Applications of Machine Learning in Medicine for Coding and Billing

Healthcare organizations are rethinking how they manage coding and billing as documentation grows faster than available staffing. Coders must interpret increasingly complex narratives, keep up with frequent regulatory updates, and maintain accuracy under higher workloads. These pressures contribute to avoidable denials, longer A/R cycles, and inconsistent reimbursement.
Machine learning in medicine is moving from research settings into everyday revenue cycle operations. Its ability to interpret clinical text, recognize coding patterns, and deliver real-time quality checks gives organizations a practical way to improve coding accuracy and stabilize financial performance. Unlike rule-based tools, ML improves as it processes more encounters, making it well suited for large and variable EHR data.
This shift is measurable. The global AI in revenue cycle management market reached USD 20.63 billion in 2024, reflecting broad investment in tools that support documentation review and code assignment. As clinical and billing data grow more complex, machine learning provides a scalable way to reduce manual review, increase coding consistency, and support more reliable reimbursement.
Key Takeaways
- Machine learning in medicine strengthens coding and billing by interpreting clinical notes, identifying key details, and supporting accurate code selection.
- ML helps revenue cycle teams keep pace with rising documentation volume, varied provider styles, and frequent payer rule changes.
- High-value applications include resolving ambiguous language, spotting subtle clinical indicators, predicting denial risk, validating billing details, routing charts by complexity, and supporting risk adjustment.
- ML learns from real coding patterns and payer outcomes, improving consistency across coders, specialties, and encounter types.
- Strong implementation requires clean data, clear coder review rules, payer-aligned tuning, structured documentation feedback, performance monitoring, and audit transparency.
- Common challenges include specialty-specific terminology, complex encounters, limited model clarity, changing payer requirements, and uneven coder acceptance.
- Key trends include EHR-integrated coding cues, timeline-based clinical interpretation, pre-claim risk forecasting, automated audit evidence packets, and specialty-tuned models.
Table of Contents:
- What Is Machine Learning in Medical Coding and Billing?
- Why Revenue Cycle Teams Should Care About Machine Learning in Medicine
- High-Impact Use Cases of Machine Learning in Medicine for Coding & Billing
- How Machine Learning Works Behind the Scenes in Medicine and RCM Workflows
- Best Practices for Implementing Machine Learning in Medicine within the Revenue Cycle
- Common Challenges in Applying Machine Learning in Medicine and How to Address Them
- Emerging Trends in Machine Learning in Medicine That Are Transforming Billing and Coding
- How RapidClaims Applies Machine Learning to Modernize Coding and Billing
- Conclusion
- FAQs
What Is Machine Learning in Medical Coding and Billing?
Machine learning in coding and billing focuses on recognizing how real clinical documentation translates into actual coding decisions and claim outcomes. Instead of relying on static rules, ML learns from thousands of encounters to spot patterns that coders and auditors deal with every day.

More specifically, ML systems are designed to:
- Interpret physician language as it is written, including shorthand, specialty phrasing, and mixed narrative styles.
- Match documentation to likely ICD-10, CPT, or HCC codes based on how similar cases were coded and paid.
- Detect patterns that typically lead to coding discrepancies, such as unsupported diagnoses or incomplete procedure descriptions.
- Identify when encounters resemble previously denied claims, allowing teams to intervene before billing.
- Adapt when providers, specialties, or payers shift their expectations, which keeps recommendations relevant over time.
The goal is not to automate coding end-to-end. It is to give coders a clearer starting point, reduce the time spent searching through long notes, and help billing teams produce claims that align with payer behavior.
Why Revenue Cycle Teams Should Care About Machine Learning in Medicine
Revenue cycle teams face challenges that are difficult to solve through manual review alone. Coding managers must manage wide variation in clinician documentation, compliance officers must ensure alignment with frequently updated guidelines, and RCM leaders must reduce denials without slowing throughput. These pressures create very specific operational gaps.
Machine learning helps address these gaps by:
- Surfacing the clinical details that directly influence code accuracy, even when buried in long or inconsistent notes.
- Highlighting encounters that are likely to trigger payer scrutiny, allowing teams to fix issues before claims leave the door.
- Normalizing coding decisions across providers and locations, which reduces variability that leads to audit findings.
- Supporting specialties with higher documentation complexity, where coding errors are harder to catch manually.
- Keeping pace with new patterns in payer edits and remittance behavior, which manual workflows cannot track consistently.
