ICD-10 Code for Telehealth Visit: 2025 Guide for Providers

Imagine receiving expert medical care without leaving your home; telehealth makes it possible. Today, virtual consultations enable timely evaluation, accurate diagnosis, and effective management from anywhere. CMS is expanding coverage and reimbursement for telehealth visits, giving patients nationwide convenient and safe access to care.
As of July 2025, CMS extended the suspension of telehealth frequency limitations on subsequent inpatient and nursing facility visits through the end of the year. This move reflects the ongoing commitment to supporting telehealth services.
In this blog, you'll explore the ICD-10 code for telehealth visits, covering correct coding practices, compliance guidance, and tips for accurate reimbursement in 2025.
TL;DR (Key Takeaways)
- Telehealth coding challenges include shifting regulations, payer inconsistencies, and documentation errors.
- Using correct modifiers (e.g., -95, -GT) ensures compliance and accurate reimbursement for telehealth services.
- Coders must document patient location, technology used, and encounter details to avoid denials.
- Following structured best practices reduces audit risks and maintains revenue integrity.
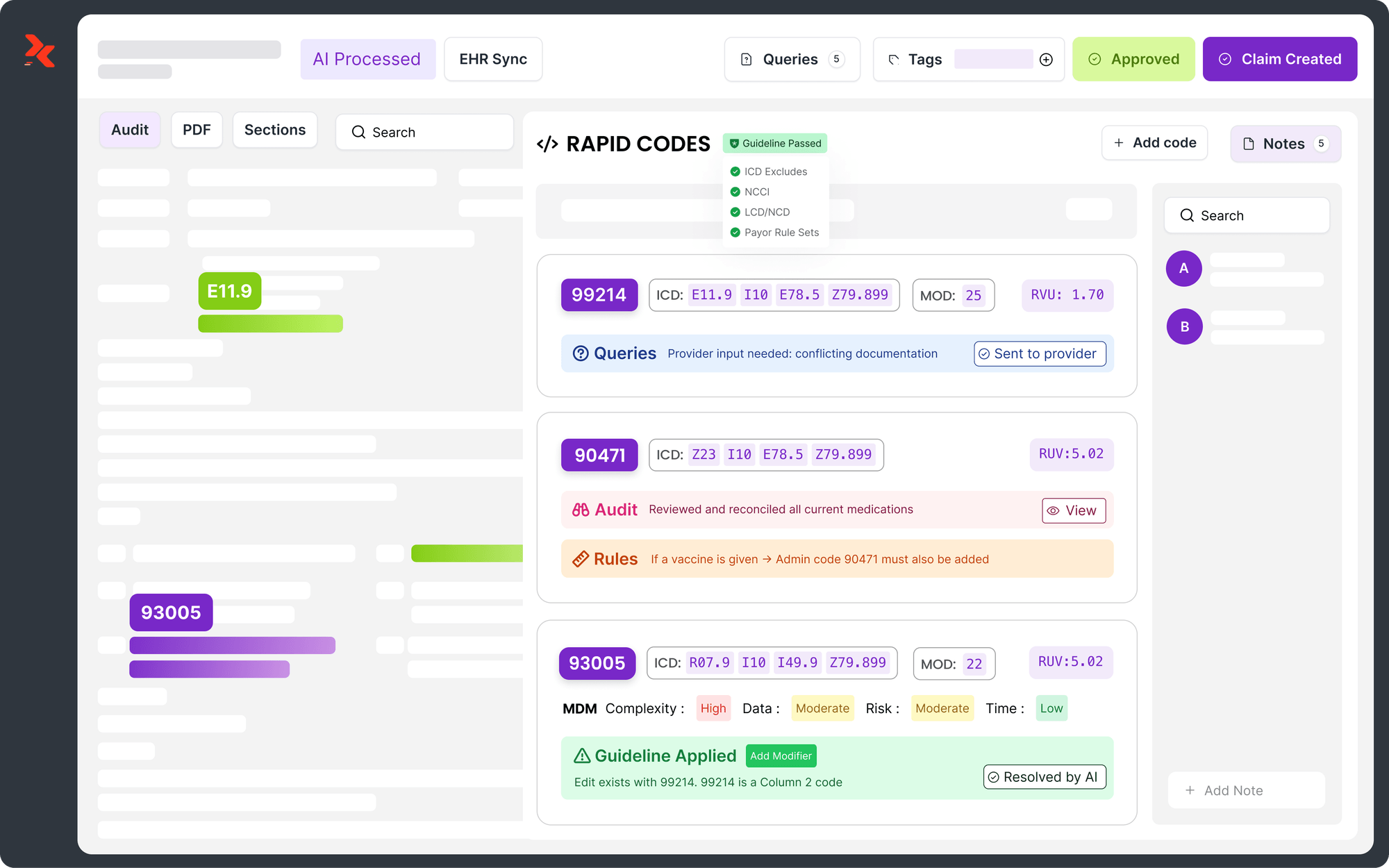
- AI-powered platforms like RapidClaims automate compliance, increase accuracy, and improve reimbursement efficiency.
