2026 ICD-10 Update: Correctly Coding Lower Back Pain (M54.5x)
Lower back pain (LBP) continues to be one of the most common reasons for clinical visits across the United States. A 2025 global burden review estimated 452.8 million people are affected by LBP worldwide, highlighting the scale of the condition and its impact on healthcare utilization.
For healthcare organizations, coders, and revenue cycle leaders, the challenge is not the volume of cases but the need for precise ICD 10 coding. Payer policies now expect a higher level of specificity, and inaccurate or outdated codes for lower back pain contribute to avoidable denials, compliance concerns, and delays in reimbursement.
Understanding how to correctly assign ICD 10 codes for lower back pain is essential for accurate documentation, cleaner claims, and audit ready workflows. This guide outlines the correct usage of the updated codes, the documentation needed to support them, and the implications for RCM and coding teams.
Key Takeaways
- Lower back pain ICD 10 coding relies on selecting the correct M54.5x code based on the level of detail documented in the encounter.
- M54.50 should be used only when the record lacks defining characteristics, while M54.51 and M54.59 apply when vertebrogenic or other specific patterns are documented.
- Coders must avoid combining lower back pain codes with diagnoses that already explain the symptoms, as this leads to claim edits and medical necessity issues.
- Clear documentation of objective findings, symptom context, and terminology consistency supports accurate code selection and reduces payer scrutiny.
- Implementing structured templates, embedded coding logic, and AI assisted coding tools such as RapidClaims helps ensure accuracy, reduce rework, and improve first pass claim acceptance.
- Regularly updating codes throughout the episode of care prevents denials tied to outdated or unsupported diagnoses.
Table of Contents:
- Overview of ICD-10 Coding for Lower Back Pain
- Understanding the Updated M54.5x Code Set
- How to Choose the Correct M54.5x Code
- Common Coding Errors and Denial Triggers
- Documentation Requirements for Accurate LBP Coding
- How M54.5x Codes Fit Into Clinical & Billing Workflows
- Examples of Correct ICD-10 Code Selection
- Conclusion
- FAQs
Overview of ICD-10 Coding for Lower Back Pain
ICD-10-CM provides the structure needed to classify lower back pain with greater accuracy and clinical relevance. It supports detailed reporting, strengthens medical necessity justification, and helps ensure correct reimbursement for conditions with varied etiologies.
- ICD-10-CM expands diagnostic detail compared to ICD-9.
- Lower back pain falls under the M54.5x category.
- Codes in this family reflect different levels of specificity based on documentation.
- Accurate assignment helps avoid denials tied to vague or incomplete coding.
Why the M54.5 Code Was Updated
Lower back pain coding shifted significantly when CMS retired the broad M54.5 code. This change addressed long-standing concerns that the old code lacked diagnostic specificity and contributed to ambiguous, unsupported claims.
- M54.5 was historically overused for nearly all lumbar pain presentations.
- APTA and other groups reported inconsistent documentation and limited clinical clarity under the old code.
- Payers often challenged claims due to insufficient detail or lack of alignment with clinical findings.
- The update aimed to improve accuracy, reduce misuse, and support clearer differentiation of pain types.
Understanding the M54.5x Code Set
The 2021 update introduced three distinct codes to better represent the documented cause or characteristics of lower back pain. Coders must now select the most precise option supported in the clinical record.
- M54.50 — Low back pain, unspecified
- M54.51 — Vertebrogenic low back pain
- M54.59 — Other low back pain
- Using outdated or non-specific codes increases the likelihood of edits, denials, and compliance scrutiny.
Understanding the Updated M54.5x Code Set
The M54.5x category includes the three active ICD-10-CM codes used to classify lower back pain with the level of specificity supported in the clinical record. Coders are expected to choose the code that best reflects the documented pain characteristics rather than defaulting to general pain categories.
- M54.50 – Low back pain, unspecified: Used only when no descriptive detail or defined etiology is documented.
- M54.51 – Vertebrogenic low back pain: Assigned when vertebrogenic features are documented, typically supported by exam findings or imaging.
- M54.59 – Other low back pain: Used when lower back pain is described clearly but does not meet vertebrogenic criteria, such as mechanical or muscular patterns.