In short, ML strengthens the parts of the revenue cycle that depend on fast, accurate interpretation of clinical text and real-world payer outcomes. It gives coding and RCM teams tools that match the scale and complexity of today’s documentation environment without replacing the expertise they bring to the process.
High-Impact Use Cases of Machine Learning in Medicine for Coding & Billing
Machine learning is most effective when it supports the specific decision points that create friction in coding and billing workflows. Instead of automating entire tasks, ML enhances the steps where human review is most likely to miss patterns, overlook details, or spend unnecessary time.
Here are the applications that create the strongest operational impact without repeating earlier concepts:
- Targeted code identification for ambiguous language: ML helps coders interpret phrasing that varies widely across clinicians, such as nonstandard abbreviations or incomplete condition statements. This reduces time spent clarifying intent and prevents misclassification.
- Detection of subtle clinical indicators tied to coding outcomes: Certain diagnoses and procedure nuances are easy to miss when buried in long narratives. ML highlights these details so coders do not need to read the entire note multiple times to confirm completeness.
- Pre-claim risk scoring based on payer behavior: By learning from past payer decisions, ML assigns a risk score to each encounter, helping teams know which charts require extra review before submission. This prevents denials that stem from patterns too subtle for manual review.
- Focused support for multi-condition encounters: Encounters with multiple active problems or procedures often create uncertainty around sequencing, linkage, and code grouping. ML identifies patterns in similar historical cases to guide coders toward consistent decisions.
- Automated validation of billing-critical elements: ML checks for documentation elements that directly affect billing, such as laterality, graft details, anesthesia specifics, or chronic condition status. These are common areas where incomplete documentation leads to rework.
- Priority-based chart routing: Instead of routing charts by time received, ML evaluates encounter complexity and documentation density. This helps coding leaders optimize queues and maintain steady throughput across specialties.
- Support for capturing risk-sensitive conditions: For organizations participating in risk adjustment, ML surfaces condition clues that may affect RAF scores but are not immediately obvious. Coders can validate these suggestions without manually searching the note.
These applications reflect how ML improves accuracy and efficiency by strengthening the points in the workflow that require most human judgment, rather than duplicating tasks already covered in previous sections.
How Machine Learning Works Behind the Scenes in Medicine and RCM Workflows
Machine learning in the revenue cycle works by capturing the specific decision logic that coders, auditors, and payers apply every day. Instead of functioning as a broad automation tool, ML models learn the subtle patterns that determine whether documentation supports a code, whether a payer is likely to accept a claim, and where coders typically spend the most time validating information.
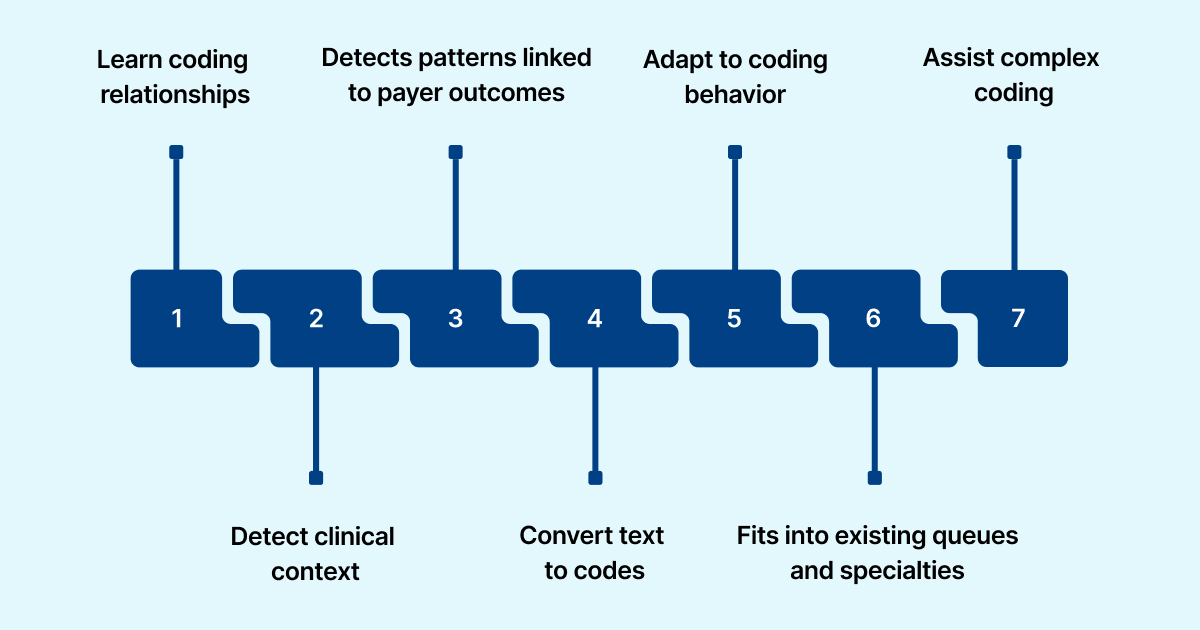
A more precise view of how it works in practice:
- Learns from detailed note-to-code relationships: ML models study how coders interpret assessment language, procedure descriptions, and diagnostic qualifiers. This allows the system to recognize whether documentation truly supports a code rather than simply containing the right terms.
