Downcoding in Medical Billing: Risks, Causes & Prevention

Have you ever submitted a claim expecting full payment, only to get a lower reimbursement code back? Downcoding in medical billing is a growing concern for healthcare providers, leaving the billed service undervalued before it even hits the revenue ledger.
Recent industry data shows that 41% of providers now experience denial rates of 10% or higher, a sign that many payers are scrutinizing documentation and downcoding submissions.
For hospitals, physician groups, and billing organizations, downcoding can quietly erode revenue, disrupt cash flow, and increase administrative burden. In this article, you will explore what downcoding is, why it occurs, and the steps you can take to prevent it.
Key Takeaways
- Downcoding lowers reimbursement by reducing service codes, leading to financial losses and disrupted cash flow.
- It often results from incomplete documentation, payer-specific policies, or misapplied coding standards.
- Risks include delayed payments, increased administrative workload, and potential compliance issues.
- Preventing downcoding requires accurate documentation, AI-driven coding solutions, and continuous staff training.
- Regular audit processes and payer collaboration can also help avoid downcoded claims.
Table of Contents
- What is Downcoding in Medical Billing?
- Difference Between Upcoding and Downcoding
- The Risks of Downcoding in Medical Billing
- 5 Common Causes of Downcoding
- How to Prevent Downcoding in Medical Billing
- How Can RapidClaims Help Combat Downcoding?
- Final Thoughts
- FAQs
What is Downcoding in Medical Billing?
Downcoding occurs when a payer reduces the level of service reported on a claim, often downgrading the procedure or treatment to a lower code than what was actually provided.
This practice, commonly seen in payer audits, can significantly impact a provider's revenue cycle by lowering reimbursements. While sometimes driven by payer policies, downcoding can also stem from incomplete documentation or misinterpretation of coding guidelines.
Understanding how downcoding works is crucial, but it's equally important to differentiate it from upcoding, which carries its own set of challenges and risks in the billing process.
Difference Between Upcoding and Downcoding
Upcoding and downcoding are two billing practices that directly affect reimbursement rates, with upcoding inflating services for higher payment and downcoding reducing the level of service for lower reimbursement.
To better understand these contrasting practices, here's a detailed comparison of upcoding and downcoding:
Understanding how both practices impact healthcare organizations provides clarity on why accurate coding is so important. With this in mind, it's crucial to recognize the risks that come with downcoding in medical billing.
The Risks of Downcoding in Medical Billing
Downcoding can lead to significant financial losses, regulatory scrutiny, and operational inefficiencies.
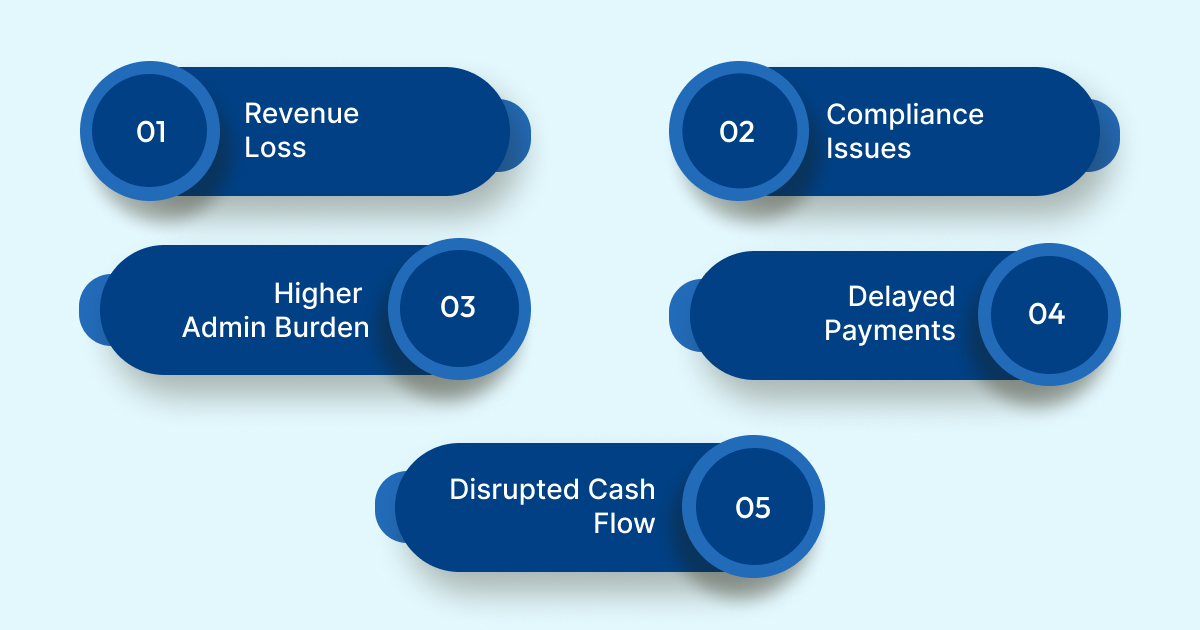
Here are the specific risks associated with downcoding:
- Revenue Loss: Downcoding leads to under-reimbursement, meaning healthcare organizations receive less than what they are entitled to for services provided.