Related Diagnoses That Replace M54.5x
When a separate condition fully explains the lumbar pain, coding guidelines require assigning the underlying diagnosis instead of an M54.5x code. This ensures the claim reflects the true source of symptoms and aligns with payer expectations.
- M51 series: Disc degeneration or herniation
- M54.16: Lumbar radiculopathy
- M54.3x: Sciatica
- S39.012: Lumbar strain
- M48.06: Lumbar spinal stenosis
If you'd like, I can format the next section the same way for consistency.
How to Choose the Correct M54.5x Code
Coding guides often focus on how to match the level of diagnostic detail in the record with the correct M54.5x code. The decision depends on what the provider has documented at that point in the clinical workflow. Coders are expected to capture the level of certainty, not assumptions about future findings.

When M54.50 Is Appropriate
Unspecified coding is acceptable only when the medical record lacks enough detail to assign a more precise diagnosis. This situation often occurs early in the clinical assessment before the provider has completed evaluation or ordered diagnostic studies. Coding resources caution that M54.50 should not be used once the record includes descriptors that point to a defined pain source.
Common scenarios for M54.50 include:
- The initial encounter where the cause of the pain is undetermined
- Documentation that describes lumbar pain without qualifiers
- Situations where the provider plans further evaluation before determining etiology
When to Assign M54.51
Many clinical coding blogs emphasize that this code should be used only when the provider identifies vertebrogenic origin. This determination is based on documented evidence such as findings from physical examination or imaging. The documentation must clearly describe features associated with vertebrogenic pain rather than general lumbar discomfort.
Indicators that support M54.51 include:
- Provider documentation of vertebral endplate changes
- Imaging studies showing Modic-type findings
- Description of pain patterns consistent with vertebrogenic etiology
When to Use M54.59
This code is often discussed in coding references as the midpoint between unspecified and vertebrogenic diagnoses. It applies when lower back pain is described with some clinical detail but does not meet vertebrogenic criteria. It is frequently used in physical therapy, musculoskeletal clinics, and primary care settings where the provider identifies a defined but nonspecific pain pattern.
Common documentation cues for M54.59:
- Mechanical low back pain
- Muscular or soft tissue related pain
- Pain that is defined but not linked to vertebrogenic changes
Common Coding Errors and Denial Triggers
Lower back pain claims are often denied when the selected ICD-10 code does not match the level of detail documented or when coding patterns conflict with payer expectations. The issues below represent the most frequent reasons LBP claims are flagged during review.
- Using unspecified codes despite documented detail: Occurs when M54.50 is assigned even though the record supports a more specific code such as M54.51 or M54.59.
- Combining general LBP codes with structural diagnoses: Edits are triggered when M54.50 or M54.59 is paired with disc disorders, radiculopathy, or sciatica that already explain the pain.
- Missing required characters or specificity elements: Denials arise when laterality, fifth/sixth characters, or complete code extensions are omitted.
- Diagnosis not supporting billed services: Particularly common in PT, rehab, and chronic pain programs when the documented condition does not clearly justify the services provided or the treatment intensity.
Documentation Requirements for Accurate LBP Coding
High-quality documentation is essential for assigning accurate lower back pain codes and supporting clean claim submission. Coding references emphasize that payers look for consistency, clarity, and measurable details when reviewing LBP-related encounters. These best practices help coders select the correct M54.5x code and ensure that the diagnosis aligns with the services delivered.

Capture Objective Findings Clearly
Documentation should include measurable or observable elements that support the diagnosis. Clear descriptors help coders determine the correct level of specificity and allow payers to validate clinical reasoning.
Examples of objective details that support accurate coding:
- Functional impact (difficulty bending, lifting, or standing)
- Neurologic signs when present
- Range of motion or mobility limitations
Use Consistent Terminology Across Notes
Coding resources often stress that the terminology used in the encounter note should match the terminology used in related documentation such as therapy evaluations, follow up visits, or imaging summaries. Consistency helps avoid conflicts during claim review.
Examples of terminology alignment:
- Using the same pain descriptors across encounters
- Ensuring exam findings and diagnostic impressions use compatible terms
Include Duration and Basic Clinical Context
Duration supports code accuracy and medical necessity review. While it does not determine the specific M54.5x code, many payer policies expect timeframe references when reviewing treatment progress and follow up care.
