.webp)
Outpatient Coding and Documentation Simplified


Outpatient coding may be routine in healthcare, but it’s far from simple. With ever-changing evaluation and management (E/M) guidelines, increasing scrutiny on clinical documentation, and the constant pressure to avoid undercoding or denials, even seasoned physicians and coders face challenges getting it right.
Recent studies have shown that providers — especially residents — often undercode outpatient visits, even when the clinical complexity would justify higher-level evaluation and management codes. These trends point to a larger issue: the gap between care delivery, documentation, and accurate code selection. And in today’s outpatient-driven healthcare landscape, that gap doesn’t just impact revenue — it affects compliance, reporting accuracy, and patient care visibility.
In this blog, we’ll break down the fundamentals of outpatient E/M coding, highlight recent updates, and share practical strategies (including how AI-powered platforms like RapidClaims can help) to simplify evaluation and management codes, improve documentation quality, and minimize denials. Here’s a quick overview of what we’ll cover:
What Is Outpatient E/M Coding?
Outpatient E/M coding refers to the process of assigning codes for the evaluation and management of patients in outpatient settings. These codes are used to categorize the complexity and length of a patient visit, which directly influences billing and reimbursement.
For example, imagine a primary care physician has two patients:
- Patient A: A new patient with a history of hypertension presenting with headaches. The physician needs to perform a full examination, order tests, and provide a treatment plan.
- Patient B: An established patient with well-controlled hypertension, coming in for a routine follow-up with no new issues. The physician only spends a few minutes reviewing the patient's progress.
For Patient A, the physician would likely assign a higher-level evaluation and management codes (e.g., 99203) because the visit involves a detailed history, examination, and decision-making. In contrast, Patient B may be assigned a lower-level E/M code (e.g., 99213) due to the simpler, routine nature of the visit.
Accurate outpatient E/M coding helps ensure appropriate reimbursement for both the complexity of care and the time spent with the patient. Errors in coding or documentation could lead to denials or incorrect payments.
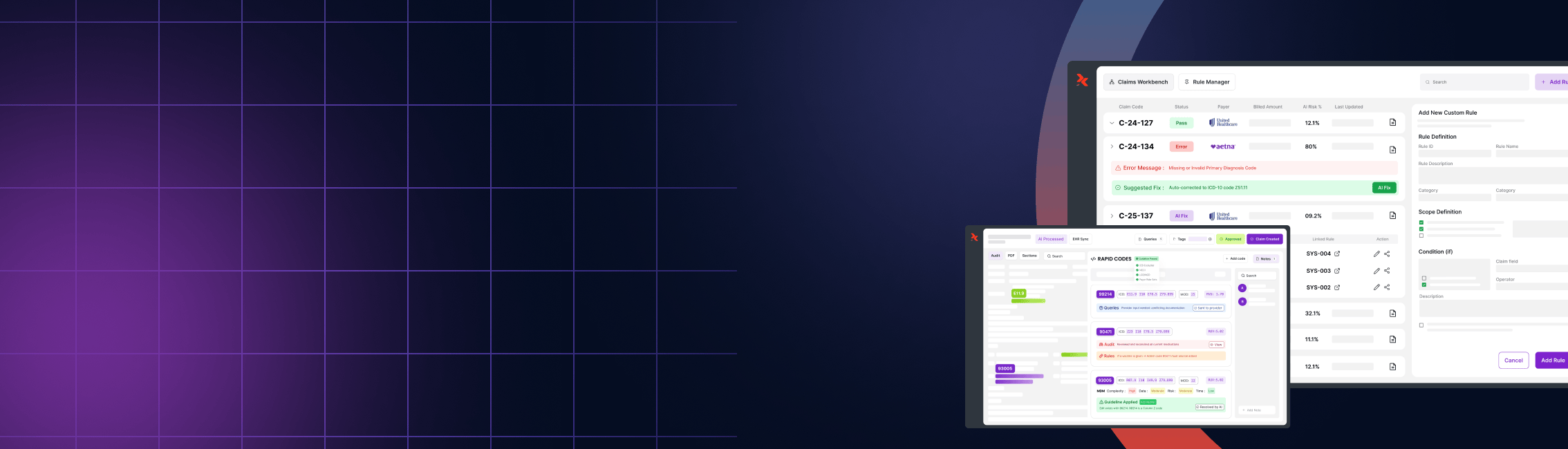
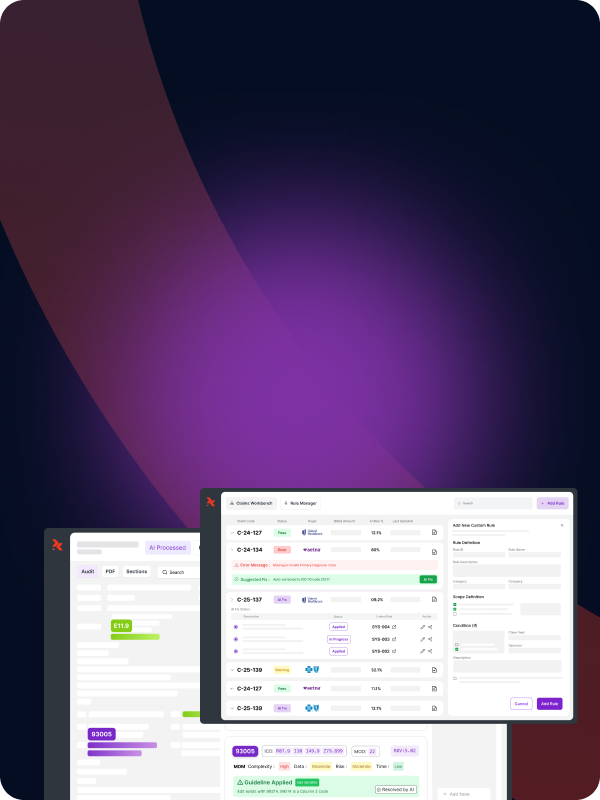