- Compliance Issues: Repeated downcoding can trigger payer audits, with providers potentially facing penalties for inaccurate billing practices.
- Increased Administrative Burden: More time and effort are spent correcting downcoded claims, slowing down the revenue cycle and adding administrative overhead.
- Delayed Payments: Downcoded claims result in slower processing times, extending accounts receivable (A/R) and delaying reimbursements.
- Disrupted Cash Flow: Consistent downcoding creates cash flow uncertainty, making financial planning and operations more difficult.
Recognizing these risks is crucial, but understanding the causes of downcoding is key to implementing effective prevention strategies.
Also Read: Denial Prevention in Healthcare: A Comprehensive Guide for 2025
5 Common Causes of Downcoding
Downcoding often occurs due to payer policies, documentation errors, or misinterpretation of coding guidelines. Identifying the root causes is crucial to implementing effective strategies for prevention.
Here are the specific causes of downcoding:
- Payer Policies: Insurance companies may apply stricter guidelines for reimbursements, automatically downcoding claims that don't meet their predefined criteria.
- Incomplete Documentation: Missing or vague documentation can lead to downcoding, as payers may downgrade claims due to insufficient details supporting the billed service level.
- Incorrect Coding: Misapplication of ICD-10, CPT, or HCC guidelines by coders can result in selecting a lower code than what the service actually warrants.
- Ambiguous Clinical Notes: Lack of clarity in medical records can lead to payers downcoding, especially if key diagnostic information or procedural details are absent.
- Payer-Specific Rule Misinterpretation: Each payer has unique billing rules. Misunderstanding or failing to apply these rules correctly can lead to downcoded claims.
Understanding these causes is the first step in taking preventive action to avoid the negative impacts of downcoding on your revenue cycle.
Recognizing the risks associated with downcoding further emphasizes the importance of effective strategies.
How to Prevent Downcoding in Medical Billing
Preventing downcoding requires a proactive approach to documentation, coding accuracy, and compliance. Implementing practical strategies can reduce the risk and ensure accurate reimbursements.

1. Strengthen Clinical Documentation to Align with Billing Codes
The accuracy of the documentation directly influences the coding process. Ensure that clinical notes are detailed, including all relevant conditions, procedures, and justifications for the level of service provided. Specifically:
- Document complex conditions: For multi-condition diagnoses, ensure that all are clearly documented, including chronic conditions, comorbidities, and complications, which support higher-level codes.
- Avoid vague terms: Refrain from using non-specific language like "chronic pain" without further specifying its underlying cause. Properly document the severity and exact nature of conditions.
- Link diagnoses to treatments: Ensure each diagnosis has a corresponding treatment or procedure documented to substantiate the code level. Missing links will trigger downcoding during payer review.
2. Implement AI and Automation Tools for Coding Accuracy
Automation can significantly reduce the risk of downcoding by ensuring coding consistency and accuracy. Deploy AI-driven coding solutions to assist human coders in selecting the correct codes based on documentation:
- Real-time feedback: Use AI tools that provide real-time suggestions, flagging potential discrepancies between the diagnosis and the assigned code.
- Integration with EHR: Ensure the AI tools are integrated with your Electronic Health Record (EHR) system, enabling seamless validation of medical records against coding standards, such as ICD-10, CPT, and payer-specific rules.
- Continuous updates: Ensure that the AI system is regularly updated to reflect the latest payer requirements and coding guidelines (e.g., CMS updates, ICD-10 revisions).
Wondering how to streamline coding with AI? RapidClaims offers AI-driven solutions like RapidCode, which automates coding, reducing errors and ensuring compliance with up-to-date payer rules.
3. Conduct Periodic Training on Coding Standards and Payer Guidelines
Ongoing education and training are vital to maintain accuracy and compliance in coding practices:
- Payer-specific workshops: Regularly conduct training sessions focused on individual payer guidelines. These sessions should highlight specific rules that might trigger downcoding, such as documentation gaps or unsubstantiated service levels.
