Difference Between Inpatient and Outpatient Coding

Coding accuracy has become a critical priority for healthcare organizations. Higher chart volumes, shifting CMS rules and increased audit scrutiny place new pressure on coding teams every year. CMS reported a Medicare improper payment rate of 5.61 percent in 2023, highlighting ongoing issues tied to documentation and coding accuracy.
Understanding the difference between inpatient and outpatient coding is essential for managing these risks. Each setting uses different code systems, documentation requirements and payment models. Inpatient encounters rely on precise diagnosis sequencing and MS DRG validation. Outpatient visits require accurate CPT and HCPCS assignment along with correct modifier use.
These distinctions influence denial patterns, audit exposure and coder workload. Clear awareness of how the two environments differ helps RCM leaders strengthen compliance, improve reimbursement accuracy and maintain consistent performance across their coding operations.
Key Takeaways
- Inpatient and outpatient coding differ in code sets, documentation needs, payment models, and audit exposure.
- Inpatient coding focuses on diagnosis sequencing, ICD-10-PCS specificity, and MS DRG accuracy, all driven by detailed multi-provider records.
- Outpatient coding centers on CPT and HCPCS assignment, correct modifier use, and medical necessity alignment for same-day services.
- Denial risks vary: inpatient claims face sequencing and clinical validation issues, while outpatient claims often encounter CPT errors, modifier conflicts, and bundling edits.
- Strong documentation, consistent rule application, and clear workflow design are essential to maintain accuracy across both coding environments.
Table of Contents:
- What Is Inpatient Coding?
- What Is Outpatient Coding?
- Key Differences Between Inpatient and Outpatient Coding
- Challenges That Affect Inpatient and Outpatient Coding Accuracy
- How to Improve Accuracy in Inpatient and Outpatient Coding
- Conclusion
- FAQs
What Is Inpatient Coding?
Inpatient coding reflects the full scope of diagnoses and procedures documented during a patient’s hospital stay. Coders apply ICD 10 CM for diagnoses and ICD 10 PCS for procedures, and these elements support the assignment of MS DRGs that determine hospital reimbursement under the Medicare Inpatient Prospective Payment System.
Inpatient encounters require coders to review a broad set of clinical documents, which often contain detailed and complex narratives. Key sources include:
- History and physical examinations
- Operative and procedure reports
- Progress notes and consultation notes
- Diagnostic imaging and laboratory results
- Discharge summaries
From these records, coders identify:
- The principal diagnosis that led to the admission
- Secondary diagnoses that meet reporting criteria
- Procedures that qualify for ICD 10 PCS reporting
- Complications or comorbidities that influence MS DRG assignment
Inpatient coding demands strong clinical interpretation skills and careful attention to sequencing rules. Documentation varies between providers and specialties, which increases complexity. Consistent accuracy in this environment supports compliant MS DRG outcomes, stable reimbursement and reduced audit risk.
What Is Outpatient Coding?
Outpatient coding captures the services provided during same day encounters such as clinic visits, diagnostic procedures, emergency department treatment and ambulatory surgeries. Coders use CPT and HCPCS Level II to report procedures and services, along with ICD 10 CM to document diagnoses that support medical necessity. These codes drive reimbursement through the Ambulatory Payment Classification system for Medicare outpatient services.
Outpatient encounters are shorter and more procedure focused than inpatient stays. Coders typically review:
- Provider evaluation and management notes
- Procedure and operative notes
- Diagnostic imaging and laboratory results
- Medication administration records
- Order sets and visit summaries
Key responsibilities in outpatient coding include:
- Selecting accurate CPT and HCPCS codes for all reportable services
- Applying correct modifiers to reflect laterality, repeat services or specific circumstances
- Assigning ICD 10 CM codes that support medical necessity and align with payer policies
- Ensuring documentation supports the service level, especially for evaluation and management visits
Outpatient settings require precise interpretation of procedure details, consistent understanding of modifier rules and close alignment with facility and payer billing guidelines. High accuracy helps reduce denials related to insufficient documentation, incorrect CPT assignment or invalid modifier use.
Key Differences Between Inpatient and Outpatient Coding
Inpatient and outpatient coding operate under different clinical, regulatory and payment requirements. These differences influence coding complexity, workflow design and denial risk. A clear comparison helps RCM leaders align staffing, documentation practices and quality review processes across both environments.
Strengthen inpatient and outpatient coding accuracy with AI-supported insights. Request a RapidClaims demo to see high-impact improvements in real workflows.
Challenges That Affect Inpatient and Outpatient Coding Accuracy
Coding operations face growing complexity across inpatient and outpatient settings. Differences in documentation patterns, payer rules and EHR workflows all influence accuracy, review speed and audit exposure.
