Key Elements in Patient-Centered and Value-Based Care Delivery

Modern healthcare is moving away from volume-driven care toward outcomes-driven delivery. Two frameworks are leading this shift: patient-centered care and value-based care. One focuses on engaging patients in their care journey, while the other ties reimbursement to quality metrics and long-term outcomes. We understand that transitioning to these new care models can feel overwhelming for healthcare providers, who must balance clinical excellence with complex documentation and reimbursement demands. When combined, they create a more responsive, accountable system. But making them work in everyday settings requires more than clinical alignment; it demands accurate documentation, timely coding, and coordinated workflows.
In this blog, we explore the building blocks that bring these models to life, starting with the foundation: patient-centered care.
TL;DR (Key Takeaways)
- One framework is not enough. True care transformation happens when patient-centered empathy is paired with value-based accountability.
- Care delivery success depends on execution. Clean documentation, accurate coding, and coordinated workflows are just as critical as clinical decisions.
- Technology is not just a support tool. Platforms that embed compliance, improve coding precision, and surface quality insights in real time.
- Common pitfalls include siloed systems and inconsistent documentation. These operational blind spots often derail even well-intentioned care models.
- Start small but think system-wide. Embed automation, enable interoperability, and make compliance effortless at the point of care.
What Is Patient-Centered Care?
Patient-centered care places the individual, not the condition, at the center of every clinical decision. It emphasizes shared decision-making, respect for patient autonomy, and a tailored approach based on lifestyle, culture, and goals.
Rather than delivering one-size-fits-all treatment, providers collaborate with patients to develop care plans that reflect both clinical priorities and personal values.
At its core, this model is built on:
- Individual Preferences: Recognizing each patient’s specific needs, cultural background, and goals during diagnosis, treatment, and follow-up
- Respect and Engagement: Actively listening, involving patients in conversations about their care, and honoring their choices
- Shared Decision-Making: Guiding patients through options and risks, then jointly selecting treatments that align with best practices and patient priorities
Example in Practice:
A patient diagnosed with Type 2 diabetes isn’t simply given a prescription and sent home. In a patient-centered approach, the provider also considers the patient’s eating habits, physical activity, stress levels, and living environment. The care team might recommend nutritional counseling, schedule regular follow-ups, send mobile reminders, and connect the patient with community support, tailoring the plan to the individual’s lifestyle and motivation.
This personalized engagement builds trust, strengthens adherence, and reduces avoidable complications. It also improves patient satisfaction and leads to more meaningful care experiences.
What Is Value-Based Care?
Value-based care is a healthcare delivery and payment model that ties provider reimbursement to patient outcomes instead of the volume of services. The focus is on delivering measurable improvements in health while managing long-term costs and ensuring care quality.
This model encourages preventive care, better management of chronic conditions, and a more holistic approach to wellness.
Core principles include:
- Outcomes Over Volume: Providers are rewarded based on clinical outcomes and patient satisfaction, not the number of tests or procedures
- Cost Efficiency: Incentives are aligned with reducing redundant care, preventing complications, and improving coordination
- Chronic Care Management: Emphasis is placed on managing long-term conditions like diabetes or hypertension through regular monitoring and proactive support
How Reimbursement Works:
Value-based contracts use quality benchmarks to determine payments. Common metrics include:
- Lower hospital readmission rates
- Improved A1C levels for patients with diabetes
- Completion of preventive screenings and annual wellness visits
To support this, providers rely on shared electronic health records, structured documentation, and timely interventions. Accurate coding and real-time data capture are crucial for representing patient complexity, ensuring compliant billing, and enabling fair, risk-adjusted reimbursement.
