Prior Authorization AI That Cuts Delays, Denials, and Admin Burden

Prior authorization (PA) was designed to ensure clinically appropriate care, yet it has become one of the most persistent operational bottlenecks in healthcare. Even as organizations strengthen their revenue cycle infrastructure, PA continues to slow care delivery and add significant administrative overhead. According to the 2024 American Medical Association (AMA) nationwide physician survey, 93% of physicians say prior authorization delays necessary care, and 29% report that PA has resulted in a serious adverse event for a patient. These delays do not only affect clinical workflows. They cascade into scheduling disruptions, billing delays, repeated submissions, and higher denial rates across the revenue cycle.
As clinical volumes rise and payer criteria grow more complex, health systems are increasingly evaluating AI-driven approaches to reduce manual effort and accelerate authorization times. But to understand where AI can have a meaningful impact, it is essential to examine why the traditional prior authorization process continues to break down.
Key Takeaways
- PA delays are widespread; 93% of physicians report slowed care and higher denial risk.
- Fragmented EHR data makes medical-necessity evidence difficult to gather.
- Rapidly changing payer rules lead to outdated submissions and preventable denials.
- Fax and portal-based workflows slow turnaround and require heavy manual follow-up.
- Rising PA volumes exceed staffing capacity, creating persistent bottlenecks.
- Manual workflows lack visibility into workload, payer patterns, and operational risk.
- AI structures clinical evidence and aligns it with payer-specific criteria.
- AI identifies documentation gaps early, reducing pends and rework.
- AI consolidates submission paths into a single, streamlined workflow.
- Human oversight still matters; AI accelerates routine cases and flags complex ones.
- Effective adoption requires strong data quality, policy governance, and clear escalation protocols.
- Health systems see faster decisions, fewer pends, and more predictable scheduling.
- High-impact areas include imaging, orthopedics, cardiology, behavioral health, specialty meds, and rehab.
- Tools like RapidClaims enhances upstream PA readiness by improving documentation completeness and coding accuracy.
Table of Contents:
- Why Prior Authorization Delays Persist in Today’s Healthcare System
- The Hidden Operational Cost of Manual Prior Authorization
- How AI Improves Prior Authorization Accuracy and Turnaround Time
- Key Requirements for Implementing AI in Prior Authorization Workflows
- Benefits of Using AI for Prior Authorization in Health Systems
- Risks and Oversight Considerations When Applying AI to Prior Authorization
- High-Impact Use Cases for Prior Authorization AI Across Care Settings
- How RapidClaims Strengthens Documentation and Coding for Prior Authorization AI
- Conclusion
- FAQs
Why Prior Authorization Delays Persist in Today’s Healthcare System
Despite years of process improvement, prior authorization remains manual, fragmented, and highly inconsistent across payers. Several operational factors continue to slow decisions and create downstream revenue impact.
1. Documentation Gaps in the EHR
Most delays start before submission. Relevant clinical details such as treatment history, diagnostics, or comorbidities are often buried in lengthy notes, scanned documents, or unstructured text.
As a result, PA teams spend significant time:
- Searching through charts
- Extracting medical-necessity evidence
- Reformatting information for payer forms
- Risking omissions that lead to pends or denials
Specialties with complex criteria, such as imaging, orthopedics, behavioral health, and cardiology, feel this burden most.
2. Payer Rules That Change Faster Than Workflows
Payers frequently update clinical criteria and submission requirements. With variations across plan types and service lines, staff often face:
- Outdated criteria applied to new cases
- Incorrect portal routing
- Missing documents tied to recent rule changes
- More back-and-forth with payers
These mismatches drive many avoidable denials seen later in the RCM workflow.
3. Legacy Submission Channels That Slow Cycle Time
Even as API pathways expand, many authorizations still rely on fax, uploads, or phone reviews. These channels create unpredictable turnaround times and force staff to:
- Manually check status
- Re-enter data
- Call payers for updates
This consumes hours and disrupts scheduling predictability.