RapidClaims can assist in this process by automating the evaluation and management codes selection based on the documentation provided, reducing human error and increasing the speed of claim processing.

The platform uses AI-driven insights to identify the correct code based on the complexity of the visit and ensures that the documentation aligns with coding requirements, minimizing the risk of claim denials.
Want to reduce E/M coding errors? Request a demo and see how RapidClaims automates compliance.
Check out RapidClaims’ Proven Impact below:
Also Read: Claim Denials: Common Reasons and How to Effectively Resolve Them
Key Guidelines for Effective Outpatient Documentation
Proper and detailed documentation is crucial for accurate outpatient E/M coding. It ensures that the services provided align with the codes selected and helps prevent billing errors or claim denials.
Key guidelines include:
1. Comprehensive Patient History
Ensure the patient’s medical history is thoroughly documented, including current symptoms, diagnoses, medications, and previous treatments.
For instance, when coding for a follow-up visit, the documentation should clearly reflect any changes or lack thereof in the patient's condition.
2. Clear Documentation of Decision Making
For each encounter, the physician’s decision-making process should be detailed. This includes why certain tests were ordered or why a particular treatment plan was chosen.
Proper documentation of this decision-making process ensures that the assigned evaluation and management code accurately reflects the level of service provided.
3. Time-Sensitive Information
In cases where time-based coding is used (e.g., prolonged services), detailed records of the time spent with the patient must be included. This ensures that evaluation and management codes based on time, such as 99215, are used correctly.
4. Accurate Diagnosis and Procedure Coding
It's important that the diagnoses and procedures documented in the patient record match the codes assigned. Inaccurate or incomplete documentation can lead to claims being denied or rejected.
RapidClaims supports this process by integrating with Electronic Health Records (EHRs) and using AI to ensure that documentation aligns with the correct outpatient E/M coding.

By automatically suggesting missing elements or identifying gaps in documentation, RapidClaims helps reduce manual errors and ensures compliance with evaluation and management code standards. This results in smoother, more efficient billing and fewer claim denials.