Table of Contents:
- What Is an ICD-10 Code for a Telehealth Visit?
- Key Considerations for Telehealth Coding in 2025
- Commonly Used ICD-10 Codes for Telehealth Visits
- Telehealth Coding Challenges That Impact Reimbursement
- Best Practices for Accurate Telehealth Coding
- Conclusion
- Frequently Asked Questions (FAQs)
What is an ICD-10 Code for a Telehealth Visit?
An ICD-10 code for a telehealth visit is the diagnostic code used to document the patient’s condition. It also indicates the reason for the visit when care is provided virtually. These codes are identical to those used for in-person visits. However, they must be paired with the appropriate telehealth modifiers or place-of-service codes to indicate that the service was delivered remotely. Proper use ensures accurate documentation, compliance with payer requirements, and correct reimbursement for telehealth services.
Key Considerations for Telehealth Coding in 2025
Accurate telehealth coding is essential to ensure compliance, proper reimbursement, and streamlined claims processing. Providers must stay updated on CMS guidance, use the correct modifiers, and document visits thoroughly to support medical necessity.
Below are some critical factors to keep in mind when coding telehealth visits in 2025:
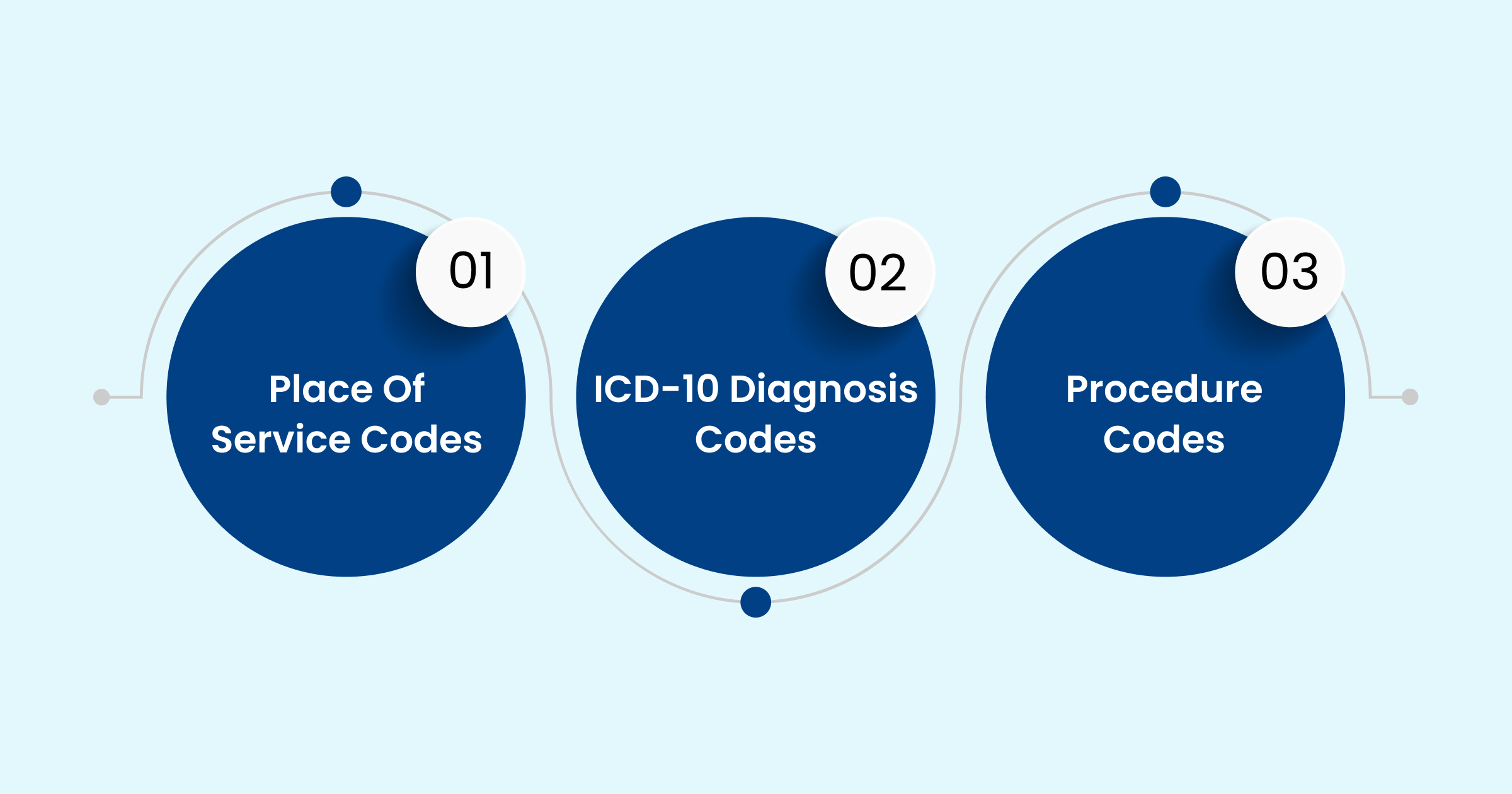
1. Place of Service (POS) Codes
For telehealth visits, the POS code indicates where the service was provided. In 2025, CMS continues to require the use of specific POS codes to differentiate between in-person and telehealth services.
Example: POS code 02 - This code is used when health services are delivered via telecommunication technology and the patient is not located in their home during the visit.