- Identifies clinical context that influences code selection: For example, it can distinguish whether a symptom is part of a chronic condition, a new finding, or a postoperative complication. These distinctions matter for sequencing, specificity, and modifier use.
- Detects patterns linked to payer outcomes: The model learns which documentation gaps or code combinations have historically triggered denials from specific payers. This insight lets it flag high-risk encounters before billing.
- Transforms narrative text into coding-relevant signals: Instead of extracting generic keywords, ML isolates the parts of the note that drive coding decisions, such as severity terms, procedure details, or supporting exam findings.
- Adapts to each organization’s coding behavior: Every coding team has slightly different review habits. ML incorporates these tendencies through coder acceptance, rejection, and adjustment patterns, improving alignment over time.
- Fits into existing queues and specialties: ML can route encounters based on predicted complexity, documentation density, or specialty-specific differences, helping coding leaders manage workflow distribution more efficiently.
- Supports complex encounters without overriding coder judgment: For charts involving multiple conditions, overlapping timelines, or unclear documentation, ML provides context cues rather than full recommendations, ensuring coders retain control where clinical nuance is critical.
This approach allows machine learning to strengthen the exact decision points that affect coding quality, claim acceptance, and operational efficiency rather than applying a generic automation layer across the revenue cycle.
Want to understand which parts of your documentation and coding workflow create the most preventable denials? RapidClaims can analyze a sample set of encounters and show where ML-driven insights would reduce friction and improve accuracy.
Best Practices for Implementing Machine Learning in Medicine within the Revenue Cycle
Successful ML adoption in the revenue cycle depends on precise operational guardrails rather than broad automation plans. Coding, RCM, and compliance leaders need controls that keep outputs accurate, transparent, and aligned with payer and regulatory expectations.
Here is a more concise, non-generic version of the section:
- Build training data that reflects real coding variation: Include encounters from high- and low-volume specialties, charts with auditor corrections, and denial-linked cases. This allows the model to learn the nuances coders regularly navigate.
- Define when and how coders should validate ML outputs: Set rules for sensitive code categories, confidence thresholds for suggestions, and documentation elements that must be present before ML recommendations are used.
- Embed payer behavior into the model: Use clearinghouse edits, prior authorization outcomes, and payer-specific denial messages to shape retraining. This keeps ML aligned with current adjudication patterns.
- Create a structured pathway for documentation improvements: Turn ML-identified issues into specific provider feedback or template updates instead of leaving them as one-off coding fixes.
- Monitor specialty-level performance: Track acceptance rates and accuracy by specialty rather than systemwide averages. This reveals where ML performs well and where retraining or specialty tuning is needed.
- Start with controlled pilots: Test ML in specialties with stable documentation and reliable historical coding. Gradually expand once the model demonstrates consistent performance.
- Maintain full visibility for compliance: Keep clear evidence markers, version histories, and coder decision logs so compliance teams can validate ML-supported coding during internal reviews or audits.
These practices ensure ML supports coding accuracy, audit readiness, and reliable reimbursement without disrupting existing revenue cycle workflows.
Common Challenges in Applying Machine Learning in Medicine and How to Address Them
Machine learning delivers meaningful value, but RCM leaders, coding managers, and compliance teams must navigate several operational and regulatory challenges to ensure dependable performance. Addressing these issues upfront helps organizations maintain accuracy and audit readiness as ML becomes part of daily workflows.