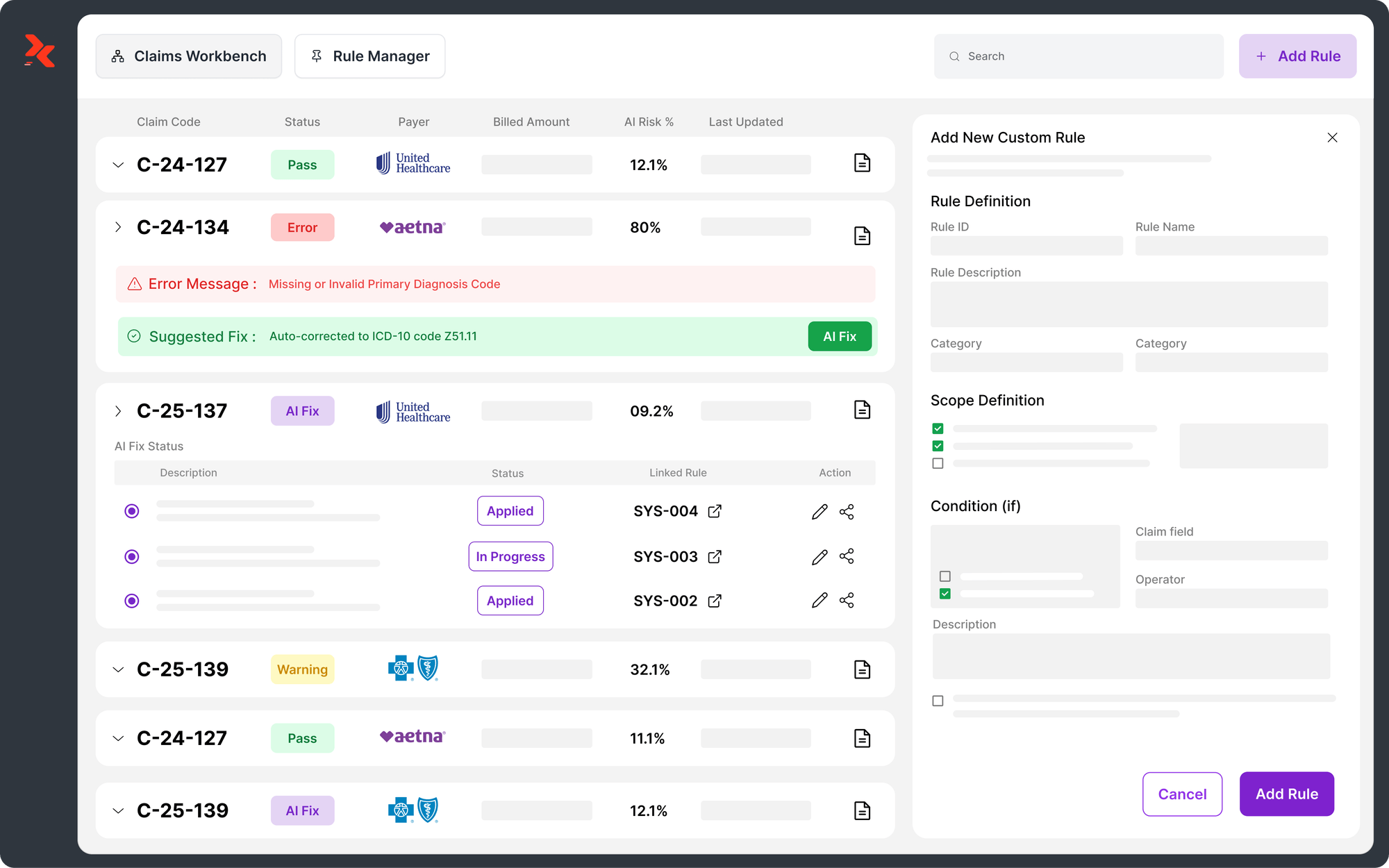
Key Elements in Patient-Centered and Value-Based Care
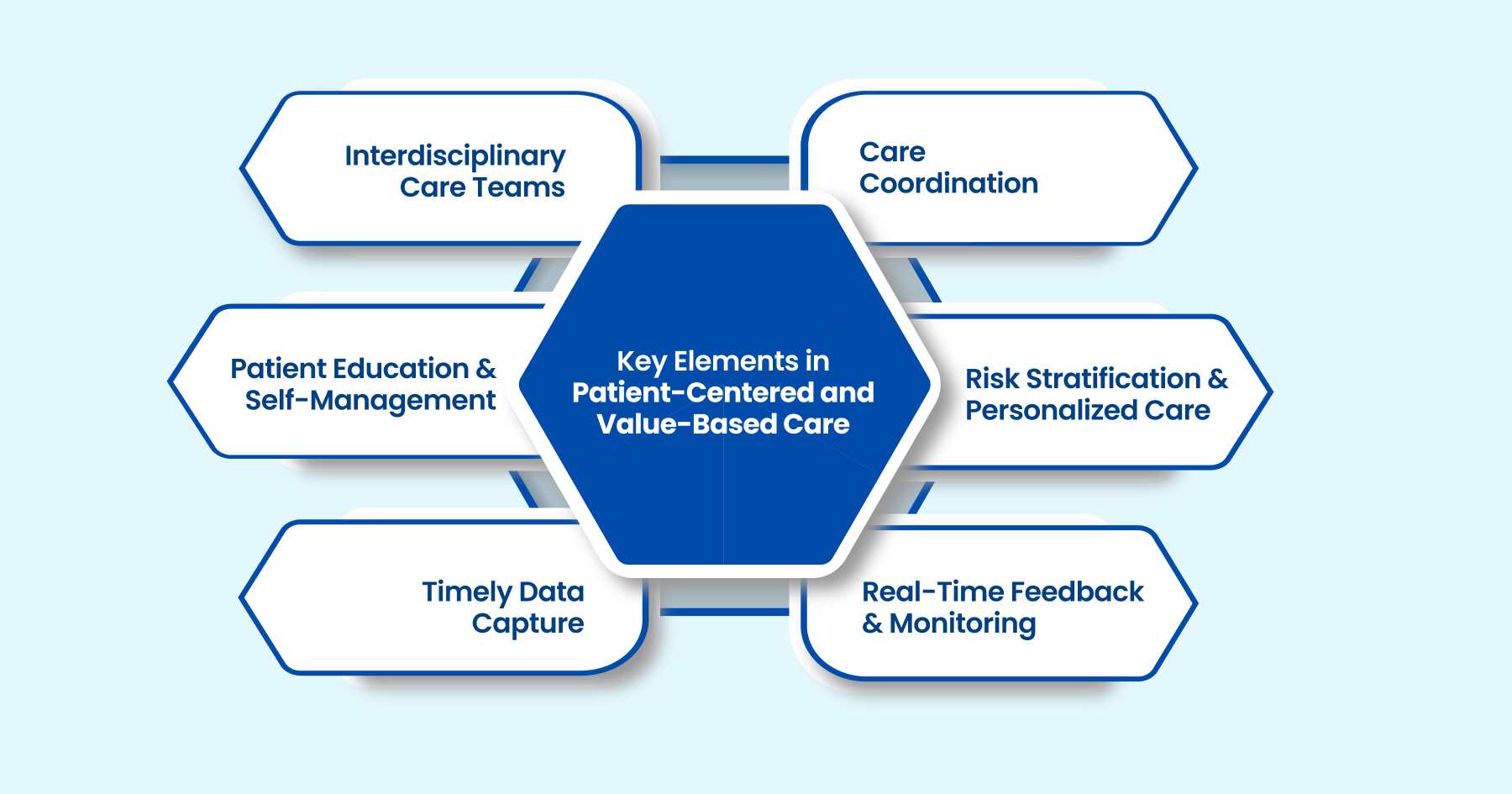
Delivering on the promise of patient-centered and value-based care requires more than good intentions. It takes synchronized workflows, structured data systems, and clear communication to ensure that providers act proactively and consistently.
Here are the foundational components that bring both care models into daily practice:
- Interdisciplinary Care Teams: Effective delivery depends on coordinated input from primary care providers, specialists, mental health professionals, and social workers. These teams share accountability for patient outcomes and work from a unified care plan.
- Care Coordination Infrastructure: Patients often move between different facilities and providers. Shared documentation, standardized protocols, and real-time communication tools help ensure smooth transitions and avoid duplicative care.
- Patient Education and Self-Management Tools: Patients who understand their conditions are more likely to follow treatment plans. Educational content, symptom tracking, and mobile reminders empower individuals to stay engaged in their care.
- Risk Stratification and Personalized Care Plans: Not all patients need the same level of support. Identifying high-risk individuals based on health status and social factors helps tailor care plans for better outcomes.
- Timely Data Capture and Reporting: Capturing structured data in real time supports everything from accurate billing to tracking performance metrics. It ensures that no critical details are missed.
- Real-Time Feedback and Quality Monitoring: Dashboards and analytic tools provide insight into what is working and what needs improvement. This allows for timely interventions and supports continuous improvement across the care cycle.
Together, these elements form the operational foundation needed to deliver care that is both empathetic and efficient, with measurable improvements in outcomes and patient satisfaction.
How Technology Bridges the Gap Between Intention and Execution
Despite strong frameworks like patient-centered and value-based care, many healthcare organizations struggle to put theory into consistent daily practice. The challenge isn’t a lack of will. It’s often a matter of fragmented tools, siloed data, and delayed feedback loops. This is where technology becomes the enabler.