4. Staffing Constraints and Rising Case Volume
PA volume continues to grow due to higher utilization, new service lines, expanding specialty care, and more complex criteria. With fixed staffing levels, teams face an imbalance that produces backlogs and slows both care delivery and revenue movement.
5. Downstream Impact on Revenue Cycle Metrics
Authorization problems extend well beyond access operations, contributing to:
- Delayed scheduling
- Charge lags
- Denials tied to missing or incorrect PA data
- Additional rework for billing and coding
- Higher days in A/R and inconsistent cash flow
Strong PA quality is foundational to first-pass claim acceptance and overall RCM performance.
If your PA or access teams face recurring delays or payer pends, RapidClaims can analyze sample encounters to pinpoint documentation and coding gaps that slow authorizations.
The Hidden Operational Cost of Manual Prior Authorization
Even when the steps of prior authorization are well understood, the broader organizational impact is often underestimated. Beyond slow turnaround times, manual PA introduces structural inefficiencies that affect staffing models, technology investment, payer relationships, and long-term financial performance.
Key operational challenges include:
- Fragmented technology infrastructure: Many access centers rely on a mix of EHR modules, shared inboxes, payer portals, spreadsheets, and email chains. This causes inconsistent documentation trails, limited visibility into case status, and no reliable way to quantify true PA workload.
- Limited scalability of human-dependent workflows: Adding new specialties, opening new service lines, or increasing procedure volume requires proportional staffing increases. Most organizations cannot scale hiring at the same pace as utilization growth, creating persistent throughput constraints.
- Inadequate visibility into payer performance: Without centralized data, teams cannot track payer-specific turnaround times, approval rates, or error patterns. This makes it difficult to identify which payers drive the most rework, negotiate operational improvements, or target education for clinical departments.
- Disruption to downstream scheduling and capacity planning: When authorization timing varies unpredictably, OR blocks, imaging slots, infusion appointments, and consult availability cannot be forecast reliably. This leads to unused capacity, last-minute reshuffling, and preventable patient cancellations.
- Increased pressure on clinical staff: Nurses, physicians, and advanced practice providers are often pulled into PA clarification, peer-to-peer reviews, or documentation correction. This reduces available clinical time and contributes to burnout, especially in high-intensity service lines.
- Inability to accurately model financial risk: Manual processes prevent leaders from projecting authorization bottlenecks or forecasting the revenue at risk due to pending or potentially denied cases. This blinds finance, RCM, and operations teams to upcoming volume constraints or cash flow dips.
How AI Improves Prior Authorization Accuracy and Turnaround Time
AI for prior authorization is most effective when it strengthens the accuracy, structure, and completeness of data used to determine medical necessity. The focus is not full automation, but creating cleaner, decision-ready requests with fewer manual touchpoints.

Core operational functions include:
- Identifying the exact clinical elements payers require: The AI pinpoints authorization-relevant details such as prior treatment timelines, diagnostic thresholds, contraindications, and service-specific metrics that staff would otherwise retrieve manually.
- Detecting documentation gaps early in the workflow: Before a request moves forward, the system flags missing clinical evidence, mismatched codes, or incomplete supporting notes. This prevents unnecessary pends and reduces back-and-forth with payers.
- Standardizing the structure of authorization submissions: Instead of relying on variable human formatting, AI generates consistent evidence summaries and attaches the appropriate encounters. This reduces variation across teams and minimizes subjective interpretation.
- Integrating submission channels into a single workflow: The AI pushes requests through the appropriate channel, whether it is a payer API, a portal, or a legacy method. This centralizes tracking and eliminates the need for staff to navigate multiple systems.
- Routing requests based on risk and completeness: Routine, criteria-aligned cases move forward with minimal intervention, while high-risk or incomplete cases are automatically directed to the appropriate specialist queue. This protects compliance and prevents costly errors.
Key Requirements for Implementing AI in Prior Authorization Workflows
Successful adoption of AI-driven prior authorization depends on how well the technology aligns with existing infrastructure, staffing models, and compliance expectations. Health systems should evaluate several operational factors before deployment.