Also Read: Differences and Basics of ICD-10 and CPT Codes
Recent Updates to Outpatient E/M Codes
Outpatient E/M coding has undergone significant changes in recent years, with the most notable updates being implemented in 2023. The 2023 E/M updates aim to simplify the coding process, reduce administrative burdens, and improve the accuracy of claims. Some key updates include:
1. Removal of History and Physical Exam Requirements for Code Selection
In the past, selecting the correct evaluation and management codes heavily relied on documenting specific elements of the patient's history and physical exam. The 2023 E/M updates allow physicians to focus more on the complexity of the decision-making process rather than the specific details of the exam and history, which can be time-consuming.
2. Increased Emphasis on Medical Decision Making (MDM)
The level of service for outpatient visits is now more closely tied to the complexity of medical decision-making (MDM). Physicians should document their thought process behind diagnosis, treatment plans, and the potential risks to the patient, which will help guide the code selection.
3. Time-Based Coding Simplification
For certain cases, such as follow-up visits, time-based coding has become more streamlined. Physicians can now base code selection more easily on the total time spent on the encounter, without being required to separate out time spent on counseling and coordination of care.
4. Telehealth and Virtual Visit Coding
With the rise of telehealth, the updated evaluation and management codes reflect a more flexible approach to coding virtual visits, ensuring that these services are reimbursed appropriately based on their complexity and time spent.
Important Note:
The 2023 E/M updates aim to make outpatient E/M coding less burdensome for providers while maintaining the accuracy needed for appropriate reimbursement. These changes also highlight the importance of maintaining updated knowledge and ensuring that documentation reflects the current standards.
Keeping up with these updates can be challenging, but platforms like RapidClaims continuously update their coding logic based on the latest CMS and AMA guidelines, helping providers stay compliant without manual reconfiguration.
Also Read: Understanding HCC Coding and Risk Adjustment
Exclusions and Special Considerations in Outpatient E/M Codes
When it comes to outpatient E/M coding, there are specific services and situations that are excluded from these codes, and recognizing them is vital to ensuring accurate billing. A few key exclusions and special considerations include:
1. Procedures That Are Not Covered by E/M Codes
Some medical services, such as surgeries or diagnostic procedures, require separate procedure codes, like CPT codes, instead of an E/M code. For example, a knee replacement or a colonoscopy would not fall under E/M coding, even if they are performed during an outpatient visit.
2. Excluded Services for Hospital Visits
Outpatient E/M codes (99202–99215) are designated for office or other outpatient services. Inpatient services, including hospital admissions and inpatient consultations, have their own distinct E/M codes (e.g., 99221–99239 for hospital inpatient services). It's essential to select the appropriate E/M code based on the setting and nature of the service provided.
3. Bundled Services
In bundled payment models, multiple services provided during a defined episode of care are reimbursed under a single payment. For example, post-operative visits within a 90-day global period are included in the bundled payment for the surgery and should not be billed separately with E/M codes. However, if an unrelated E/M service is provided during this period, it may be billed separately with appropriate modifiers and documentation.
4. Use of Separate Diagnosis Codes
Often, the documentation of the patient’s diagnosis will indicate a need for specific diagnosis codes (ICD-10), which must be separately documented in addition to the E/M code. Failure to document these accurately can lead to incomplete claims or denials.
Pro Tips:
Given the complexity of these exclusions, it’s important to have a system in place to ensure that services are categorized correctly.
RapidClaims helps by utilizing AI to automatically recognize and flag services that fall outside the scope of E/M coding, ensuring that claims are more accurate and complete.
Resources and Tools for Outpatient E/M Coding

Navigating E/M coding can be challenging, but using the right resources and tools can make the process smoother. Whether you're a coder, physician, or healthcare administrator, having the right support can help avoid costly mistakes and improve efficiency.
