Getting this right means fewer rework loops, fewer denials, and fewer red flags in your claims data.
Key Takeaways
- R41.82 should only be used when no other diagnosis is documented
- Vague terms like “confused” or “AMS” need more context to be billable
- Specific codes like G93.41 or F05 reduce denials and audit flags
- Coders must link clinical findings to a defensible code
- Solutions like RapidClaims help surface better code options faster
What Is ICD-10 and Why It Matters for Coding Altered Mental Status
ICD-10, or the International Classification of Diseases, Tenth Revision, is the standardized coding system used by healthcare organizations to classify symptoms, diagnoses, and procedures. It acts as a universal language between clinical teams, billing departments, payers, and regulators. But when it comes to altered mental status, its utility depends entirely on how well the clinical documentation supports coding decisions.
Altered mental status may show up in a provider’s note as confusion, lethargy, or cognitive decline. But insurers will not process these vague descriptors unless they are clearly connected to an underlying medical condition or workup. ICD-10 codes are how billing teams translate a narrative chart into a claim, but symptom-only language leaves too much open to interpretation.
Here is why ICD-10 accuracy matters:
- It ensures the symptom is clearly linked to an underlying cause or diagnosis
- It prevents overuse of non-specific codes like R41.82 that invite payer denials
- It helps revenue cycle teams maintain compliance and improve first-pass acceptance rates
- It enables HIM and CDI teams to identify documentation gaps earlier in the workflow
- It protects against audit triggers caused by inconsistent or unsupported coding
For healthcare organizations, using ICD-10 correctly is not just about coding skills. It is about building a defensible reimbursement process where billing accuracy aligns with clinical care.
How Documentation Gaps Complicate Coding for Altered Mental Status
Even the best coders can only work with what’s written in the chart. When providers use phrases like “confused” or “not responding appropriately” without context, the resulting claim lacks the specificity needed for clean billing.
Here’s what often goes missing in documentation:
- No mention of diagnostic workup (labs, imaging, neurological consultation, etc.)
- No linkage between the symptom and possible causes (like infection, medication, trauma)
- No clarification on whether the condition was transient, progressive, or resolved
- Missing terms like delirium, encephalopathy, psychosis, or disorientation, even when clinically relevant
These omissions don’t just frustrate coding teams. They increase the risk of:
- Defaulting to R41.82, which invites medical necessity denials
- Missed query opportunities that would strengthen claims
- Documentation-related delays that slow down reimbursement cycles
To code an altered mental status correctly, providers need to do more than describe what they observed. They need to tell the clinical story; what was suspected, tested, ruled out, and diagnosed. Without that, coders and auditors are left filling in the blanks and that’s exactly what payers look for in a denial.
ICD-10 Code Selection for Altered Mental Status Diagnosis
Not all cases of altered mental status are clinically or financially equal. The right ICD-10 code depends on whether documentation supports a root cause, not just a symptom. Below are commonly used ICD-10 codes, how they differ, and what documentation signals to look for. This is designed to help CDI and coding teams strengthen claim defensibility from the outset.
R41.82: Altered Mental Status, Unspecified
Use only when no cause has been identified and all diagnostics are still in progress or inconclusive. Make sure no other diagnosis is documented in the final impression. This code is highly scrutinized, especially when overused across encounters. Frequent usage signals weak clinical correlation and invites payers to question medical necessity.
G93.41: Metabolic Encephalopathy
Assign when documentation shows mental status changes tied to confirmed metabolic causes such as hepatic encephalopathy, uremia, or severe hyponatremia. Look for lab values, clinical notes, and consults that support the diagnosis and link it explicitly to the altered cognition.
F05: Delirium Due to Known Physiological Condition
Use when the provider clearly documents delirium as caused by an infection, medication reaction, or systemic issue. The chart must describe fluctuating consciousness and disorientation, and indicate that the condition is expected to resolve.
R41.0: Disorientation
Appropriate when the patient exhibits confusion or disorientation but does not meet the clinical criteria for delirium or encephalopathy. Use only if no underlying cause is documented and higher specificity codes do not apply.
G93.40: Encephalopathy, Unspecified
Use when encephalopathy is diagnosed but the type is not further clarified in the documentation. This should not be a fallback. Confirm that the provider has used the term encephalopathy in the impression, even if the subtype is missing.
F44.89: Other Dissociative and Conversion Disorders
Consider this code when mental status changes are tied to psychological or behavioral causes. Documentation should refer to dissociation, non-organic reactions, or behavioral unresponsiveness with no medical origin.