Key considerations include:
- EHR integration and data availability: The AI must pull directly from encounter notes, order details, problem lists, imaging impressions, and structured fields. Limited access to clinical data reduces accuracy and increases exceptions routed to staff.
- Payer policy management and version control: Health systems need a process to validate that the AI uses up-to-date payer criteria. This includes version tracking, rule updates, and alignment with plan-level variations that influence authorization decisions.
- Workflow design across access, clinical, and RCM teams: The introduction of AI changes handoffs, queue management, and case prioritization. Leaders should define which request types the AI handles end-to-end and which require clinical review to avoid bottlenecks.
- Staff readiness and exception-handling protocols: PA teams need clear guidance on how to validate AI-generated packets, manage flagged inconsistencies, and handle complex cases. Without defined escalation pathways, workloads can shift unevenly.
- Compliance, auditability, and documentation retention: Every AI-generated action must be traceable, including evidence sources, decision logic applied, and user overrides. This is essential for internal audits and responding to payer inquiries or medical-necessity reviews.
- Performance monitoring and measurable KPIs: Health systems should track metrics such as request turnaround time, pend rates, first-pass approval rates, and rework volume. This ensures the AI’s impact is visible and tied to operational and financial outcomes.
Benefits of Using AI for Prior Authorization in Health Systems
AI-driven prior authorization strengthens operational performance by improving submission quality, reducing manual workload, and stabilizing downstream revenue. The benefits extend beyond faster approvals and influence multiple components of the access and revenue cycle.
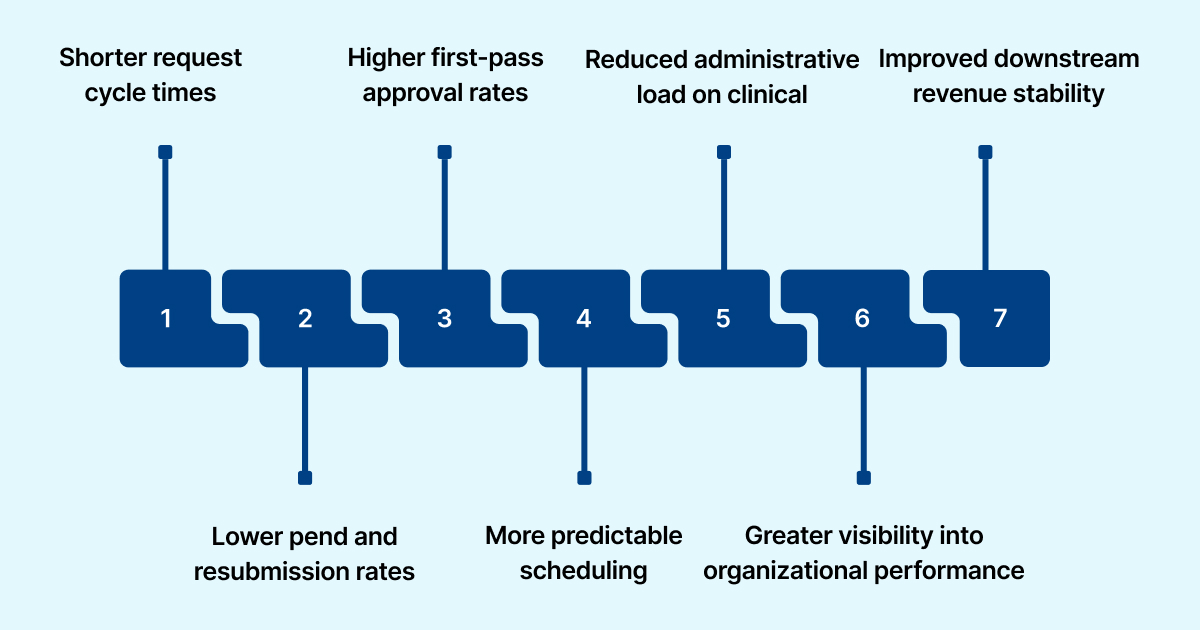
Key benefits include:
- Shorter request cycle times: AI reduces the time spent gathering clinical evidence and formatting submissions, allowing teams to process routine cases more quickly and free capacity for complex reviews.