2. ICD-10 Diagnosis Codes
The choice of ICD-10 diagnosis codes for telehealth visits should accurately reflect the patient's condition and the reason for the encounter. CMS provides a list of valid ICD-10 codes that support medical necessity for telehealth services, which should be consulted to ensure compliance.
3. Procedure Codes (CPT/HCPCS)
Telehealth services are billed using specific procedure codes, such as CPT codes for telehealth consultations. It's crucial to use the correct codes to avoid claim denials and ensure proper reimbursement. CMS provides guidance on the appropriate use of these codes for telehealth services.
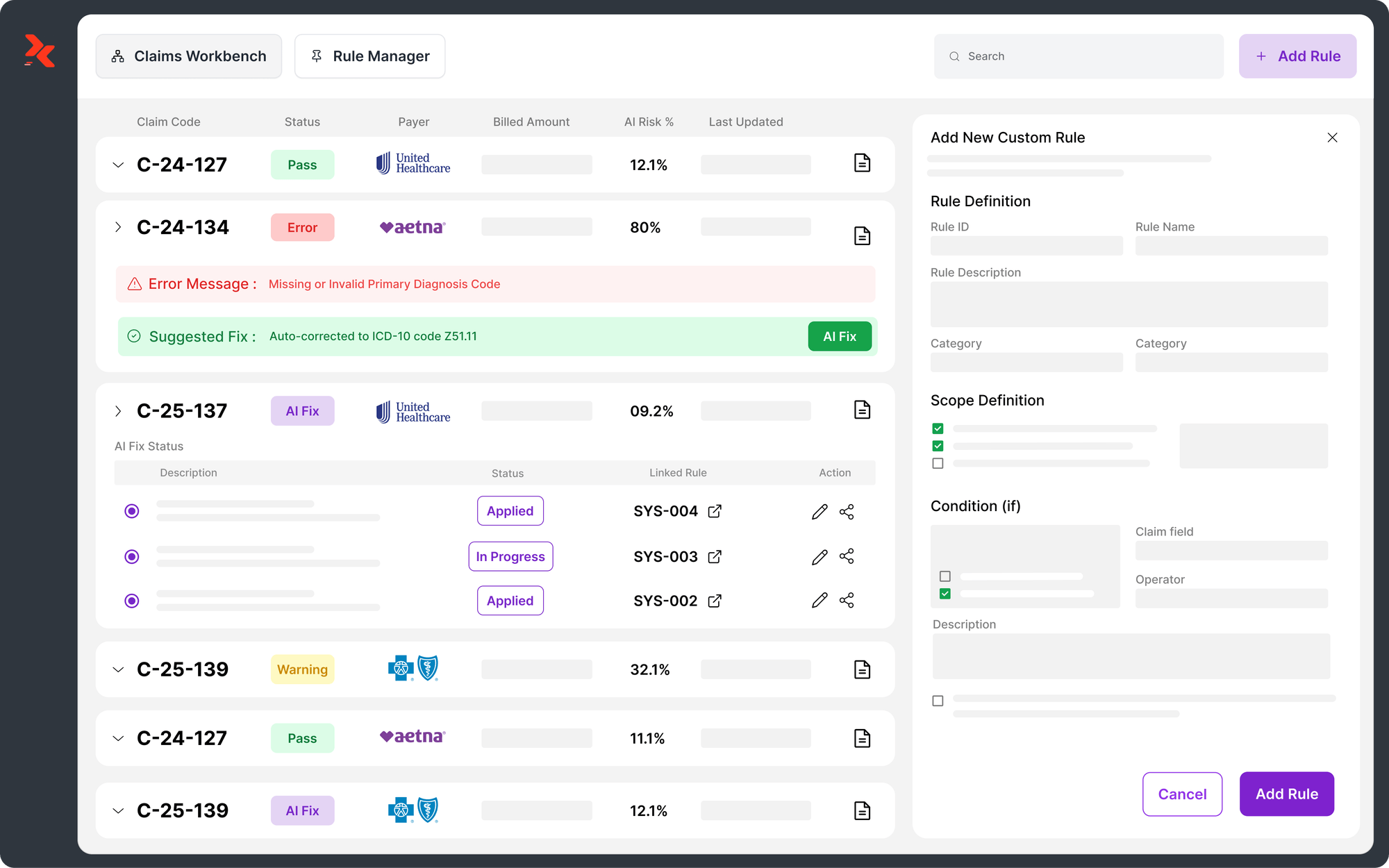
Even with clear guidelines, manual coding often leads to errors, denials, and delayed revenue cycles. RapidClaims addresses these challenges by utilizing AI-driven automation to assign accurate ICD-10, CPT, and HCC codes in real-time. This approach reduces administrative costs, improves claim acceptance rates, and ensures ongoing compliance with CMS and payer requirements.
Let’s now look at some of the most commonly used ICD-10 codes for telehealth visits, which help ensure accurate documentation and compliant billing.
Commonly Used ICD-10 Codes for Telehealth Visits

Selecting the appropriate ICD-10 code is crucial for accurate billing and reimbursement of telehealth services. While the specific code depends on the patient's condition, several codes are frequently used for routine check-ups and administrative purposes.
1. Z00.00 - Adult Medical Exam Without Abnormal Findings