F06.0: Psychotic Disorder with Hallucinations Due to Known Medical Condition
Use when hallucinations or psychosis are documented as stemming from a diagnosed medical condition such as a neurologic or endocrine disorder. There should be a clear link between the medical condition and the mental status change.
For coders and CDI professionals, choosing the right code means reviewing more than the final diagnosis. It involves looking at labs, imaging, consults, progress notes, and discharge summaries to ensure the clinical picture supports the selected ICD-10.
When to Use ICD-10 Code R41.82 for Altered Mental Status
R41.82 is a valid ICD-10 code used to capture altered mental status when no definitive diagnosis has been established. However, it should be applied only when all reasonable workups are either inconclusive or still pending and when there is no clinical evidence to support a more specific diagnosis like delirium, encephalopathy, or psychosis.
For healthcare organizations, relying too often on R41.82 is not just a documentation issue. It becomes a revenue risk. This code often lacks the specificity that payers require, leading to denials, delays, and compliance concerns.
R41.82 may be appropriate in the following scenarios:
- The provider documents altered mental status or a similar observation but does not link it to a specific cause
- The diagnostic evaluation is underway or completed without yielding a conclusive diagnosis
- There are no findings to support related codes, such as metabolic encephalopathy or delirium
- The episode is clearly documented but labeled as non-specific by the provider
Still, its use should trigger internal scrutiny. Not because it is wrong, but because it often signals a missed opportunity for clarification or improvement in provider documentation. By surfacing vague chart entries early in the workflow, solution like RapidClaims enables CDI teams to intervene before claims are submitted. This prevents unnecessary reliance on default codes and ensures the clinical narrative is complete. It also protects the organization from compliance flags and poor denial trends.
If your claims data shows a consistent pattern of R41.82 usage, it may be time to review how altered mental status is being documented and flagged across departments. RapidClaims makes it easier to catch these patterns before they affect reimbursements.
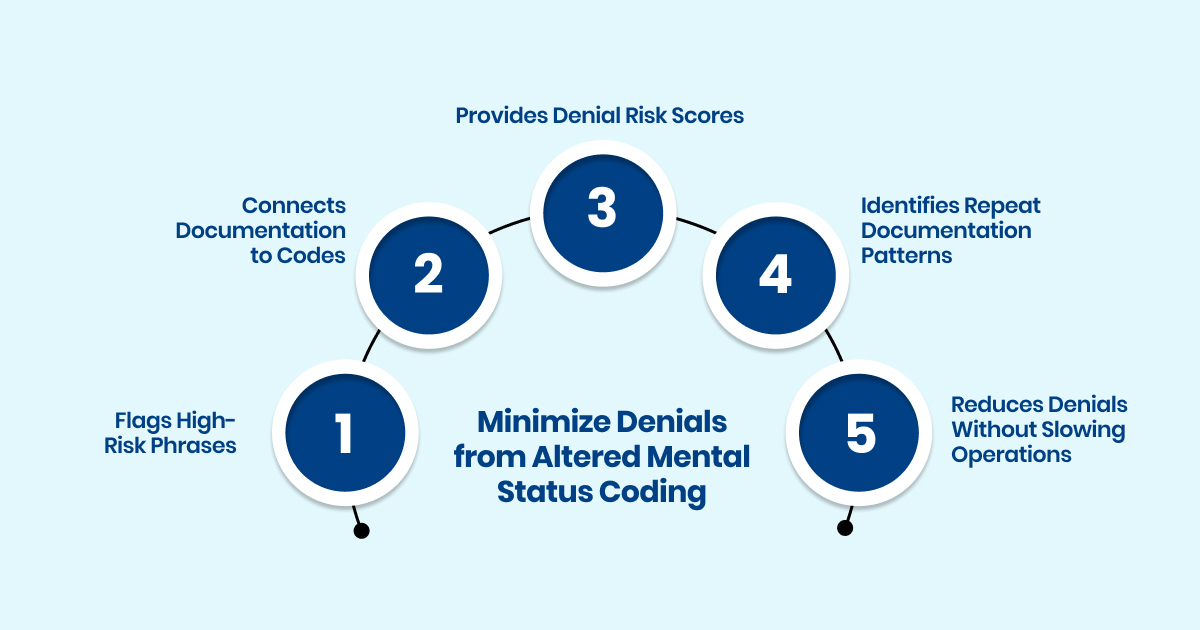
How RapidClaims Helps Minimize Denials from Altered Mental Status Coding
When altered mental status is documented vaguely, it becomes more than a clinical issue. It directly affects the claim. Incomplete documentation forces coders to assign non-specific ICD-10 codes like R41.82, which can pass basic validation but often trigger denials during medical necessity review. The real cost shows up later in claim edits, audit flags, delayed reimbursements, and extra hours lost in rework.