- Lower pend and resubmission rates: By validating documentation before submission, AI reduces incomplete or inconsistent packets, which translates into fewer payer requests for additional information.
- Higher first-pass approval rates: When required clinical elements are consistently captured and aligned to policy, payers receive cleaner requests, improving approval accuracy across high-volume service lines.
- More predictable scheduling and capacity management: Faster, more reliable authorization decisions allow clinics, imaging centers, and surgical departments to schedule with greater confidence and reduce last-minute cancellations.
- Reduced administrative load on clinical and access teams: Staff spend less time on repetitive tasks such as chart mining, manual uploads, and portal navigation, enabling them to focus on complex cases, patient coordination, or payer communication.
- Greater visibility into organizational performance: AI centralizes request data, allowing leaders to monitor volumes, turnaround times, payer behavior, and service-line trends. This supports operational planning and payer strategy discussions.
- Improved downstream revenue stability: Cleaner authorizations reduce delays in charge capture and minimize denials tied to missing or invalid PA numbers, improving cash flow consistency and overall RCM performance.
Risks and Oversight Considerations When Applying AI to Prior Authorization
While AI can improve authorization accuracy and throughput, health systems must evaluate how the technology behaves within clinical, operational, and regulatory environments. Effective oversight ensures AI accelerates workflows without creating new compliance or quality issues.
Key risks and considerations include:
- Inconsistent outputs without defined governance: If payer criteria or clinical documentation patterns change, AI recommendations may diverge from current requirements. Organizations need structured governance to review rule updates, monitor model performance, and validate outputs.
- Over-automation of borderline cases: Not all requests are appropriate for automated processing. High-cost procedures, multi-step medical-necessity pathways, and complex clinical histories require human review to avoid inappropriate submissions or avoidable denials.
- Limited transparency for clinical or compliance teams: AI systems must allow staff to see what data was extracted, how criteria were applied, and why a request was routed a certain way. Without clear reasoning, staff cannot validate the accuracy of packets or respond to payer inquiries.
- Operational disruption during rollout: Shifting from manual workflows to AI-assisted processes can temporarily increase workload if staff do not understand new routing rules, exception queues, or review thresholds. Defined training plans and phased adoption help stabilize transitions.
- Data quality issues impacting AI accuracy: Missing encounter details, inconsistent provider documentation, or incomplete coding can reduce the reliability of AI outputs. Strong documentation practices remain essential to ensure accurate extractions and alignments.
- Regulatory expectations for audit trails: Payors and auditors may request evidence of how clinical criteria were met. AI systems must preserve detailed logs, including source documents and decision logic, to support compliance reviews and clinical justification.
High-Impact Use Cases for Prior Authorization AI Across Care Settings
AI-driven prior authorization delivers the strongest operational lift in areas where clinical criteria are complex, documentation volume is high, and payer scrutiny is consistent. These service lines often experience the heaviest administrative burden and the greatest scheduling volatility.
High-value use cases include:
- Advanced imaging (MRI, CT, PET): Imaging requests often require detailed clinical evidence such as prior treatments, symptom duration, comparative findings, and functional limitations. AI reduces the time technologists and schedulers spend assembling this information and helps prevent incomplete evidence submissions that delay scans.
- Orthopedics and spine procedures: These services rely on multi-step criteria that reference therapy trials, specific diagnostic findings, and symptom progression. AI helps standardize evidence preparation so requests across different surgeons and clinics meet the same documentation threshold.
- Cardiology and electrophysiology: Device implants, stress tests, and advanced diagnostics require precise clinical markers such as ejection fraction values, arrhythmia burden, or medication response. AI extracts these data points directly from notes and imaging reports, reducing manual validation tasks.
- Behavioral health and psychiatry: Behavioral health authorizations frequently require longitudinal documentation such as treatment history, medication changes, and functional assessments. AI organizes these records into structured summaries that expedite review and reduce rework.