This code is used for a general adult medical examination where no abnormal findings are reported. It's applicable when a patient undergoes a routine health check-up without any identified issues. However, it's important to note that this code should not be combined with administrative exams (Z02), special screenings (Z11-Z13), or pre-procedural exams (Z01.81) due to exclusions.
2. Z00.01 - Adult Medical Examination With Abnormal Findings
This code applies when a general adult medical examination reveals abnormal findings. It's used to document routine health check-ups where issues are identified that may require further investigation or intervention. As with Z00.00, it's essential to avoid combining this code with administrative or special screening examination codes to ensure compliance.
3. Z01.419 - Gynecological Examination Without Abnormal Findings
This code is used for routine gynecological examinations where no abnormal findings are identified. It is commonly applied for preventive care visits, such as annual exams. Importantly, Z01.419 should not be reported with general adult medical examination codes (Z00.00 or Z00.01) when performed by an OB/GYN. Some payers, however, may allow reimbursement for two separate annual visits if an OB/GYN conducts one.
4. Z02.89 - Other Administrative Examinations
This code is used for administrative examinations that don't fall under other specific categories. It's applicable for services like pre-employment physicals or other non-medical evaluations. However, it should not be used for general health check-ups or gynecological exams, as those have their designated codes (Z00.00, Z00.01, Z01.419).
