Unlocking the Future of Integrated Healthcare: A Deep Dive into Strategic Practice Building

Healthcare today is changing faster than ever, and organizations that rely on fragmented systems risk inefficiencies, delayed reimbursements, and compliance challenges. Seamless, patient-centered care is no longer just a goal; it is essential for success in a diverse healthcare environment.
In 2024, the global service integration and management in healthcare market was valued at $5.43 billion and is projected to reach $8.28 billion by 2030. For healthcare professionals, understanding integrated healthcare management is crucial for enhancing patient outcomes, optimizing operations, and ensuring regulatory compliance.
In this blog, you will learn how this integrated approach enhances revenue cycle performance, supports accurate medical coding, and strengthens overall care coordination across healthcare organizations.
TL;DR (Key Takeaway)
- Unified Management: Integrated healthcare management connects clinical, administrative, financial, and compliance systems to boost efficiency and patient outcomes.
- Coding Importance: Accurate medical coding is vital for revenue cycle performance, regulatory compliance, and informed decision-making.
- Key Challenges: Workflow alignment, data interoperability, regulatory adherence, change management, and financial investment remain significant hurdles.
- Best Practices: Standardized processes, AI-driven platforms like RapidClaims, staff training, patient-focused workflows, and continuous audits enhance performance.
- Emerging Trends: AI, telemedicine, blockchain, and population health analytics are shaping the future of integrated healthcare strategies.
Table of Contents:
- What is Integrated Healthcare Management?
- Why Integration Makes a Difference in Healthcare Management?
- Critical Role of Medical Coders in Integrated Healthcare
- Challenges in Integrated Healthcare Management
- Best Practices for Effective Integrated Healthcare Management
- Looking Ahead: The Future of Integrated Healthcare
- Final Thoughts
- Frequently Asked Questions (FAQs)
What is Integrated Healthcare Management?
Integrated healthcare management refers to the coordinated alignment of clinical, administrative, financial, and compliance functions within a single, interoperable framework. Its goal is to ensure seamless, patient-centered care while improving process accuracy and adherence to healthcare regulations.
To achieve this, organizations typically rely on a combination of interoperable systems, such as:
- Electronic Health Records (EHRs): Serve as centralized repositories for patient data, enabling real-time access and coordination across providers.
- Revenue Cycle Management (RCM) Systems: Optimize financial operations from patient intake to final reimbursement, reducing claim denials and delays.
- Compliance and Audit Tools: Ensure adherence to HIPAA, CMS, and other regulatory standards while maintaining audit readiness.
- Clinical Decision Support Systems (CDSS): Provide evidence-based insights to assist clinicians in diagnosis, treatment planning, and medication management.
- Data Integration Platforms: Connect disparate systems and standardize data using frameworks like HL7 and FHIR for secure, efficient information exchange.
Together, these systems enable seamless information flow, improve coordination across departments, and provide the foundation for data-driven, patient-centered healthcare management.
Now, let’s examine how unifying clinical, financial, and administrative processes enhances efficiency, compliance, and patient outcomes in healthcare management.
Why Integration Makes a Difference in Healthcare Management?
Integrated healthcare management goes beyond simply connecting systems; it fundamentally reshapes how healthcare organizations deliver care, manage operations, and ensure compliance.
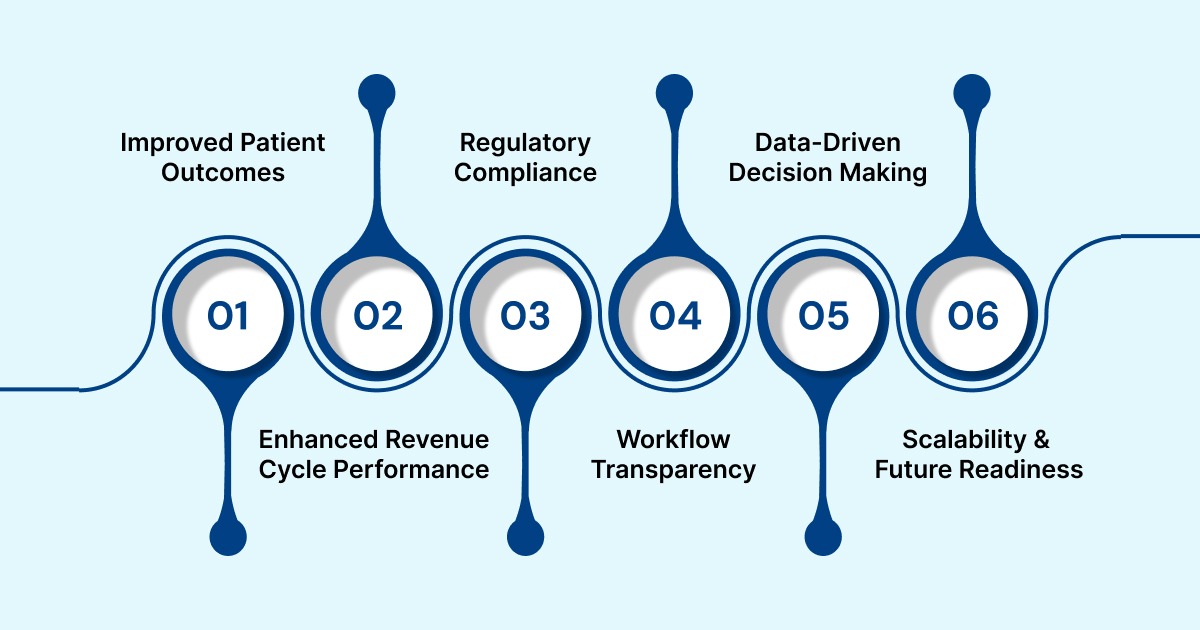
Alt text:Why Integration Makes a Difference in Healthcare Management?