Elements often recommended in coding guidance:
- Whether symptoms are acute, subacute, or chronic
- Whether pain is stable, improving, or worsening
Connect Documentation to the Plan of Care
Several clinical billing resources emphasize the importance of showing how the diagnosis supports the services performed. This connection allows reviewers to verify medical necessity and expected treatment trajectory.
Examples that strengthen this linkage:
- Describing how pain affects function addressed by therapy
- Identifying factors that justify imaging, medication, or specialist referral
How M54.5x Codes Fit Into Clinical & Billing Workflows
Effective ICD 10 coding for lower back pain depends on workflows that support accurate documentation, timely code selection, and consistent review before claims move downstream. Many healthcare organizations rely on a combination of EHR templates, coding guidelines, and automated validation tools to standardize this process. The goal is to reduce manual coding burden, minimize rework, and improve first-pass acceptance rates.
Integrating Structured Documentation in the EHR
Structured fields for pain characteristics, exam findings, and clinical context help ensure the information coders need is captured during the encounter. EHR templates often include prompts for functional impact, symptom duration, and relevant objective findings, which makes downstream coding more consistent.
Embedding Coding Logic Into Daily Workflows
Many RCM teams use coding rules or checkpoints inside the EHR to alert clinicians or coders when documentation does not support the selected LBP code. These prompts help prevent errors such as selecting a code that does not match the documented detail or overlooking a more specific option.
Using AI Assisted Coding Tools to Support Accuracy
Platforms like RapidClaims help automate the review process by analyzing clinical documentation and identifying the ICD 10 codes supported by the text. The system can:
- Detect when documentation points to a more specific M54.5x code
- Flag conflicting code combinations
- Identify missing elements that may affect medical necessity
- Apply the latest ICD 10 CM updates without manual intervention
This level of automation supports coders by ensuring that claims align with payer expectations and reduces the need for post submission edits.
Strengthening Pre Submission Validation
Before claims are released, many organizations run automated checks to confirm that diagnosis codes match the documented encounter, the services provided, and payer policy requirements. RapidClaims supports this process by validating code selection, highlighting inconsistencies, and reducing avoidable denials caused by unsupported documentation.
Unlock cleaner claims and higher coding accuracy with AI-assisted workflows.
RapidCode and RapidScrub help RCM teams apply the correct M54.5x codes, prevent denials, and maintain payer-compliant documentation. Request your tailored coding accuracy assessment.
Examples of Correct ICD-10 Code Selection
The following examples illustrate how coders apply the appropriate M54.5x code based on the details documented in the encounter. Each scenario reflects patterns commonly discussed in coding references and helps clarify how specificity is determined in practical situations.
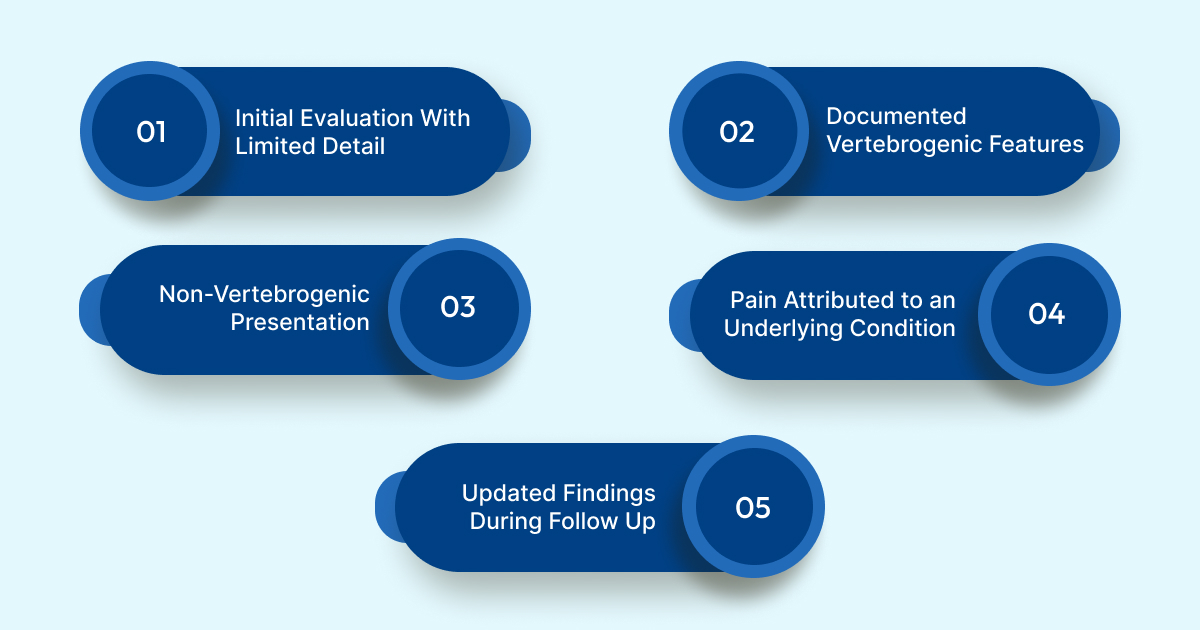
Example 1: Initial Evaluation With Limited Detail
A patient reports lower back discomfort without descriptive qualifiers. The provider documents general lumbar pain and plans further assessment at a follow up visit.