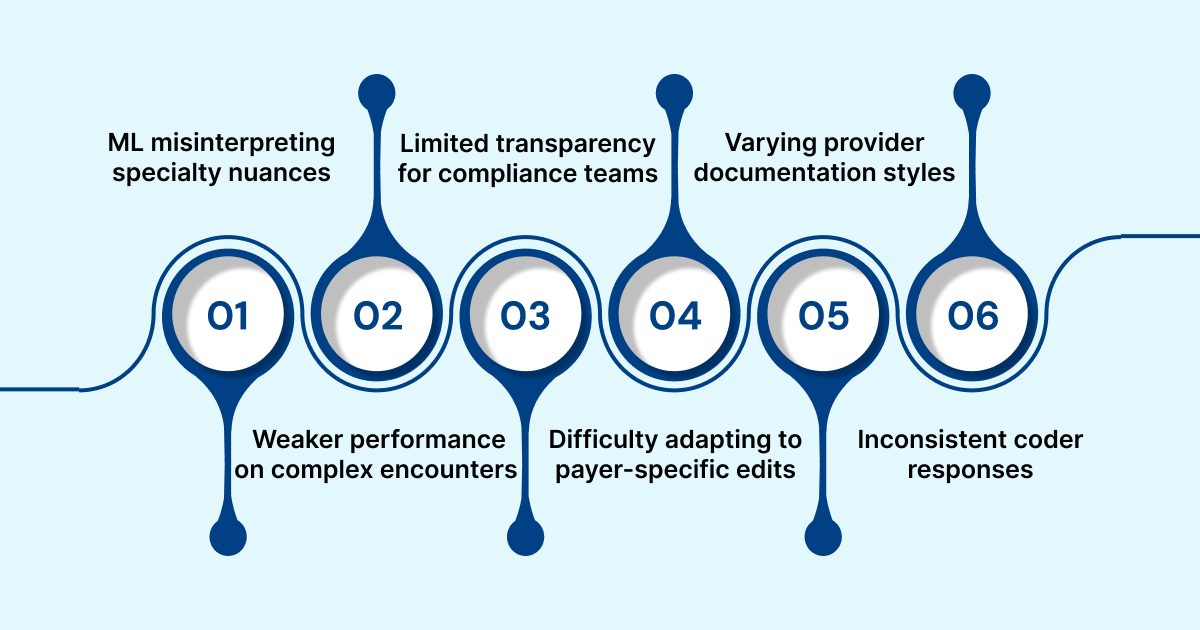
1. ML misinterpreting specialty nuances
Models trained on broad datasets may overlook specialty-specific phrasing, leading to inaccurate suggestions in areas such as cardiology, orthopedics, or behavioral health.
Solution: Use specialty-tagged datasets and validate model behavior by service line before scaling.
2. Weaker performance on complex encounters
ML tools often perform best on routine visits and struggle with multi-condition or procedure-heavy charts.
Solution: Route complex encounters for enhanced human review and reserve ML for pre-screening or documentation checks.
3. Limited transparency for compliance teams
When systems do not show how recommendations were generated, compliance staff cannot verify alignment with ICD-10, CPT, or HCC rules.
Solution: Select tools that provide evidence markers, highlighted source text, or mapped concepts to support audit workflows.
4. Difficulty adapting to payer-specific edits
Rapid shifts in payer bundling logic, modifier usage, or documentation rules can reduce model accuracy.
Solution: Incorporate clearinghouse edits, denial messages, and payer-specific remittance data into ongoing retraining cycles.
5. Documentation styles that vary across provider groups
Models may expect terminology or detail that clinicians do not consistently provide.
Solution: Deliver targeted feedback to provider groups and refine templates based on ML-identified documentation gaps.
6. Inconsistent coder responses to ML suggestions
Distributed teams may apply acceptance criteria differently, creating variability in outputs.
Solution: Define confidence thresholds, acceptance rules, and escalation paths to standardize decision-making.
These challenges underscore the need for ML systems built specifically for revenue cycle environments. RapidClaims addresses these issues with specialty-aware NLP, payer-informed model tuning, and transparent evidence trails that help coders and compliance teams validate decisions. Its human-in-the-loop workflow ensures that complex encounters receive expert oversight while ML accelerates routine review.
Emerging Trends in Machine Learning in Medicine That Are Transforming Billing and Coding
AI in the revenue cycle is shifting from retrospective review toward real-time guidance and specialty-specific intelligence. The trends below reflect where coding, compliance, and RCM leaders will see the most meaningful advancements without repeating earlier concepts.
- Coding support directly inside the EHR: AI is moving into provider-facing workflows, offering coding cues and documentation prompts as clinicians write their notes. This reduces clarification requests and strengthens documentation before coders ever touch the chart.
