Improving DRG Assignment with AI: The Future of Inpatient Coding

For many hospitals and clinics, DRG assignment is a constant source of stress. Coders spend hours combing through patient charts, juggling multiple diagnoses, procedures, and treatments, all while ensuring compliance with ever-changing regulations. One small error can result in underpayment, overpayment, or costly claim denials, affecting both the healthcare center’s revenue and the patient’s care experience.
The stakes are high, and the traditional manual approach simply can’t keep up with the growing volume and complexity of inpatient data. That’s where DRG coding automation comes in. Advanced AI and deep learning models are now capable of analyzing patient records, predicting DRGs, and achieving accuracy rates of 95% and above.
In this blog, we’ll explore how AI is transforming DRG assignment, why it matters for inpatient facilities and coders, and how automation can save time, reduce errors, and secure accurate reimbursements.
Key Takeaways:
- Challenge of Manual DRG Coding: Coding by hand is complex, error-prone, and constantly affected by changing regulations, which can slow revenue and affect compliance.
- Core AI Functionality: AI-driven DRG coding automates code assignment, pre-submission claim review, real-time error detection, and workflow management to reduce mistakes and speed up claims.
- Primary Benefits: Clinical Documentation Improvement ensures the accuracy and completeness of patient records, supporting correct DRG assignment and proper reimbursement.
- Evolving Coder Role: The hybrid model shifts coders’ focus from routine tasks to handling complex or ambiguous cases that require human judgment.
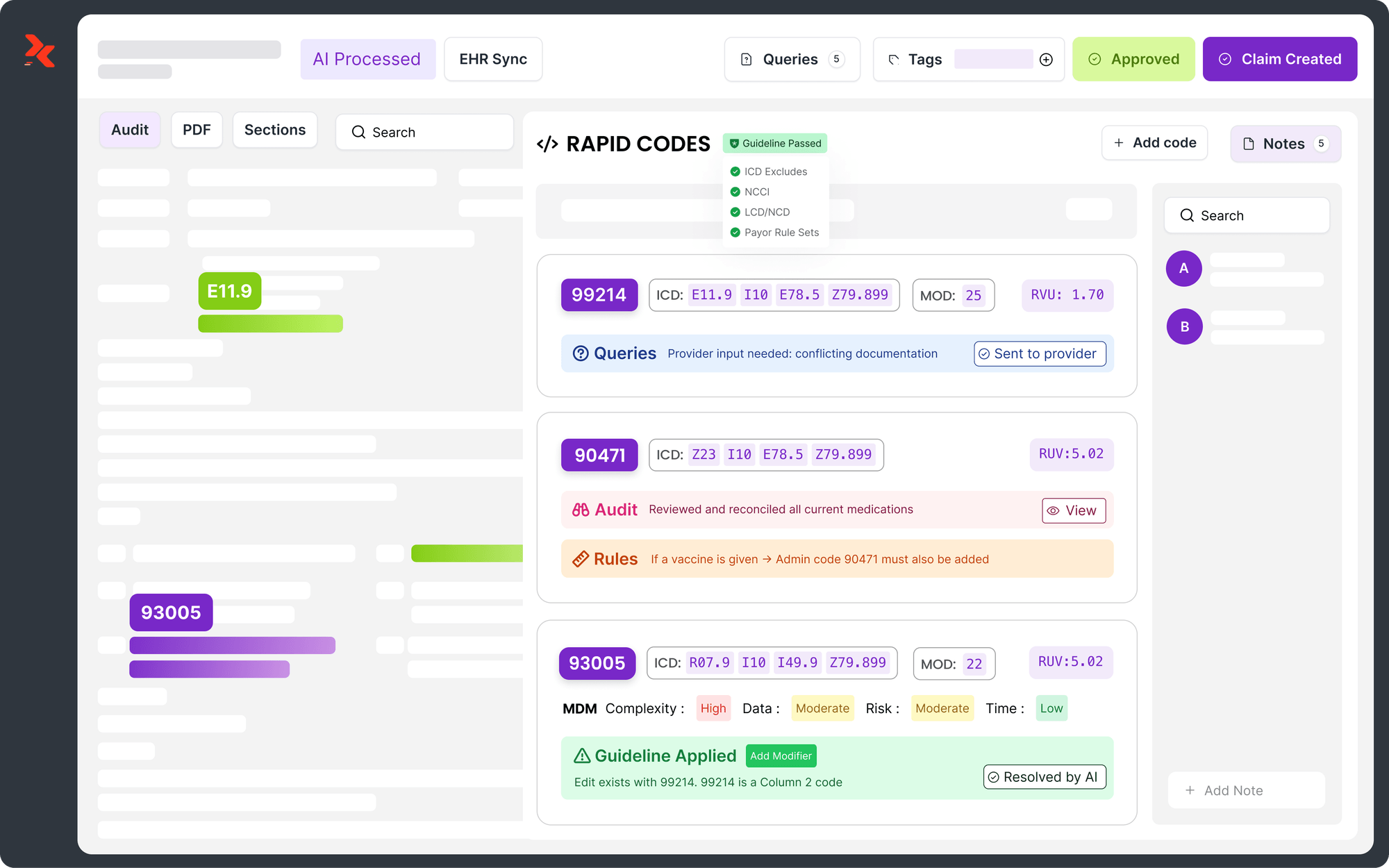
- A Collaborative Tool: Platforms like RapidClaims combine AI efficiency with human oversight, boosting accuracy, reducing denials, and enhancing overall operational efficiency.