RapidClaims helps healthcare organizations close this gap.
Detects High Risk Phrases That Can Cause Revenue Loss
Terms like “confused,” “lethargic,” or “AMS” without supporting detail can go unnoticed in busy clinical workflows. RapidClaims flags these vague terms at the prebill stage and alerts teams when documentation is missing key clinical elements like diagnostics, clinical impression, or causality. This proactive flagging prevents problematic claims from leaving the door in the first place.
Connects Documentation to Code Selection Automatically
RapidClaims does not just identify weak documentation. It maps it to potential coding mismatches. For example, if altered mental status is documented but there is no evidence of delirium, encephalopathy, or disorientation, the platform surfaces this disconnect. It gives CDI and coding teams the opportunity to initiate timely queries and update records before submission.
Provides Denial Risk Scores Based on AMS Patterns
Using machine learning trained on real world claims data, RapidClaims can score the likelihood of a denial based on how altered mental status is documented and coded. This gives compliance teams better visibility into documentation risk, allowing them to prioritize high impact queries and make audit readiness part of the daily workflow.
Surfaces Repeat Documentation Patterns Across Facilities and Providers
If a provider or department regularly uses AMS related terminology without clear diagnostic support, RapidClaims identifies those trends across charts and timeframes. This makes it easier for HIM and education teams to intervene early, provide targeted training, and reduce reliance on low specificity codes like R41.82.
Reduces Avoidable Denials Without Slowing Down Operations
The goal is not to slow documentation or overload providers with education. RapidClaims works in the background of the revenue cycle, surfacing only high risk documentation that is likely to result in denials. This streamlines collaboration between CDI, coding, and compliance teams without introducing unnecessary friction into clinical workflows.
Final Thoughts
Altered mental status may begin as a vague symptom, but by the time it reaches your coding team, it becomes a critical decision point. Do you assign R41.82 by default, or pause to see if the documentation supports a more specific diagnosis?
That decision impacts more than reimbursement. It shapes compliance reporting, payer audit outcomes, and the accuracy of your hospital’s clinical data. Accepting vague terms like “AMS” or “confused” without clarification leads to repeat denials, delayed payments, and lost revenue across dozens or even hundreds of charts.
This is not just about fixing occasional documentation errors. It is about identifying risk patterns before they grow into costly trends. Repeated use of ambiguous codes weakens defensibility and puts your revenue cycle at risk.
That is where solution like RapidClaims come in. They go beyond code suggestions. By surfacing documentation gaps, highlighting red flags, and prompting query opportunities, they help your team code with confidence and speed. The result is cleaner claims, better compliance, and reduced denial risk without adding to your team’s workload.
Want to see how it works in your environment? [Request a demo today.]
Frequently Asked Questions
Q: What is the ICD-10 code R41.82?
A: R41.82 stands for Altered Mental Status, Unspecified. It is used when symptoms like confusion or disorientation are present, but no specific cause has been documented. Although it is technically billable, it often leads to denials because it lacks clinical clarity and justification.
Q: When is it appropriate to use R41.82?
A: Only when diagnostic workups have been performed and no definitive cause has been found or documented. If the chart includes no confirmed diagnosis and nothing suggests a condition like delirium, encephalopathy, or psychosis, this code may be necessary as a last resort. It should never be used without first exhausting all other documentation opportunities.
Q: Why does overusing R41.82 cause reimbursement issues?
A: Frequent use of R41.82 indicates a pattern of vague documentation. Payers see it as a red flag for unsupported claims. It does not clearly establish medical necessity, and over time, it increases the risk of denials, audit reviews, and compliance setbacks.
Q: How can revenue cycle leaders prevent this coding risk?
A: The key is early intervention. By flagging vague terms like AMS or confusion in real time, teams can ask for clarification while the patient is still under care. This makes it easier to avoid fallback codes and build stronger claims before they hit billing.
Q: Is this mainly a coder’s problem?
A: It is a shared responsibility. Coders may assign the code, but systemic gaps in provider documentation are what drive the overuse. This is where compliance leaders, HIM, and CDI teams must step in to address patterns and create guardrails against unsupported entries.
Q: How does AMS coding influence audit exposure?
A: When claims contain non-specific codes like R41.82 without supporting documentation, it signals to payers that documentation standards are weak. If this code appears repeatedly across encounters, it could result in audit targeting and retroactive claim reviews.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






