.webp)
CO 11 Denial Code: What It Means and How to Fix It

Eligibility and coverage-related denials remain one of the most expensive and avoidable gaps in the revenue cycle. According to MGMA and Change Healthcare, 27% of all medical claim denials stem from eligibility or registration issues, and 86% of them are preventable with improved front-end workflows and automation.
The CO-11 denial code is one of the most common eligibility-related CARC codes used by Medicare, Medicaid, and commercial payers. It generally appears when the patient’s coverage is inactive, invalid, or inconsistent with the billed date of service or procedure. While simple on the surface, CO-11 denials can cause cascading impacts; delayed reimbursement, higher AR days, and unnecessary rework for coding, billing, and registration teams.
As healthcare organizations continue shifting toward value-based care and real-time digital reimbursement, preventing CO-11 denials requires tight alignment between eligibility verification, coding accuracy, payer policy compliance, and automated claim scrubbing. AI-driven revenue cycle automation platforms like RapidClaims help teams identify coverage gaps early, flag coding inconsistencies, and reduce rework long before claims reach the payer.
Key Takeaways
- CO 11 is an eligibility and coverage mismatch denial that occurs when a patient’s insurance is inactive, invalid, or does not support the billed service or diagnosis.
- The most common causes of CO 11 include inactive coverage, demographic errors, outdated insurance cards, gender or age specific diagnosis conflicts, and incorrect coordination of benefits.
- CO 11 denials increase AR days, raise administrative workload, and lower clean claim rates, especially in outpatient and ambulatory settings.
- CO 11 issues are avoidable when teams verify eligibility before every visit, capture accurate insurance data, apply payer specific coverage rules, and follow gender and age specific coding guidelines.
- AI supported RCM tools can help detect coverage mismatches early, apply accurate coding rules, and prevent CO 11 denials before claims reach the payer.
Table of Contents:
- What Is CO 11 Denial Code?
- Common Causes of CO 11 Eligibility and Coverage Denials
- How CO 11 Impacts Your Revenue Cycle
- How to Fix and Resolve CO 11 Denial Codes Step by Step
- How AI and Automation Prevent CO 11 Denials
- CO 11 vs Other Common Eligibility and Coverage Denial Codes
- 2026 Trends in Eligibility Verification That Reduce CO 11 Denials
- Conclusion
- FAQs
What Is CO 11 Denial Code?
The CO 11 denial code is a Claim Adjustment Reason Code (CARC) that indicates the patient’s insurance coverage is not active, not valid, or not consistent with the billed service or diagnosis.
Depending on the payer, CO 11 may also appear when:
- The diagnosis is inconsistent with the patient’s gender
- The coverage rules do not support the billed procedure for that plan type
In all cases, CO 11 points to a coverage or eligibility mismatch that prevents the payer from processing the claim correctly.
Most Common Times Payers Use It
Payers typically assign CO 11 during the initial automated claim intake process when eligibility or coverage checks do not match the submitted information. Common triggers include:
- Insurance inactive or terminated on the date of service
- Subscriber or dependent information not found in the payer system
- Procedure not covered under the patient’s benefit plan
- Gender specific or age specific diagnosis inconsistencies
- Incorrect or outdated coordination of benefits information
These issues occur early in adjudication, so CO 11 is one of the most common front end denials in outpatient, ambulatory, and specialty practices.
How CO 11 Appears on EOBs and ERA Files
CO 11 appears on payer remittances such as Explanation of Benefits (EOBs) and Electronic Remittance Advice (ERA) files. You may see it listed in one of the following formats:
- "CO 11: The diagnosis is inconsistent with the patient’s gender."
- "CO 11: The diagnosis is inconsistent with the patient’s age or gender or is not covered."
- "CO 11: Patient eligibility not valid for date of service."
- "CO 11: This service is not covered under the patient’s current insurance plan."
Payers may also include a Remittance Advice Remark Code (RARC) that provides extra detail, such as asking for updated eligibility verification or corrected demographic information.
CO 11 often appears next to other coverage related CARCs such as CO 22 for coordination of benefits concerns or CO 27 for coverage not available. This grouping helps identify that the claim failed at the coverage validation step.