Appropriate code: M54.50
Example 2: Documented Vertebrogenic Features
The encounter note includes findings consistent with vertebrogenic origin, supported by imaging that describes endplate changes.
Appropriate code: M54.51
Example 3: Defined but Non Vertebrogenic Presentation
The provider documents mechanical lumbar pain with no evidence of vertebrogenic involvement. The findings describe a reproducible musculoskeletal pattern.
Appropriate code: M54.59
Example 4: Pain Attributed to an Underlying Condition
The encounter indicates that lumbar pain is due to disc degeneration confirmed by imaging. Coding guidelines instruct coders to assign the diagnosis representing the underlying pathology instead of an M54.5x code.
Appropriate code: A disc-related code from the M51 series
Example 5: Updated Findings During Follow Up
A patient initially assessed with M54.50 returns with new documentation showing a more defined pain source. The coder updates the diagnosis to reflect the new level of specificity.
Appropriate code: M54.51 or M54.59 based on the new findings
Conclusion
Accurate ICD 10 coding for lower back pain depends on aligning documentation with the most specific code supported in the clinical record. Consistent terminology, clear objective findings, and up to date coding workflows allow RCM and coding teams to reduce denials and maintain compliance with current payer expectations. As coding requirements continue to evolve, organizations benefit from tools that can validate documentation, surface the correct code options, and streamline review before claim submission.
RapidClaims supports these goals by analyzing encounter documentation, identifying supported ICD 10 CM codes, and flagging discrepancies that could lead to rework or denials. The platform helps teams maintain accuracy across high volume conditions like lower back pain while keeping pace with annual code updates.
To explore how RapidClaims can strengthen coding accuracy and improve clean claim rates, request a demo and see how the platform fits within your workflows.
FAQs
Q: What is the ICD 10 code for lower back pain?
A: The ICD 10 CM code category for lower back pain is M54.5x, which includes M54.50, M54.51, and M54.59. The correct code depends on how clearly the provider defines the pain source in the documentation.
Q: What is the difference between M54.50 and M54.51?
A: M54.50 is used when lower back pain is documented without a defined cause. M54.51 is used only when vertebrogenic origin is clearly supported by clinical findings or imaging.
Q: What is the difference between F43.8 and F43.89?
A: Both codes describe stress-related conditions, not lower back pain. F43.8 captures other reactions to severe stress, while F43.89 includes other specified stress and adjustment disorders.
Q: What is low back pain unspecified?
A: Low back pain unspecified refers to lumbar pain without documented descriptors or identified etiology. It is coded as M54.50.
Q: What is another name for lower back pain?
A: Lower back pain is also called lumbago or lumbar pain in clinical settings.
Q: What is the cause of lower back pain?
A: Lower back pain can result from muscle strain, mechanical dysfunction, vertebral changes, disc issues, or nerve irritation. Identifying the cause helps determine whether an M54.5x code or a more specific diagnosis should be used.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