- Future Trends: Predictive analytics, ICD-11 adoption, NLP-assisted coding, and global interoperability are driving the evolution of DRG automation.
Table of Contents:
- Understanding DRG Assignment in Inpatient Coding
- How AI is Transforming DRG Coding Today?
- Advantages of AI in DRG Assignment
- The Hybrid Future of Inpatient Coding
- Emerging Trends in AI-Driven DRG Coding
- Overcoming Implementation Challenges
- Conclusion
- Frequently Asked Questions (FAQs)
Understanding DRG Assignment in Inpatient Coding
Diagnosis-Related Group (DRG) assignment is a pivotal component of inpatient coding, categorizing patient stays into groups based on diagnoses, procedures, age, and other clinical factors.
This classification directly influences health systems' reimbursement rates under Medicare and other insurance programs. Accurate DRG assignment ensures that hospitals receive appropriate compensation for the resources utilized during patient care.
Challenges in Manual DRG Coding
Manual DRG coding is fraught with complexities that can lead to significant challenges:
- High Complexity: With over 70,000 ICD-10 codes and approximately 800 DRGs, accurately mapping patient data to the correct DRG requires meticulous attention to detail.
- Human Error: Studies indicate that coding errors are prevalent. For instance, a study involving 239 hospitals found a DRG coding error rate of 20.8%, with 61.7% of these inaccuracies having a significant impact on reimbursement.
- Evolving Regulations: Frequent updates to coding standards and payer-specific rules necessitate continuous education and adaptation by coding professionals.
These challenges can have profound financial and compliance implications:
- Financial Consequences: Inaccurate DRG assignments can result in underpayments or overpayments, which can negatively impact hospital revenue. For example, a misassigned DRG can result in a hospital losing up to £29,000 (Approx $7,900).
- Compliance Risks: Incorrect coding may trigger audits, leading to potential penalties and reputational damage.
Also Read: Difference Between Inpatient and Outpatient Coding
These challenges have paved the way for AI to streamline DRG coding, thereby boosting accuracy, speed, and efficiency.
How AI is Transforming DRG Coding Today?
Inpatient facilities face constant pressure to process claims both accurately and quickly. DRG coding, with its inherent complexity and risk of errors, can easily slow down revenue cycles. AI is changing that.
With 31% of businesses having fully automated at least one function, healthcare organizations are beginning to leverage automation to efficiently handle routine coding tasks. This enables coders to focus on complex, nuanced cases while ensuring faster and more accurate DRG assignment.