Common Causes of CO 11 Eligibility and Coverage Denials
CO 11 denials occur when the information on a claim does not match what the payer has on file for the patient’s coverage. Although the specific wording on remittances can vary, most CO 11 errors fall into predictable categories that relate to eligibility, plan validation, or basic demographic alignment.
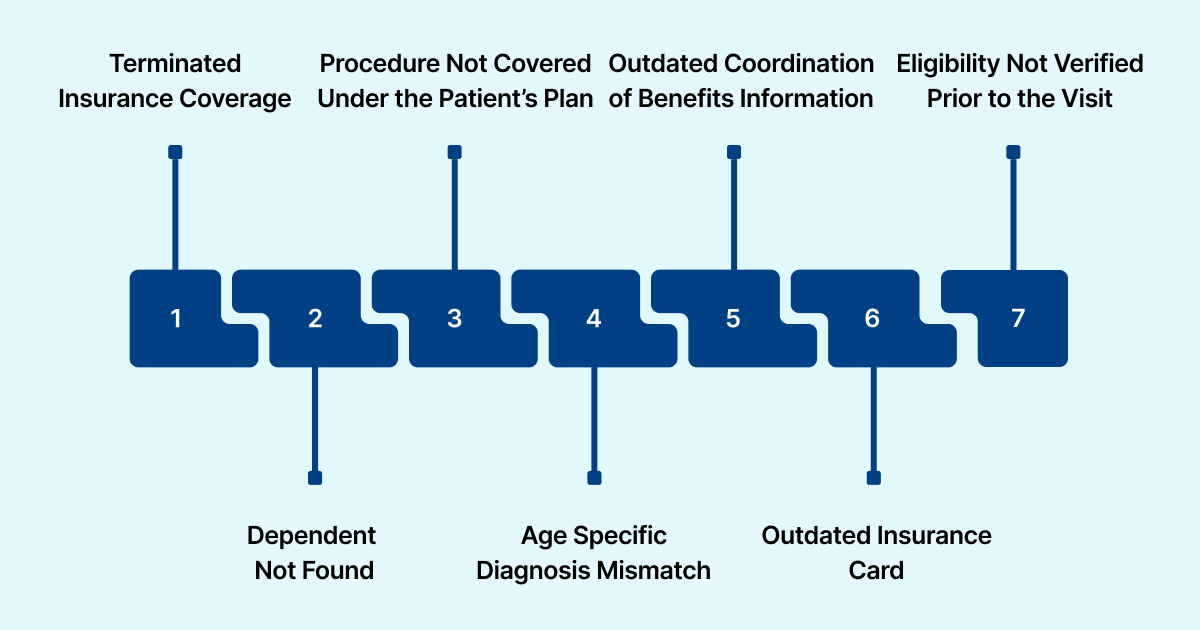
1. Inactive or Terminated Insurance Coverage
This is the most frequent cause of CO 11. The patient’s plan may have expired, been replaced, or terminated before the date of service. Even small timing gaps between visits and coverage changes can trigger CO 11.
2. Subscriber or Dependent Not Found
If the patient’s name, date of birth, member ID, or relationship code does not match the payer system, the claim fails eligibility validation. A single digit error in a member ID can lead to CO 11.
3. Procedure Not Covered Under the Patient’s Plan
Some services are only covered under specific benefit tiers or plan types. If the billed CPT or diagnosis combination falls outside covered benefits, the payer may respond with CO 11 instead of a medical necessity denial.
4. Gender or Age Specific Diagnosis Mismatch
Payers use CO 11 when a diagnosis does not align with the patient’s gender or age. Examples include gender specific codes for reproductive health or age specific preventive services.
5. Incorrect or Outdated Coordination of Benefits Information
If the payer needs updated primary or secondary insurance information, or if the order of coverage is incorrect, CO 11 may appear until the COB file is corrected.
6. Outdated Insurance Card or Missing Front End Verification
Incorrect policy numbers, group numbers, or plan information from an old insurance card often lead to CO 11. These errors are common when coverage changes occur at the beginning of the year or during employer enrollment shifts.