1. Smart Documentation at the Point of Care
Clinical decisions happen in real time, and the supporting systems must keep pace. Modern platforms help providers document care activities as they occur, reducing reliance on retrospective data entry or memory-based coding. This ensures that nuanced decisions such as education provided or patient concerns addressed are accurately reflected in structured formats.
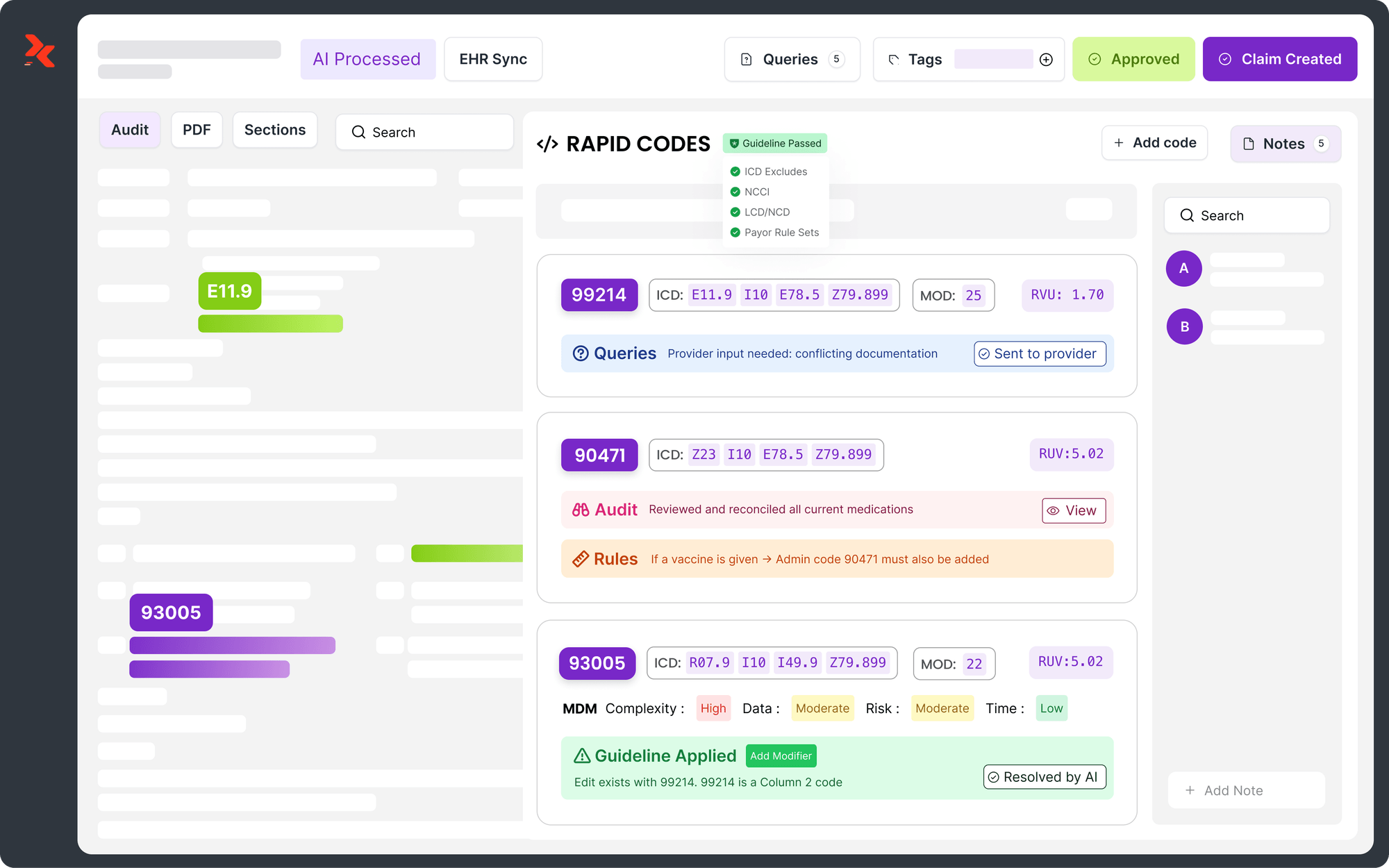
2. Intelligent Coding Assistance
Even minor gaps in coding can lead to underpayment, compliance issues, or a distorted picture of population health. AI-driven tools like RapidClaims provide contextual suggestions during the coding process, improving both speed and precision. By flagging potential omissions or mismatches upfront, they reduce the risk of denials and rework.