- Timeline-based encounter interpretation: New models evaluate the entire clinical story instead of isolated note sections. This helps with complex coding scenarios such as postoperative complications, chronic disease management, and combination codes.
- Pre-claim risk forecasting: Instead of reacting to denials, teams use ML to estimate risk at the encounter level. Charts with high predicted denial probability can be routed for enhanced review before billing.
- Automated evidence packets for audits: AI can compile supporting text, clinical indicators, and coding rationales into structured summaries. Compliance teams spend less time gathering proof during payer audits.
- Service-line-specific ML models: Smaller models trained for individual specialties improve accuracy by understanding domain-specific terminology and documentation structures.
- More consistent FHIR-based data flows: As EHRs adopt FHIR, ML systems can access data with fewer extraction issues. This improves the reliability of coding suggestions and risk scoring.
- Continuous tuning based on payer behavior: Models update when payer edits or modifier expectations change. This keeps recommendations aligned with real adjudication patterns rather than outdated rules.
Together, these trends move AI from a back-end review tool to an integrated part of coding and billing operations, helping teams avoid rework and maintain accuracy in environments with rising documentation and compliance demands.
How RapidClaims Applies Machine Learning to Modernize Coding and Billing
RapidClaims focuses on practical, revenue-cycle–specific ML capabilities that address the gaps coding and RCM leaders experience in daily operations. Instead of broad AI features, the platform delivers targeted functions that directly support coding accuracy, compliance, and workflow efficiency.
- Specialty-aware NLP: Models tuned for individual specialties interpret clinical language more precisely, reducing miscoding tied to varying documentation styles.
- Evidence-backed code suggestions: Each ML recommendation includes highlighted source text, giving coders and compliance teams immediate clarity on why a code was surfaced.
- Payer-aligned logic: RapidClaims incorporates denial trends, modifier patterns, and payer edits to help teams avoid common rejection points before claims go out.
- Proactive documentation prompts: The system identifies missing elements that could affect coding or billing, allowing coders to resolve issues before submission.
- Smart encounter routing: Straightforward charts receive ML-assisted review, while complex encounters route to coders automatically, preserving accuracy without slowing throughput.
- HCC-focused intelligence: RapidClaims surfaces potential HCC candidates using models tuned for HCC v28, helping risk-adjustment teams capture conditions that may otherwise be overlooked.
These capabilities help organizations apply machine learning where it delivers the most reliable operational impact: consistent coding, cleaner claims, and less rework.
Ready to apply machine learning to strengthen coding accuracy, improve documentation completeness, and reduce denial risk? Request a personalized RapidClaims demo to see how ML-driven review fits directly into your existing revenue cycle workflows.
Conclusion
Machine learning is becoming essential for organizations that need to keep coding and billing accurate while managing growing documentation and shifting payer expectations. Its value comes from improving consistency, strengthening decision support, and reducing the operational friction that slows down reimbursement. The examples and workflow applications in this article show how ML can support real day-to-day challenges faced by coding managers, RCM leaders, and compliance teams rather than serving as a broad or abstract automation concept.
If your organization is exploring how ML can support coding accuracy, documentation quality, or denial reduction, a practical walkthrough is the most useful next step. You can request a demo of RapidClaims to see how ML-driven review and coding intelligence work within real revenue cycle workflows.
FAQs
Q: What is the role of machine learning in medical coding and billing?
A: Machine learning helps by analyzing large volumes of clinical documentation and claims data to identify likely ICD-10, CPT or HCC codes, flag potential omissions, and estimate claim risk before submission.
Q: How does machine learning improve claims processing speed and accuracy?
A: By converting unstructured text into structured inputs, suggesting codes based on prior outcomes, and identifying documentation gaps, ML reduces manual review time and helps improve first-pass claim acceptance.
Q: Can machine learning tools fully replace medical coders and billers?
A: No. While ML handles many repetitive tasks and surfacing of issues, human coders and compliance teams remain essential for complex encounters, clinical nuance, and audit-ready validation.
Q: What are the main implementation risks of applying machine learning in revenue cycle operations?
A: Key risks include training on biased or low-quality data, lack of transparency in model recommendations, misalignment with payer rules, and inadequate documentation workflows.
Q: How can organizations measure whether machine learning is delivering value in coding and billing?
A: Organizations should track metrics like coder acceptance rate of ML suggestions, change in denial rate, coding turnaround time, variation across specialties, and audit correction frequency.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