7. Eligibility Not Verified Prior to the Visit
When eligibility checks are skipped or rushed, claims are more likely to reach the payer with incorrect data. This often leads to preventable CO 11 denials during the payer’s initial intake process.
Also read: Essential Guide to Healthcare Data Compliance & Protection
How CO 11 Impacts Your Revenue Cycle
CO 11 denials create significant operational and financial strain across the revenue cycle because they occur early in the adjudication process and often signal preventable front end breakdowns. Although each denied claim represents a small error, the cumulative effect across patient visits, service lines, and locations can be substantial.
RapidCode supports this by applying payer-aware, demographic-aligned coding before claims are submitted, helping teams catch mismatches that commonly lead to CO 11 denials.
How to Fix and Resolve CO 11 Denial Codes Step by Step
Resolving a CO 11 denial requires validating eligibility, correcting coverage data, and ensuring that the billed service aligns with the patient’s active plan. Because CO 11 is often triggered before formal adjudication, most fixes involve front end or registration level corrections rather than coding changes alone.
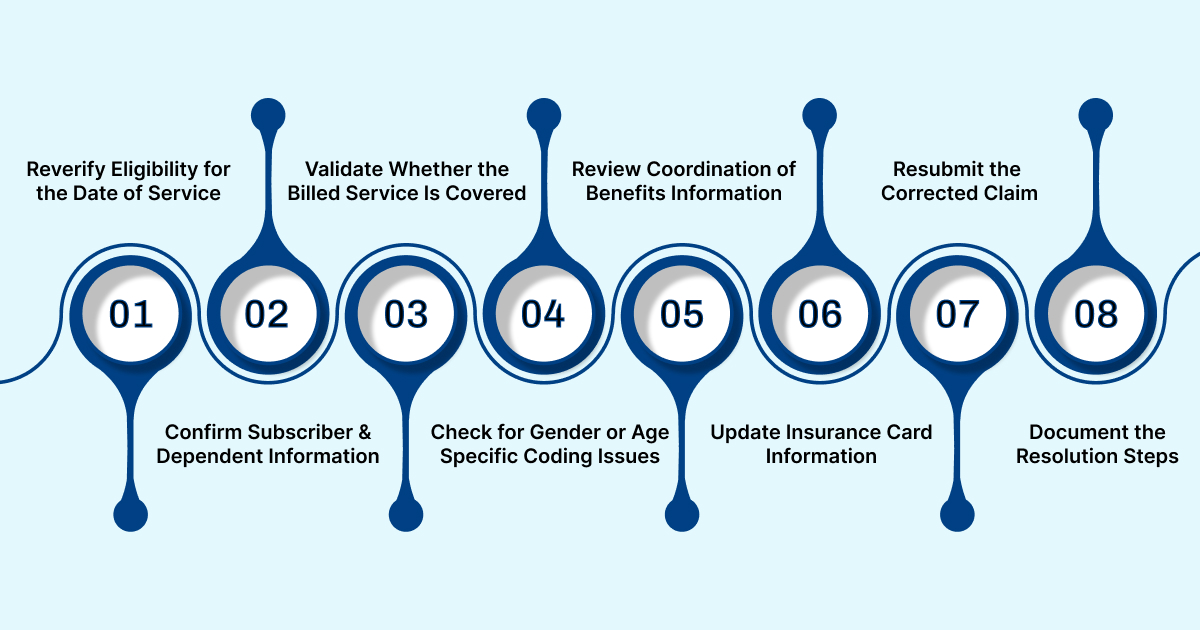
1. Reverify Eligibility for the Date of Service
Start with a fresh eligibility check through the payer portal, clearinghouse, or EHR integrated verification tool. Confirm that the plan was active on the exact date the service was performed. If coverage was inactive, contact the patient to obtain updated insurance information.
2. Confirm Subscriber and Dependent Information
Check all demographic fields for accuracy. Review:
- Member ID
- Subscriber name
- Date of birth
- Relationship code
- Group number
Correct any errors and update the patient’s registration file in the EHR or practice management system.
3. Validate Whether the Billed Service Is Covered
Some payers use CO 11 when a CPT or ICD combination does not fall under the patient’s benefit plan. Review the payer’s coverage criteria, benefit tier rules, and medical policy documents.