3. Workflow Integration Across Systems
A well-coordinated care plan means little if the data sits in disconnected silos. Seamless interoperability between EHRs, billing platforms, analytics dashboards, and care coordination systems ensures that each stakeholder works from a single source of truth. This helps synchronize tasks, eliminate duplication, and keep everyone aligned on goals and responsibilities.
4. Real-Time Quality Signal Tracking
Modern platforms surface performance insights during active workflows, not just in retrospective reports. Providers can adjust care plans, identify trends, or trigger interventions before minor issues escalate. This proactive approach supports continuous quality improvement rather than reactive corrections.
5. Audit Readiness by Design
Instead of scrambling for documentation during payer reviews, digital systems can embed compliance logic into the workflow itself. Tools that guide the user to collect supporting data during care delivery, such as time-stamped notes, patient consent, or clinical rationale, help maintain a complete and defensible record from day one.
By embedding these capabilities into daily operations, technology transforms intention into repeatable action. It enables healthcare teams to move from knowing what to do, to doing it well and proving it with data.
Common Gaps That Undermine Patient-Centered, Value-Based Delivery
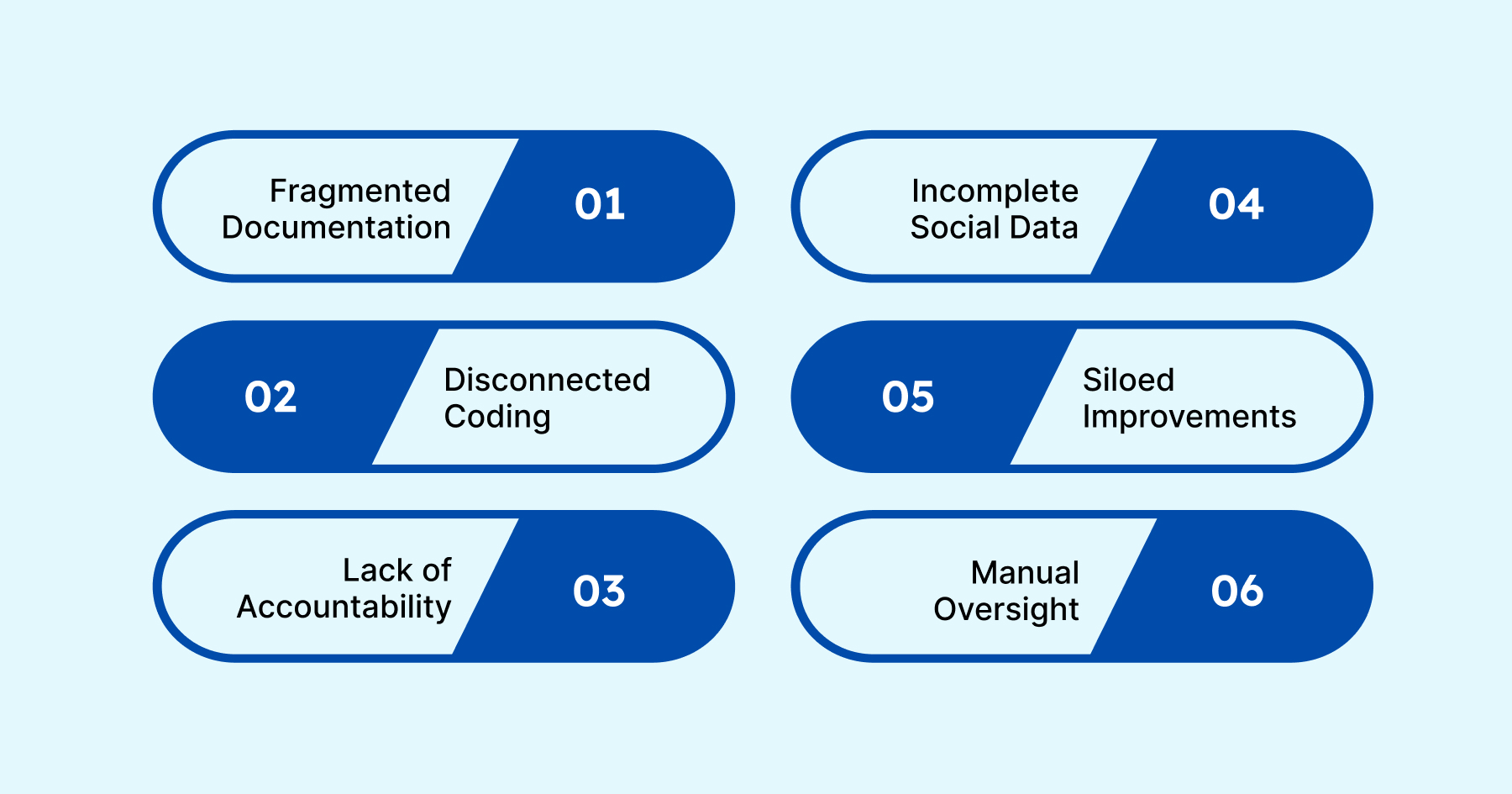
Even with strong intentions and robust technology, execution gaps can still derail outcomes. These issues often arise not from poor care but from operational blind spots and misaligned workflows.