These ICD-10 codes are frequently used for routine check-ups and administrative purposes in telehealth. However, accuracy is critical to avoid denials and ensure compliance. RapidClaims uses AI and NLP to detect documentation gaps, suggest compliant ICD-10 codes, and reduce claim denials. The platform also leaves a full audit trail, ensuring compliance with CMS, HIPAA, and payer-specific requirements.
Also Read: 2025 Telehealth Updates: Key E/M Code Changes & Medicare Policies
Telehealth Coding Challenges That Impact Reimbursement
Despite broader adoption and supportive regulations, telehealth coding in 2025 still poses significant hurdles for providers. The following persistent challenges often disrupt accurate claim submission and directly impact reimbursement outcomes:
- Evolving Regulations: CMS and commercial payer rules change frequently, requiring coders to update workflows or risk noncompliant claims.
- Technology Barriers: Patients without video capability often default to audio-only visits, requiring different coding and modifier use.
- Reimbursement Inconsistencies: Medicare reimburses video and audio-only visits differently, while some private payers restrict coverage, causing underpayments.
- Modifier Confusion: Misuse of modifiers -95 (synchronous telehealth), -FQ (audio-only), or -FR (video) is a leading cause of telehealth claim denials.
- Place of Service Errors: Reporting POS 02 instead of POS 10 (the patient’s home) often results in reduced reimbursement.
- Documentation Gaps: Missing records of patient consent, encounter modality, or provider location can lead to post-payment audits.
- State Variation: For multi-state providers, differences in Medicaid telehealth rules create added administrative overhead.
Understanding these challenges makes it clear why best practices are essential; let’s examine how to ensure accurate, compliant, and efficient telehealth coding.
Best Practices for Accurate Telehealth Coding
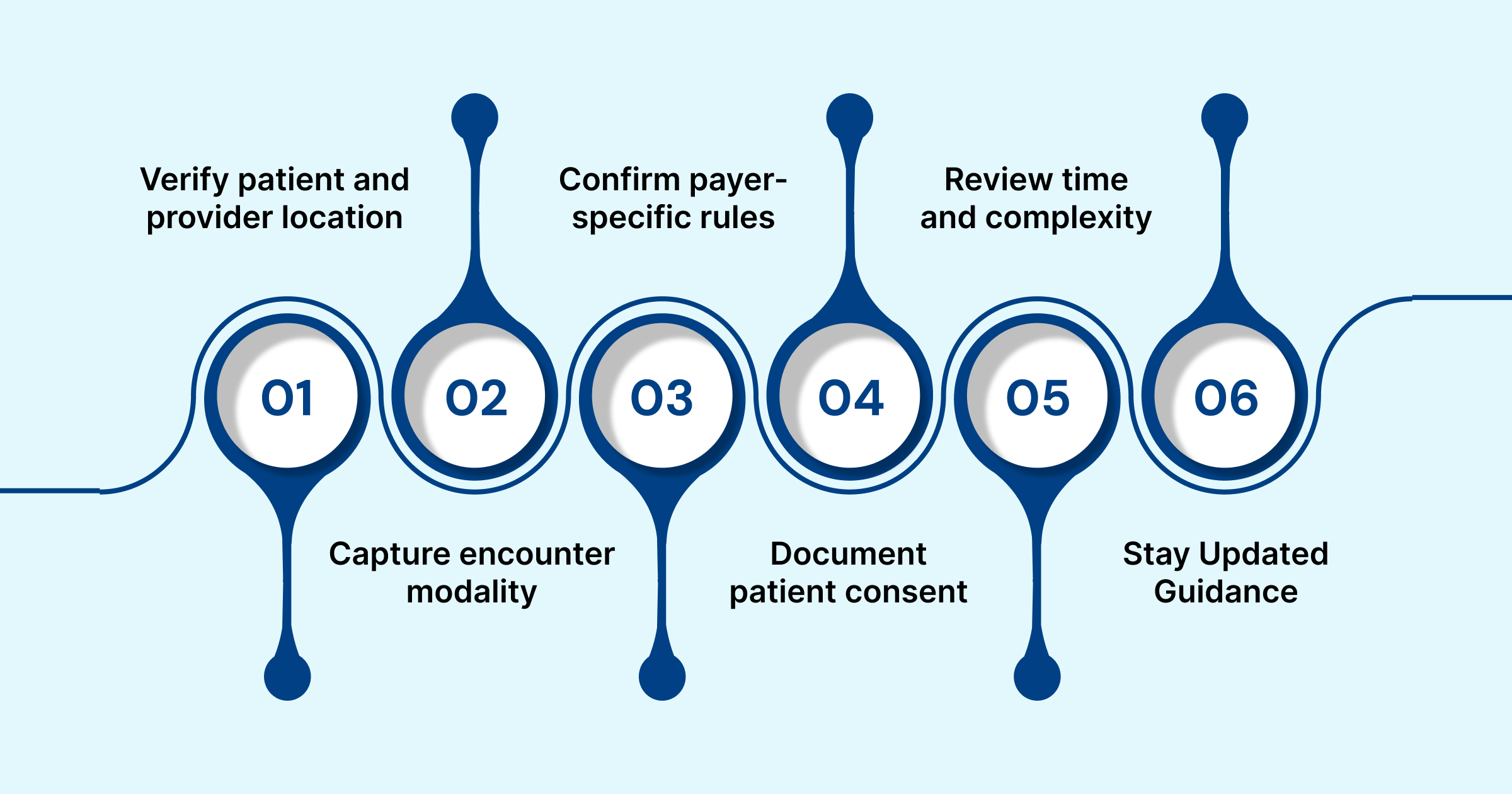
Accurate telehealth coding is critical for both compliance and reimbursement. To reduce denials and audit risks, coders and billing teams should follow structured best practices that address documentation, modifiers, payer rules, and encounter details.
Below are key practices every organization should implement to ensure accuracy and consistency in telehealth coding:
- Verify patient and provider location: Confirm whether the patient is at home (POS 10) or another site (POS 02) and document the provider’s location, as both impact reimbursement.
- Capture encounter modality: Specify whether the visit was synchronous video, audio-only, or asynchronous (store-and-forward) to guide correct CPT/HCPCS coding.
- Confirm payer-specific rules: Differentiate between Medicare, Medicaid, and commercial payer policies, which often vary in covered codes and documentation needs.