If the service is not covered, determine whether a corrected claim, prior authorization check, or appeal is appropriate.
4. Check for Gender or Age Specific Coding Issues
If the denial message mentions diagnosis inconsistency with patient gender or age, review the codes for:
- Gender specific diagnoses
- Age dependent preventive services
- Procedure or diagnosis combinations that trigger demographic rules
Correct codes when appropriate and ensure documentation supports the changes.
5. Review Coordination of Benefits Information
If the payer requires updated COB information, confirm whether another plan should be primary. Update the insurance order in the system and send the corrected claim once COB is verified.
6. Update Insurance Card Information
Request a current insurance card if the denial suggests outdated or incorrect plan details. Enter all information exactly as printed, including plan numbers, prefixes, and suffixes.
7. Resubmit the Corrected Claim
After confirming eligibility and correcting all mismatched data, submit a corrected claim through the standard submission workflow. If the payer requires a reconsideration or appeal instead of a corrected claim, follow the guidelines in the payer’s ERA remarks.
8. Document the Resolution Steps
Record all updates in the claim notes, including eligibility confirmation, demographic corrections, COB changes, or coding adjustments. This ensures transparency for future audits and helps prevent repeat CO 11 errors.
How AI and Automation Prevent CO 11 Denials
AI enabled tools play an important role in preventing CO 11 denials by validating eligibility, coverage rules, and coding accuracy before a claim is submitted. Automation helps close the gaps that commonly lead to CO 11 issues such as outdated insurance information, demographic mismatches, gender specific coding errors, or incomplete coordination of benefits.
1. Real Time Eligibility Verification Through Automated Data Feeds
AI driven systems can pull eligibility information in real time through integrated payer APIs, clearinghouses, or EHR connections. This reduces the risk of inactive coverage, terminated plans, or incorrect member IDs.
RapidScrub supports this step by performing automated eligibility and demographic checks at the front end of the workflow to detect mismatches before the claim is created.
2. Automated Review of Patient Demographics Against Payer Records
Automation can compare name, date of birth, member ID, and relationship codes against payer databases to ensure accuracy. This reduces demographic related CO 11 denials.
3. AI Assisted Coding That Applies Gender and Age Specific Rules
AI medical coding systems can identify when a diagnosis code is not compatible with a patient’s age or gender. This prevents common demographic mismatches that trigger CO 11.
RapidCode uses rule based and machine learning logic to ensure diagnosis and procedure codes are compatible with patient demographics.
4. Automated Coverage Policy Checks for CPT and ICD Combinations
AI can evaluate whether billed services fit within the patient’s active benefit plan. This includes checking procedure codes against payer coverage policies and benefit tiers.
5. Predictive Identification of CO 11 Risk Based on Historical Patterns
AI can analyze past claims and identify patterns that signal a high likelihood of CO 11 errors. These include seasonal plan changes, employer transitions, or common registration mistakes.
6. Integrated Front End to Back End Workflow Automation
When automation is embedded across scheduling, registration, coding, charge entry, and billing, data remains consistent throughout the revenue cycle. This reduces the chance of eligibility errors or documentation gaps.
RapidClaims connects through HL7 and FHIR interfaces to ensure accurate coverage and coding data flows across the entire RCM process. If you are ready to cut eligibility and coding denials by up to 70 percent and improve clean claim performance, request a demo today.
CO 11 vs Other Common Eligibility and Coverage Denial Codes
CO 11 is often confused with other eligibility- and coverage-related denial codes. While they may appear similar on remittance advice, each code points to a different failure point in the revenue cycle.
Misclassifying CO 11 as a medical necessity or coding-only denial can lead to unnecessary appeals and delayed reimbursement. CO 11 is most often resolved by front-end corrections, such as eligibility re-verification, demographic updates, COB fixes, or coverage validation, rather than clinical appeals.
AI-enabled RCM platforms help differentiate these denial types automatically, ensuring claims are routed to the correct resolution workflow and reducing wasted effort across registration, coding, and billing teams.