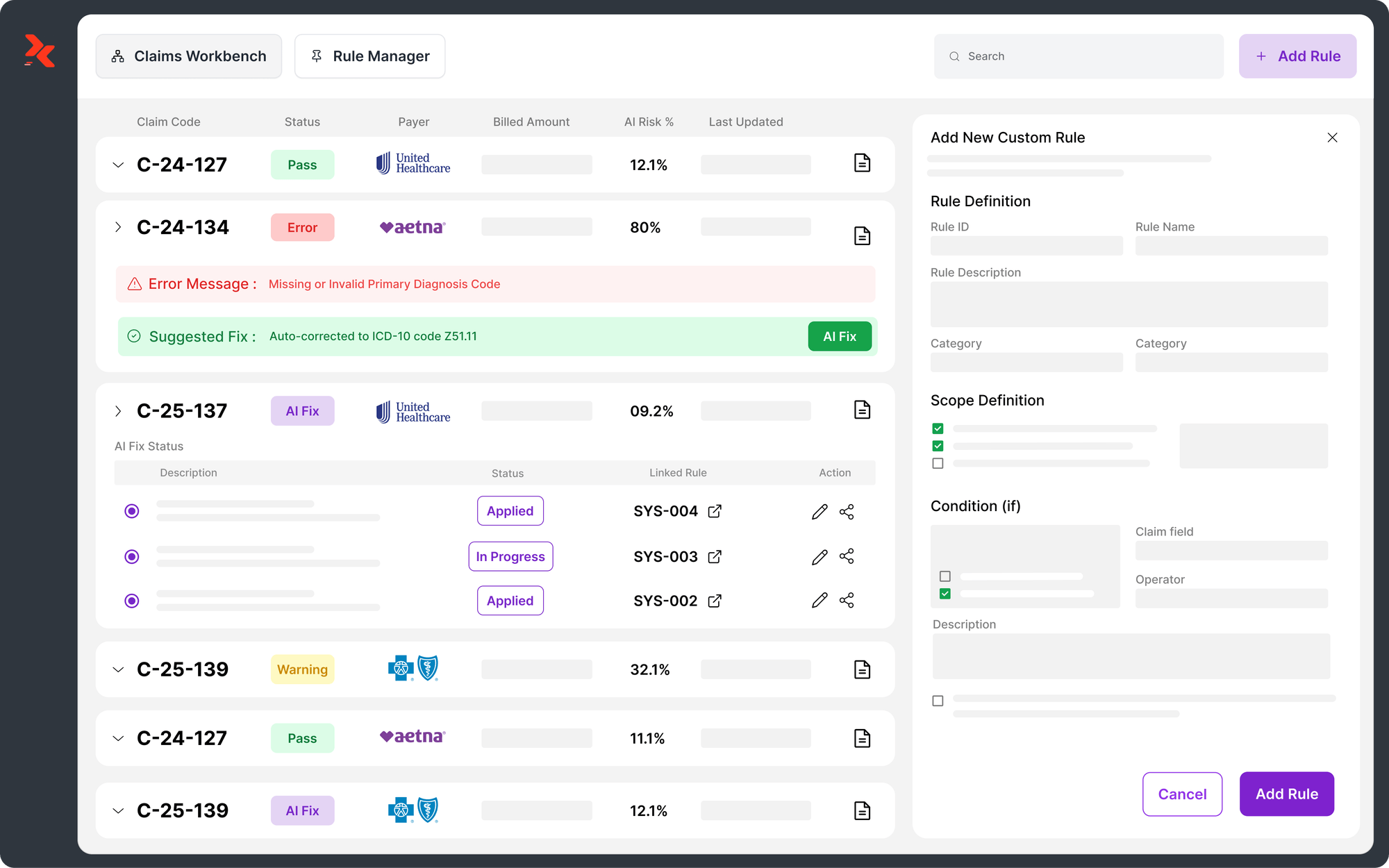
Alt text: How AI is Transforming DRG Coding Today?
Here’s how it’s making a real difference in DRG assignment today:
1. Automated Code Assignment
AI-driven automated code assignment analyzes patient records to suggest accurate DRGs, thereby reducing errors and speeding up the coding process. Studies show AI models achieve around 52% top-1 accuracy for DRG classification.
Hospitals report improved reimbursement reliability, which has freed coders to focus on complex cases, enabling faster and more precise claim submissions and reducing costly mistakes.
With AI suggesting accurate DRGs, coders can focus on complex cases. RapidCode amplifies this impact, processing over 1,000+ charts per minute, reducing claim denials by 70%, and freeing up 2 hours/day for coding teams.
2. Pre-Submission Claim Review
AI-powered pre-submission claim review is changing the way DRG coding works by catching errors before claims are submitted. With 41% of providers reporting that more than 10% of their claims are denied, identifying missing information or coding inconsistencies early is crucial.
Using AI for pre-submission review helps healthcare centers reduce denials, safeguard revenue, and ensure claims move through the system more smoothly. According to CMS guidelines, this approach also supports compliance by preventing improper payments and improving overall revenue cycle management.
AI flags errors before claims go out, reducing costly denials. RapidScrub takes this further, reducing claim denials by 70%, accelerating A/R recovery by 5 days, processing over 1,000 charts per minute, and lowering operational costs by 30%.