- Document patient consent: Record verbal or written consent for telehealth services in the medical record to satisfy CMS and state requirements.
- Review time and complexity: Ensure time-based E/M coding reflects the actual duration and medical decision-making complexity of the telehealth encounter.
- Stay updated with CMS and payer guidance: Telehealth coverage rules, code lists, and frequency limits are frequently updated; therefore, coders should regularly monitor CMS telehealth lists and payer bulletins.
Conclusion
Manual coding errors, changing telehealth policies, and payer-specific requirements continue to challenge compliance for healthcare practices. Selecting and applying the correct ICD-10 Code for a Telehealth Visit is essential. Without it, providers face higher denial rates, revenue leakage, and increased audit risks that can harm both financial stability and patient care.
With AI-powered solutions from RapidClaims, providers can simplify telehealth coding, reduce errors, and ensure faster reimbursements. RapidClaims automates documentation checks, applies correct modifiers, and keeps pace with regulatory updates, making coding more efficient and audit-ready.
Ready to minimize denials and maximize reimbursements? Request a Free Demo with RapidClaims today to streamline your coding workflows and strengthen your revenue cycle.
Frequently Asked Questions (FAQs)
1. How do I know if my payer covers a specific telehealth service?
A. You should always verify payer-specific telehealth policies before billing. Coverage varies between Medicare, Medicaid, and commercial insurers. Reviewing updated payer guidelines helps avoid denials.
2. Can I bill telehealth visits if my patient only uses audio calls?
A. Yes, many payers reimburse for audio-only services, but coverage differs. You must document the communication method and confirm payer rules. Some may limit reimbursement to video visits only.
3. What happens if I use the wrong telehealth modifier?
A. Using the wrong modifier can cause immediate claim denials or underpayment. It also increases audit risks since modifiers validate the service method. Regular training helps coders avoid these mistakes.
4. How often should I update my telehealth coding guidelines?
A. Telehealth rules change frequently, so guidelines should be updated at least quarterly. Monitoring CMS and payer policy changes ensures compliance and prevents outdated coding practices.
5. If I code telehealth incorrectly, can I resubmit the claim?
A. Yes, most payers allow corrected claim submissions. However, delays in resubmission can impact cash flow. Promptly identifying errors and resubmitting with accurate codes improves revenue recovery.

Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products
%201.png)

.jpg)