2026 Trends in Eligibility Verification That Reduce CO 11 Denials
Eligibility and coverage validation are evolving quickly as payers, providers, and technology vendors move toward real time data exchange and automated decision support. In 2025, several trends are shaping how organizations prevent CO 11 denials and strengthen front end accuracy.
1. Wider Adoption of Real Time Payer API Connections
More payers are supporting real time eligibility APIs that provide up to date coverage information directly from the payer source. These connections reduce reliance on batch files and minimize outdated plan data.
2. Integration of HL7 FHIR Standards Across EHR and RCM Systems
FHIR based data exchange allows eligibility, demographic, and coverage information to flow more accurately between EHRs, clearinghouses, and RCM platforms. This improves accuracy for member IDs, plan types, and benefit restrictions that typically trigger CO 11.
3. Expansion of Digital Coverage Rules by Medicare and Commercial Payers
CMS and commercial payers are publishing more digital policy rules that outline benefit limitations, demographic restrictions, and CPT to ICD coverage logic. These structured rules help systems flag errors earlier in the process.
4. Growth of AI Enabled Eligibility Verification Tools
Organizations are increasing their use of AI tools that compare patient information with payer databases, detect inconsistencies, and flag high risk claims before submission. These tools reduce manual work and improve clean claim rates.
5. More Frequent Insurance Changes by Patients
Patients are switching plans more often due to employer changes, marketplace shifts, and benefit redesigns. This creates a higher risk of outdated plan information and increases the importance of repeated eligibility checks.
6. Greater Focus on Front End Denial Prevention in Outpatient and Ambulatory Care
High volume outpatient settings are prioritizing early detection of eligibility issues because frequent visits and rapid patient turnover increase the chances of CO 11 denials.
7. Consolidation of Coverage Data Across RCM Workflows
Many organizations are centralizing eligibility, demographic, and coverage validation into a single workflow to reduce fragmented processes. This helps maintain consistent patient data from scheduling to claims submission.
Conclusion
CO 11 denials are highly preventable when eligibility, demographics, and coverage rules are verified correctly at the front end. Strengthening these workflows reduces rework, shortens payment cycles, and improves clean claim performance across outpatient and specialty settings.
AI supported automation can help teams catch mismatches early, validate coverage accurately, and maintain compliance with CMS and payer requirements. RapidClaims brings these capabilities into one integrated workflow so organizations can prevent CO 11 issues before claims reach the payer.
If you want to reduce eligibility related denials and improve clean claim rates, request a RapidClaims demo to see how automated validation can support your RCM team.
FAQs
Q. What does CO-11 denial code mean?
A: CO-11 generally means there is a mismatch between the diagnosis code (ICD/diagnosis) and the procedure code (CPT/HCPCS or service) submitted on the claim. The payer considers that the diagnosis does not support or justify the rendered service or procedure.
Q. When will a payer typically assign CO-11 on a claim?
A: A payer assigns CO-11 when, during claim adjudication or review, it finds that the diagnosis and procedure codes do not align; either because the diagnosis is too general, does not support medical necessity, or because the procedure or service falls outside coverage guidelines under that diagnosis.
Q. Can CO-11 result from coding errors or outdated codes?
A: Yes. Common triggers for CO-11 include incorrect diagnosis or procedure codes, outdated or invalid codes, inappropriate modifiers, or codes that do not reflect the clinical documentation. Even when codes are technically valid, if they don’t support medical necessity or documentation is insufficient, CO-11 can be applied.
Q. Does CO-11 always mean the service was not medically necessary?
A: Not always. While CO-11 often reflects concerns about medical necessity, in many cases it is simply a “diagnosis-procedure mismatch.” If documentation supports justification for the service, or if a corrected diagnosis-procedure alignment is provided, the claim could be resubmitted or appealed.
Q. How common is CO-11 compared to other denial codes?
A: CO-11 is widely recognized among the most common coding-related denial codes. Denial-code guides list it as a frequent reason for claim rejection due to coding mismatches and coverage verification failures.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
What Is An Additional Diagnosis In Medical Coding And Why It Matters For Reimbursement?
Related Post
Top Products

%201.png)