Here’s a look at some essential resources:
1. AMA and CMS Guidelines
The American Medical Association (AMA) and Centers for Medicare & Medicaid Services (CMS) offer the primary guidelines for outpatient E/M coding. These documents lay out exactly what needs to be documented for each service, helping you select the correct evaluation and management codes. Keeping up with any updates from these organizations is essential to avoid errors and stay compliant.
2. Coding Books and Manuals
While they might seem old-school in today’s digital world, coding books like the CPT Codebook and ICD-10 Coding Manual remain crucial tools for coders. These resources provide clear definitions and rules for each code, ensuring that you know exactly which one to use for any given situation. Although referencing them might take a bit more time, they are incredibly helpful for understanding the details.
3. Online Coding Tools and Software
Many hospitals and billing companies use online platforms to streamline the coding process. These tools help by automatically suggesting the correct E/M codes based on the patient's chart. Using this technology can save time, reduce errors, and increase the accuracy of your coding.
4. Training and Education
The world of E/M coding is constantly changing, so it’s important to keep learning. Organizations like AAPC and AHIMA offer courses and certifications to keep coders up to date on the latest guidelines and best practices. Regular training ensures that coders stay sharp and can handle new challenges confidently.
5. Code Lookup and Error-Checking Tools
Today’s coding software goes beyond just suggesting codes. Many platforms include built-in error-checking features that scan for mistakes in the codes or missing documentation. This helps catch potential problems before claims are submitted, reducing the chances of denials or delays.
By tapping into these resources, healthcare teams can navigate the complexities of E/M coding more effectively. Not only does this ensure accuracy, but it also helps providers stay compliant with changing regulations, keeping revenue cycles running smoothly.
Conclusion
Outpatient E/M coding is no longer just a billing formality — it's a critical part of documenting care, justifying medical decisions, and ensuring fair reimbursement. As coding guidelines evolve and documentation requirements grow more complex, the margin for error continues to shrink.
By combining accurate documentation support, AI-driven code suggestions, and constantly updated coding logic, RapidClaims helps outpatient practices improve accuracy, stay compliant, and reduce costly denials. From identifying documentation gaps to assisting with E/M code selection based on complexity and guidelines, RapidClaims streamlines the outpatient coding process.
Don't Risk Denials or Revenue Loss: Book Your E/M Audit Today to Master the 2023+ Updates Before Q3 Deadlines Strike
Frequently Asked Questions (FAQ)
1. What is outpatient E/M coding?
Outpatient E/M (Evaluation and Management) coding refers to the assignment of billing codes based on the complexity, time, and decision-making involved in treating patients in an outpatient setting, such as a clinic or physician’s office. These codes directly impact reimbursement from payers like Medicare or private insurers.
2. Why is accurate outpatient coding so important?
Accurate coding ensures proper reimbursement, reduces the risk of audits or denials, and reflects the true complexity of care provided. Inaccurate coding can lead to underpayments, compliance issues, or misrepresentation of patient care.
3. What E/M documentation requirements changed in the 2023 E/M guidelines?
The 2023 E/M updates simplified coding by:
- Removing detailed history and physical exam requirements for code selection
- Emphasizing medical decision-making (MDM)
- Allowing more flexible time-based coding
- Expanding and standardizing rules around telehealth visits
These changes aim to reduce administrative burden while aligning documentation with clinical complexity.
4. What are common reasons for outpatient coding errors?
Common issues include:
- Incomplete or vague documentation
- Undercoding due to conservative code selection
- Using outdated E/M guidelines
- Confusion between outpatient and inpatient codes
- Failing to document time when using time-based coding
5. How can AI tools like RapidClaims help with outpatient E/M coding?
RapidClaims uses AI to:
- Analyze clinical notes in real time
- Suggest the most appropriate E/M codes
- Identify documentation gaps or missing elements
- Stay current with coding updates and payer rules
- Reduce claim denials and speed up reimbursement
6. Do outpatient E/M codes apply to all services?
No. Outpatient E/M codes (99202–99215) are used for office visits and similar outpatient care. Procedures, diagnostic tests, inpatient care, and services under bundled payment models often require different coding and must be billed separately or with modifiers when appropriate.
%201.png)