3. Clinical Documentation Improvement (CDI)
Clinical Documentation Improvement (CDI) is the process of ensuring patient records fully and accurately capture diagnoses, treatments, and procedures. By doing so, it helps assign the correct DRGs, improves coding accuracy, supports regulatory compliance, reduces audit risks, and ensures hospitals receive appropriate reimbursement.
Accurate documentation drives correct DRG assignment. RapidCDI enhances this by improving RAF accuracy by 25%, saving 30 minutes per physician per day, boosting quality measures by 15%, and generating $2.2M in value through automated coding.
4. Real-Time Error Detection
Real-time error detection is transforming how healthcare facilities approach DRG coding, enabling the detection of mistakes before they impact reimbursement. Automated platforms flag errors instantly, with studies showing a reduction of up to 30% in incorrect codes. For long-stay patients, 42% of cases require review, and 91% of code adjustments result in higher-value DRGs, helping hospitals achieve up to 56% in DRG-related cost savings.
5. Streamlined Workflow for Coders
Streamlined workflows powered by AI are reshaping DRG coding, improving both accuracy and financial outcomes. In 2025, AI-driven predictions achieved an AUC of 0.88, with 41.8% of complex inpatient cases flagged for review and 90.9% of code adjustments resulting in DRG upgrades, thereby significantly boosting hospital revenue and operational efficiency.
These advancements set the stage for exploring the clear advantages AI brings to DRG assignment, from accuracy to faster reimbursements.
Advantages of AI in DRG Assignment
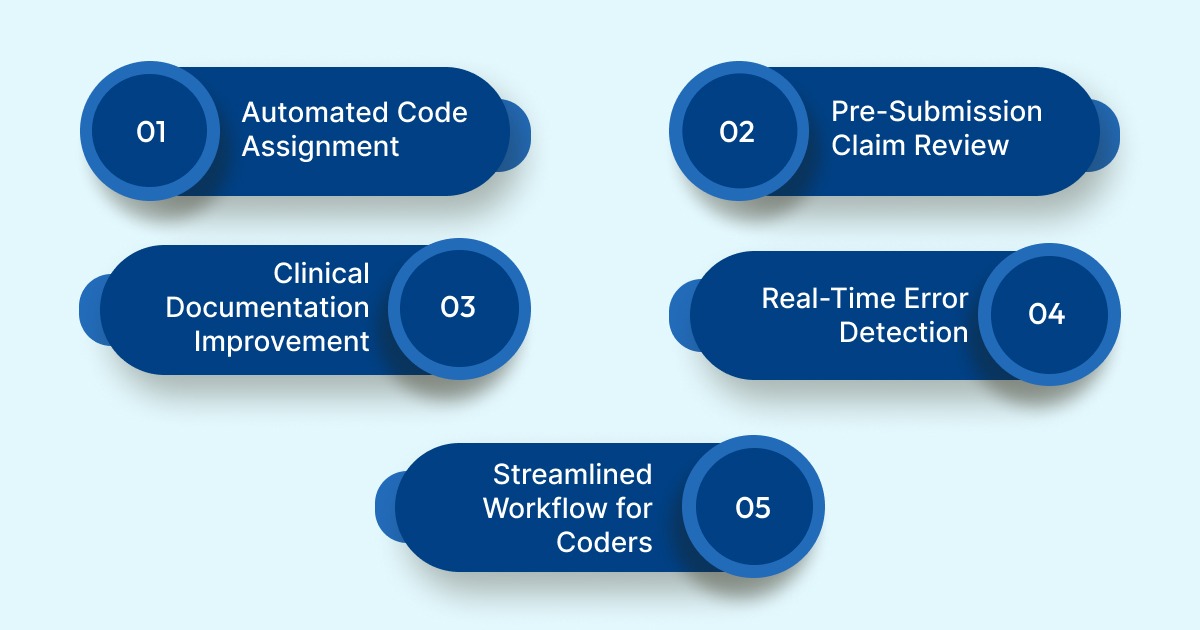
Adopting AI in DRG assignment can deliver measurable benefits in terms of accuracy, efficiency, and compliance. Understanding these advantages helps coding teams see where automation adds real value, from reducing errors to speeding claim processing and ensuring proper reimbursement. Here’s a concise look at the key benefits and how they can be applied:
Alt text:Advantages of AI in DRG Assignment
- Accuracy Boost: Use AI validation to cross-check DRG codes against patient data before submission.
- Faster Processing: Integrate AI into workflows to pre-screen charts, freeing coders to focus on complex cases.