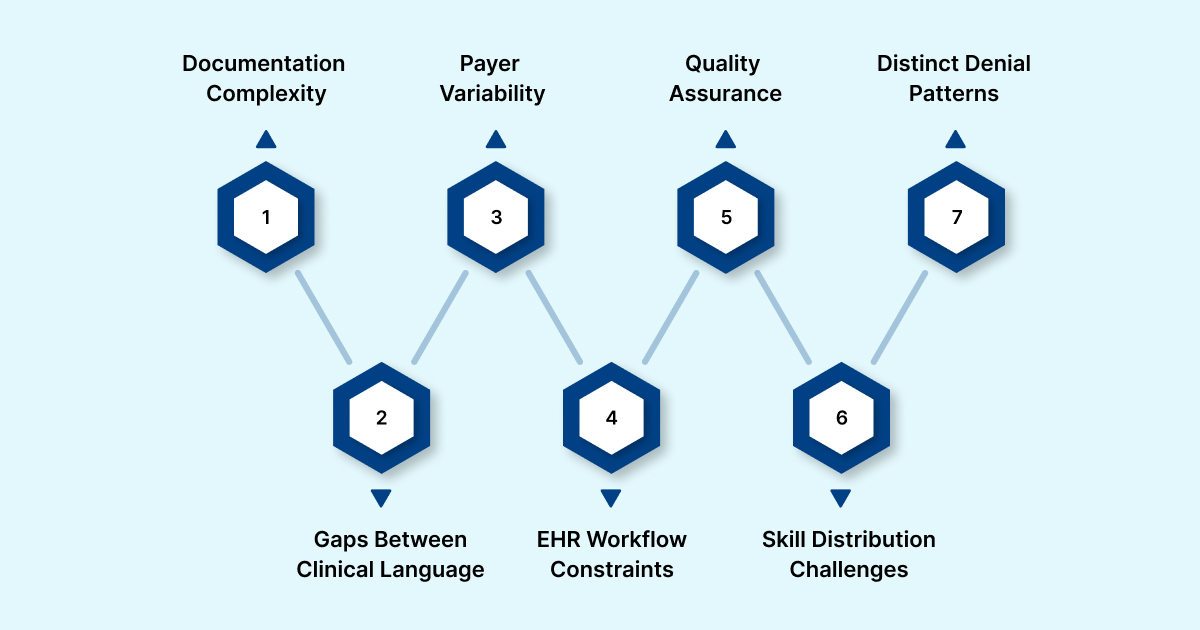
1. Increasing Documentation Complexity
Inpatient stays generate long, multi-specialty narratives with evolving diagnoses and procedure details. Outpatient encounters involve shorter notes but require precise coding of procedures, time based services and modifiers. Coders must interpret inconsistent terminology, varied provider styles and EHR templates that do not always align with coding rules.
2. Gaps Between Clinical Language and Coding Language
Coders regularly translate clinical phrasing into standardized coding terminology. In inpatient settings, this affects diagnosis specificity, sequencing and ICD 10 PCS elements such as approach and device. In outpatient settings, the challenge centers on exact CPT selection, appropriate modifiers and diagnosis codes that support medical necessity.
3. Payer Variability and Conflicting Requirements
Medicare, Medicaid and commercial payers differ in how they interpret coding rules. Inpatient claims may be questioned for secondary diagnoses that lack sufficient clinical validation. Outpatient claims are more likely to be denied due to bundling edits, modifier issues or authorization requirements. Teams must track these differences to avoid repeated denials.
4. EHR Workflow Constraints
EHR systems prioritize clinical documentation rather than coding efficiency. Inpatient reviewers often navigate multiple sections to confirm MCC or CC documentation, procedure details or discharge information. Outpatient details may be split across orders, procedure notes or ancillary reports. These workflows increase review time and risk of missed information.
5. Quality Assurance and Audit Demands
Inpatient QA requires verification of sequencing logic, DRG assignment and documentation sufficiency. Outpatient QA focuses on CPT accuracy, modifier use and compliance with payer medical necessity rules. Maintaining strong review processes across both areas requires significant time and specialized knowledge.
6. Workforce and Skill Distribution Challenges
Coder shortages continue across the industry. Inpatient work requires deep clinical understanding and ICD 10 PCS expertise. Outpatient coding demands precise CPT and modifier application. Many teams struggle to balance experience across both areas, which leads to inconsistent accuracy and variable turnaround times.
7. Distinct Denial Patterns That Require Targeted Strategies
Inpatient denials often stem from clinical validation issues, incorrect sequencing or insufficient documentation for MCC or CC capture. Outpatient denials commonly involve CPT errors, modifier issues, bundling edits and gaps in medical necessity. Effective mitigation requires monitoring denial trends separately for each setting.