- Specialty medications and infusion therapies: For specialty drugs, payers expect step-therapy verification, biochemical markers, and documented contraindications. AI helps pharmacy teams compile evidence faster and reduces delays that affect infusion scheduling.
- Post-acute and rehabilitation services: These requests require coordination across multiple care teams and transitions. AI brings together functional assessments, therapy progress notes, and clinical justifications that would otherwise require staff to review multiple encounters.
How RapidClaims Strengthens Documentation and Coding for Prior Authorization AI
RapidClaims is not a standalone prior authorization platform, but its AI infrastructure strengthens the upstream processes that determine whether an authorization is approved, delayed, or denied. By improving documentation accuracy and coding integrity, RapidClaims ensures every PA request begins with clean, complete, and policy-aligned clinical data.
How RapidClaims enhances PA workflows:
- Improves documentation completeness before PA preparation: RapidClaims extracts clinically relevant details from unstructured EHR notes and aligns them with diagnoses, procedures, and documented clinical factors. This gives PA teams a more complete starting point and reduces time spent gathering evidence.
- Strengthens coding accuracy that supports medical-necessity alignment: Authorization approvals often depend on correct ICD-10-CM, CPT, or HCC coding tied to the documented condition. RapidClaims’ AI validates coding accuracy so the PA request reflects the true clinical picture, reducing downstream conflicts with payer criteria.
- Identifies documentation gaps that may stall PA decisions: RapidClaims flags missing clinical elements, inconsistent problem lists, or incomplete episode histories. PA staff receive clearer insight into what may be questioned by a payer, allowing corrections before the request is submitted.
- Supports cleaner handoffs between clinical, access, and RCM teams: With standardized documentation and structured data, RapidClaims reduces variation between departments. This helps ensure PA packets, order entries, and claims all align, minimizing rework later in the revenue cycle.
- Provides audit-ready information for payer follow-ups: When payers request clarification, RapidClaims helps teams quickly retrieve the relevant encounters, clinical details, and coded information used in the original request. This shortens response time and supports compliance.
- Exploring AI to improve authorization accuracy, reduce rework, or stabilize scheduling? Request a personalized RapidClaims demo to see how stronger documentation and coding improve PA outcomes.
Conclusion
Prior authorization remains a major source of operational friction for health systems, especially as clinical complexity and payer requirements grow. AI helps reduce delays by creating more complete, consistent, and decision-ready requests, allowing teams to move cases forward with fewer touchpoints and less uncertainty. When organizations adopt technologies that standardize evidence and streamline workflows, authorization becomes more predictable, scheduling stabilizes, and downstream revenue performance improves.
If you are exploring AI-enabled improvements to documentation and RCM workflows, request a demo of RapidClaims to see how it fits within your organization’s operational strategy.
FAQs
Q: What is prior authorization AI and how does it differ from traditional prior authorization?
A: Prior authorization AI uses machine learning and NLP to extract clinical data, map it against payer-specific criteria, and generate structured authorization requests; replacing much of the manual chart review, data entry, and form-filling typical of traditional PA. It aims to reduce staff workload, speed up approvals, and lower error rates.
Q: How much faster can authorizations be with AI compared to manual PA?
A: While speed gains vary by organization, recent studies show that AI-driven PA can significantly reduce the time required for authorization, especially for imaging, diagnostics, and medication approvals; transforming what might take days or hours of manual work into processed, payer-ready requests in a fraction of that time.
Q: Can AI for prior authorization reduce denials or pended requests?
A: Yes; by validating clinical evidence against payer criteria before submission, AI helps ensure completeness and compliance, reducing the risk of missing documentation, incorrect coding or form errors, which are common causes of denials or pends under manual PA workflows.
Q: Will implementing prior authorization AI replace my PA team or staff?
A: Not necessarily. For many use cases, AI acts as a “co-pilot,” handling repetitive and high-volume tasks. Staff remain essential for complex cases, clinical judgment, exception handling, appeals, and oversight especially where payer criteria are intricate or evolving.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