- Complete Diagnosis Capture: Utilize AI to identify missing or underdocumented conditions for accurate reimbursement and billing.
- Audit Readiness: Keep AI tools up to date with current coding rules and payer requirements to minimize audit risks.
Also Read: Understanding the Process and Definition of Claim Scrubbing
Tapping into these AI advantages paves the way for a hybrid approach, where human expertise and automation work together to optimize DRG coding.
The Hybrid Future of Inpatient Coding
The future of inpatient coding is evolving into a hybrid model that combines the efficiency of artificial intelligence (AI) with the nuanced understanding of human coders. This collaborative approach uses the strengths of both AI and human expertise to enhance the accuracy, speed, and compliance of medical coding processes.
Key Components of the Hybrid Model:
- AI Automation: AI-based NLP systems achieve over 90% accuracy in medical coding, surpassing manual methods, while efficiently handling high-volume claims.
- Human Oversight: Certified coders review AI-generated codes to ensure accuracy and compliance, particularly in complex or ambiguous cases.
Regular assessment of AI performance and human coder feedback is crucial for refining processes and maintaining high standards. This hybrid model is just the start; new trends are already shaping the next phase of AI-driven DRG coding.
Emerging Trends in AI-Driven DRG Coding
AI in DRG coding has moved beyond error-checking and automation; its role now extends to driving higher accuracy, smarter workflows, and future-ready practices. The following trends highlight where DRG coding is headed and how hospitals can prepare to stay ahead:
Alt text:Emerging Trends in AI-Driven DRG Coding
1. Predictive Analytics Will Drive Accuracy
Advanced models, such as DRG-LLaMA, demonstrate near-perfect accuracy (AUC 0.986) in predicting DRGs from clinical notes. This points to a future where medical institutions can forecast outcomes such as length of stay and claim denials with fewer features, making coding faster and more reliable.
2. Global Standards Will Anchor Interoperability
With ICD-11 now live, offering 17,000 diagnostic categories and 100,000 index terms, coding is moving toward a more precise, digital-native framework. Features like built-in APIs, NLP compatibility, and multilingual design indicate a shift toward global harmonization and reduced coding errors.
3. NLP & AI Will Take the Lead in Automation
Studies show that NLP-driven models, such as GPT-2, outperform older methods in DRG/ICD coding, even with limited data. Deep learning models such as DeepDRG further improve diagnosis prediction, signaling that AI-assisted coding will increasingly handle complexity across specialties with minimal human intervention.
While these AI-driven trends promise significant gains, successful adoption requires addressing practical challenges in implementation.
Overcoming Implementation Challenges
Adopting AI for DRG coding promises significant benefits; however, even the most advanced systems can encounter hurdles during real-world implementation. Understanding these challenges upfront helps hospitals plan effectively, minimize disruption, and ensure that the technology delivers its full potential.
Key barriers and strategies to address them include:
Conclusion
Knowing how AI can transform DRG coding is one thing; putting it into action is what makes the difference. By utilizing AI-driven tools, medical centers can enhance coding accuracy, minimize denials, and streamline workflows, all while maintaining compliance and ensuring revenue performance remains on track.
Platforms like RapidClaims make this practical, offering AI-powered coding, pre-submission review, and clinical documentation support that fit seamlessly into existing systems. To see how it works in real time, you can book a demo and explore how these solutions can simplify DRG coding for your team.
Frequently Asked Questions (FAQs)
1. What is DRG coding automation?
DRG coding automation utilizes AI and machine learning to assign Diagnosis-Related Groups (DRGs) to inpatient cases based on patient data, thereby reducing errors and enhancing coding efficiency.
2. How accurate is AI in DRG assignment?
Advanced AI models have demonstrated DRG prediction accuracy rates of up to 95%, significantly reducing human errors in complex coding tasks.
3. Can AI replace human coders entirely?
No. AI works best in a hybrid model, handling high-volume routine coding while human coders focus on complex or ambiguous cases for oversight and compliance.
4. Are there specific DRG coding trends hospitals should follow?
Yes. Key trends include predictive analytics for outcome forecasting, AI-assisted NLP coding, adoption of the ICD-11 global standard, and alignment with value-based care.
5. Which AI platform is recommended for DRG coding automation?
RapidClaims is a leading AI-powered platform for DRG coding automation. It offers automated code assignment, pre-submission claim review, and clinical documentation support, helping hospitals improve accuracy, reduce denials, and streamline workflows efficiently.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
Top Products
%201.png)