How to Improve Accuracy in Inpatient and Outpatient Coding
Coding teams need precise interpretation of clinical documentation, consistent rule application and strong protection against denials. RapidClaims supports these needs across inpatient and outpatient settings through structured AI models, clear validation logic and seamless EHR integration.

1. RapidCode: Accurate Diagnosis and Procedure Capture
RapidCode reviews inpatient and outpatient documentation and identifies diagnoses, procedures and clinical indicators that support compliant code selection.
Key capabilities:
- Identification of principal and secondary diagnoses
- Extraction of ICD 10 PCS procedure elements for inpatient charts
- Accurate CPT and HCPCS prediction for outpatient encounters
- Alerts for missing details that affect MS DRG or APC outcomes
- Detection of mismatches between documentation and selected codes
RapidCode strengthens inpatient sequencing and DRG accuracy while supporting procedure specificity and modifier needs in outpatient visits.
2. RapidAssist: Real Time Coding Guidance in the EHR
RapidAssist provides coders with in-workflow suggestions based on the content of the clinical record.
Core functions:
- CPT and HCPCS recommendations tied to procedure notes and diagnostic results
- Modifier suggestions based on payer rules and clinical context
- Sequencing support for inpatient diagnoses
- Prompts when documentation does not support selected codes
This reduces manual searching, shortens review time and promotes consistent application of CMS guidelines.
3. RapidRecovery: Denial Recovery Aligned to Inpatient and Outpatient Coding
Denial management requires different strategies for inpatient and outpatient claims due to differences in payment models, documentation depth, and audit focus.
RapidRecovery supports post submission recovery by applying AI driven prioritization and structured appeal workflows.
Key benefits include:
- Identification of recoverable inpatient denials related to sequencing, clinical validation, and MS DRG disputes
- Prioritization of outpatient denials driven by CPT errors, modifier conflicts, bundling edits, or medical necessity challenges
- Support for appeal documentation alignment based on payer specific requirements
- Feedback of denial insights into upstream coding and documentation improvement efforts
By addressing denials after they occur and feeding intelligence back into prevention workflows, RapidRecovery helps organizations reduce revenue leakage and stabilize reimbursement across both inpatient and outpatient services.
4. Enterprise Integration for Scalable Coding Operations
RapidClaims connects with EHRs using FHIR and HL7 standards, giving coders unified access to encounter data without changing workflows.
Integration benefits:
- Centralized review of inpatient and outpatient charts
- Dashboards for quality assurance and audit preparation
- Rules tailored to facility policies and payer specific requirements
- Transparent coding rationales for compliance teams
This creates a more consistent and efficient coding ecosystem across service lines.
5. Denial Prevention Aligned to Each Setting
RapidClaims supports prevention strategies based on the unique denial patterns of inpatient and outpatient claims.
- Inpatient: sequencing validation, accurate MCC and CC capture, complete procedure detail
- Outpatient: CPT accuracy, correct modifiers, bundling edit prevention and medical necessity alignment
This reduces rework, improves reimbursement and supports steady RCM performance.
Improve documentation clarity, coding precision, and denial prevention across inpatient and outpatient settings. Connect with RapidClaims for a tailored demonstration.
Conclusion
Improving coding performance today requires more than familiarity with individual code sets. It depends on how well organizations coordinate workflows, support coders with reliable information, and maintain consistency across very different clinical environments. Strong operational foundations allow teams to handle rising documentation demands while keeping compliance and reimbursement stable.
For leaders evaluating tools that can strengthen these workflows, request a demo of RapidClaims to explore how AI supported coding can fit into your organization’s broader revenue cycle strategy.
FAQs
Q: What is the main difference between inpatient and outpatient coding?
A: Inpatient coding is based on ICD 10 CM and ICD 10 PCS and supports MS DRG assignment for full hospital stays. Outpatient coding uses CPT, HCPCS and ICD 10 CM to capture procedures and diagnoses for same day encounters.
Q: Why does sequencing matter more in inpatient coding?
A: Sequencing determines the principal diagnosis and affects MS DRG assignment. Incorrect sequencing can alter reimbursement, trigger audits or cause clinical validation denials.
Q: Why are modifiers important in outpatient coding?
A: Modifiers clarify circumstances such as laterality, repeat procedures or bundled services. Incorrect or missing modifiers contribute to a large share of outpatient claim denials.
Q: How do denial patterns differ between inpatient and outpatient claims?
A: Inpatient denials often relate to insufficient documentation for MCC or CC capture, clinical validation issues or incomplete procedure detail. Outpatient denials typically involve CPT errors, modifier issues, bundling edits or medical necessity conflicts.
Q: Does outpatient coding require the same level of documentation depth as inpatient coding?
A: Outpatient documentation is generally shorter but must be precise. Procedure details, time based services and clear clinical indications are essential for accurate CPT and HCPCS coding.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