- Focus on advanced coding: Provide in-depth training on advanced coding techniques, including risk adjustment coding (HCC) and evaluation and management (E&M) services, where the risk of downcoding is higher due to their complexity.
- Stay updated with regulatory changes: Make sure coders are up to date with the latest regulatory changes from CMS and other key industry bodies. This includes new rules for coding bundled services or updates to ICD-10/ICD-11.
4. Establish an Effective Internal Audit System for Claims Review
Prevention starts before submission. Establish a strong internal audit system to identify potential downcoding issues before claims are sent to payers:
- Random sample audits: Implement regular random audits of coded claims to identify patterns of downcoding. This can catch recurring errors or misunderstandings early in the process.
- Error pattern analysis: Use audit results to identify specific areas where downcoding is most common, such as underreporting of multi-system diseases or procedural codes.
- Pre-submission scrubbing tools: Incorporate pre-submission claim scrubbing tools that flag downcoded claims based on payer rules. RapidScrub by RapidClaims helps prevent denials by automatically detecting and correcting downcoded claims before submission, ensuring compliance and faster payments.
5. Develop Strong Payer Relationships to Clarify Coding Standards
Downcoding often arises from a lack of alignment between the provider's understanding of coding and the payer's expectations.
To avoid this:
- Open lines of communication: Establish regular communication channels with payer representatives to discuss specific downcoding issues, especially for complex cases or services with ambiguous coding guidelines.
- Request regular payer audits: Proactively ask for feedback from payers on claim rejections or downcoding patterns. This feedback helps you adjust coding practices and reduce the risk of similar issues in the future.
- Understand payer-specific edits: Keep a close watch on payer-specific edit policies, such as NCCI (National Correct Coding Initiative) or LCD/NCD (Local Coverage Determinations/National Coverage Determinations), which may downcode claims if certain conditions are not met.
By implementing these actionable strategies, healthcare organizations can prevent downcoding, improve claim accuracy, and safeguard their revenue cycle.
Also Read: From Chaos to Clarity: How AI in Medical Coding Enhances Accuracy
How Can RapidClaims Help Combat Downcoding?
RapidClaims uses AI-driven automation to improve coding accuracy, ensuring a clean claim rate of over 98% and 100% audit compliance. With RapidClaims providers can reduce downcoding and increase productivity by 1.7x, saving up to 2 hours per day.
Here's how RapidClaims helps:
- Autonomous Medical Coding with RapidCode: Achieve 96% coding accuracy and process 1000+ charts per minute, reducing downcoding risks while improving productivity by 170%.
- Proactive Denials Prevention with RapidScrub: Automatically identify and resolve claim issues, leading to a 40% reduction in denials, and 5 days faster A/R recovery.
- AI-Powered Risk and Documentation Improvement with RapidCDI: Optimize HCC capture by 24%, driving an additional $2.2M+ in revenue annually.
By integrating RapidClaims, healthcare providers can significantly enhance their coding accuracy, reduce denials, and streamline their revenue cycle.
Final Thoughts
Downcoding in medical billing leads to under-reimbursement and increased operational costs. By addressing the root causes and implementing preventive strategies, healthcare providers can protect their revenue cycle and ensure accurate reimbursement.
RapidClaims offers AI-driven tools like RapidCode, RapidScrub, and RapidCDI to prevent downcoding, improve coding accuracy, and optimize the revenue cycle.
Schedule a Free Demo today and discover how RapidClaims can transform your billing process!
FAQs
1. Can downcoding affect patient care quality?
Downcoding can lead to financial constraints that limit resources available for patient care. Healthcare providers may need to reduce staff or equipment investment due to reimbursement cuts.
2. How can coders prevent unintentional downcoding?
Coders should focus on detailed, accurate documentation and cross-check it against coding guidelines. Regular peer reviews and updates to coding knowledge can prevent errors.
3. What is the impact of payer-specific downcoding policies on coding practices?
Payer-specific policies often create confusion, leading to inconsistent downcoding. Providers must stay updated on individual payer requirements to avoid claim rejections.
4. Why is downcoding more prevalent in certain specialities?
Specialities with complex, high-cost procedures, such as surgery or cardiology, are often subject to downcoding due to stringent payer reviews and detailed service documentation requirements.
5. How does downcoding affect a provider's relationship with insurance companies?
Frequent downcoding may lead to strained relationships with insurers, as it can signal ongoing issues with billing accuracy. This can complicate negotiations for future reimbursements.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