- Fragmented Documentation Habits: When providers document inconsistently or after the fact, critical care actions can be lost, misrepresented, or misaligned with coding requirements.
- Disconnected Coding Processes: Coding delays or workflows that sit outside the care process can lead to inaccurate reporting, compliance risks, and missed reimbursements.
- Accountability Without Feedback Loops: Without real-time alerts or task escalation pathways, it is difficult to monitor whether documentation, coding, or follow-up responsibilities were completed or where breakdowns occurred.
- Incomplete Capture of Social Determinants: Clinical data alone does not tell the full story. Without visibility into housing, transport, or food security, care plans can fall short of a patient’s actual needs.
- Siloed Improvement Efforts: When quality teams operate separately from clinical operations, insights become retrospective. Embedding feedback directly into workflows ensures faster adjustments and greater impact.
- Manual Oversight Without Automation: Relying solely on human review for compliance and documentation checks slows down processes and increases the chance of error. Tools like RapidClaims help automate validation and support consistency at scale.
Addressing these challenges requires systems that guide the right actions in real time, not just policies or training. True transformation happens when day-to-day decisions are supported by embedded tools and connected processes.
Final Thoughts
Patient-centered, value-based care is more than a philosophy. It is a measurable standard that depends on effective execution. From the provider’s intention at the point of care to the final detail in a claim, each step must align clinically, operationally, and technologically.
Bridging the gap is not a one-time fix. It is a continuous process supported by integrated workflows, real-time feedback, and intelligent automation. Whether you are a physician, coder, or administrator, your ability to work in sync with others ultimately determines outcomes and reimbursement.
One platform can make a real difference. Tools like RapidClaims help bring everything together, streamlining documentation, improving coding accuracy, and ensuring audit-ready compliance from day one.
Want to see how it works in action? Request a demo and discover how RapidClaims can help your team move from knowing what to do to doing it well and proving it with data.
Frequently Asked Questions (FAQ)
1. How is patient-centered care different from traditional care models?
Ans: Patient-centered care places the patient’s values, lifestyle, and preferences at the core of decision-making, unlike traditional models that often prioritize provider-driven choices or efficiency metrics alone.
2. What types of healthcare organizations benefit most from value-based care?
Ans: Primary care groups, ACOs (Accountable Care Organizations), specialty practices managing chronic conditions, and integrated health systems typically see strong ROI when implementing value-based models due to better care coordination and risk-sharing incentives.
3. Is value-based care only about reducing costs?
Ans: No. While cost savings are a goal, the primary focus is improving outcomes, reducing unnecessary interventions, and enhancing the patient experience. All of these contribute to more sustainable and effective healthcare delivery.
4. What role does technology play in these care models?
Ans: Technology acts as the operational backbone, enabling real-time documentation, seamless data sharing, proactive alerts, and intelligent coding support. Platforms like RapidClaims help teams align clinical intent with compliance and billing accuracy.
5. How can providers transition toward these models without disrupting current workflows?
Ans: Start with phased implementations. Adopt interoperable tools, train staff on patient engagement practices, and introduce real-time documentation support. Aligning tech with existing workflows minimizes friction and accelerates ROI.
6. Are there risks in adopting patient-centered or value-based care?
Ans: Challenges include the need for cultural change, upfront investment in technology, and ongoing training. However, the long-term benefits in care quality, compliance, and reimbursement generally outweigh the risks.
.png)
Ayeesha Siddiqua
Ayeesha Siddiqua is a highly experienced medical coding professional with 22 years of expertise in E/M Outpatient, Radiology, and Interventional Radiology (IVR), ensuring coding accuracy, regulatory compliance, and optimized reimbursements at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products
%201.png)

.jpg)