Below are the key benefits of integrating healthcare management systems:
1. Improved Patient Outcomes
Integrated systems provide clinicians with a comprehensive view of a patient's history, lab results, medications, and prior procedures. This reduces errors, prevents duplicate tests, and ensures timely interventions, ultimately improving care quality and patient safety.
2. Enhanced Revenue Cycle Performance
Linking coding, billing, and RCM platforms reduces claim errors, accelerates reimbursements, and lowers accounts receivable days. Organizations benefit from optimized cash flow and fewer denied or delayed claims.
3. Regulatory Compliance and Audit Readiness
Standardized documentation and automated compliance checks simplify adherence to HIPAA, CMS, and other regulations. Real-time auditing features help identify potential gaps before they become compliance risks.
4. Workflow Transparency and Efficiency
Unified platforms provide a clear view of workflows, patient journeys, and departmental performance. This transparency enables better resource allocation, reduces administrative bottlenecks, and streamlines the decision-making process.
5. Data-Driven Decision Making and Analytics
Consistent and accurate data from integrated systems support predictive analytics, population health management, and evidence-based strategic planning. Leaders can make informed decisions to improve clinical outcomes and organizational efficiency.
6. Scalability and Future Readiness
Integrated healthcare frameworks enable organizations to scale their operations, adopt emerging technologies such as AI and telemedicine, and adapt quickly to evolving regulatory and market requirements. This strategic approach strengthens every aspect of healthcare delivery, from patient care to operational management and compliance.
Now, let’s take a closer look at the critical role medical coders play in ensuring accuracy, compliance, and efficiency within integrated healthcare systems.
Critical Role of Medical Coders in Integrated Healthcare
Medical coders serve as the link between clinical documentation and administrative, financial, and regulatory processes. They convert patient records into standardized codes for diagnoses, procedures, and services, ensuring accurate reimbursement, regulatory compliance, and reliable data for analytics and decision-making.
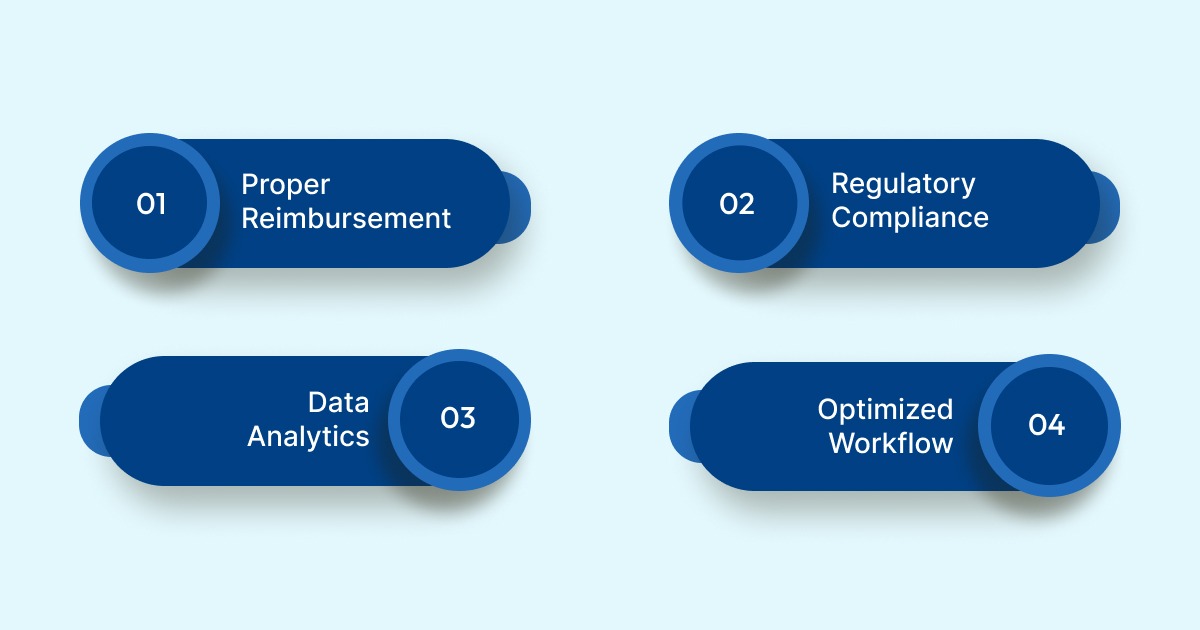
Alt text:Critical Role of Medical Coders in Integrated Healthcare
Below are the key contributions of medical coders in supporting accurate healthcare decisions:
- Proper Reimbursement: Correct medical coding ensures that healthcare providers receive accurate and timely payment from insurers, reducing claim denials and financial losses.
- Regulatory Compliance: Adhering to ICD, CPT, and HCPCS coding standards minimizes audit risks and helps healthcare organizations meet the requirements of HIPAA and CMS.
- Data Analytics and Quality Improvement: Standardized codes allow hospitals and clinics to analyze patient outcomes, identify trends, track population health, and support evidence-based decision-making.
- Optimized Workflow: When medical coding systems are integrated with Electronic Health Records (EHRs) and Revenue Cycle Management (RCM) platforms, workflows become more streamlined, resulting in reduced errors and administrative burdens.
Also Read: 4 Basic Types of Health Care Systems and Their Structures
By ensuring accuracy and consistency across clinical, financial, and administrative domains, medical coders contribute to better patient care, improved revenue cycles, and a compliant, data-driven healthcare environment.
Challenges in Integrated Healthcare Management
Implementing integrated healthcare management presents several challenges that healthcare organizations must address to achieve seamless operations:
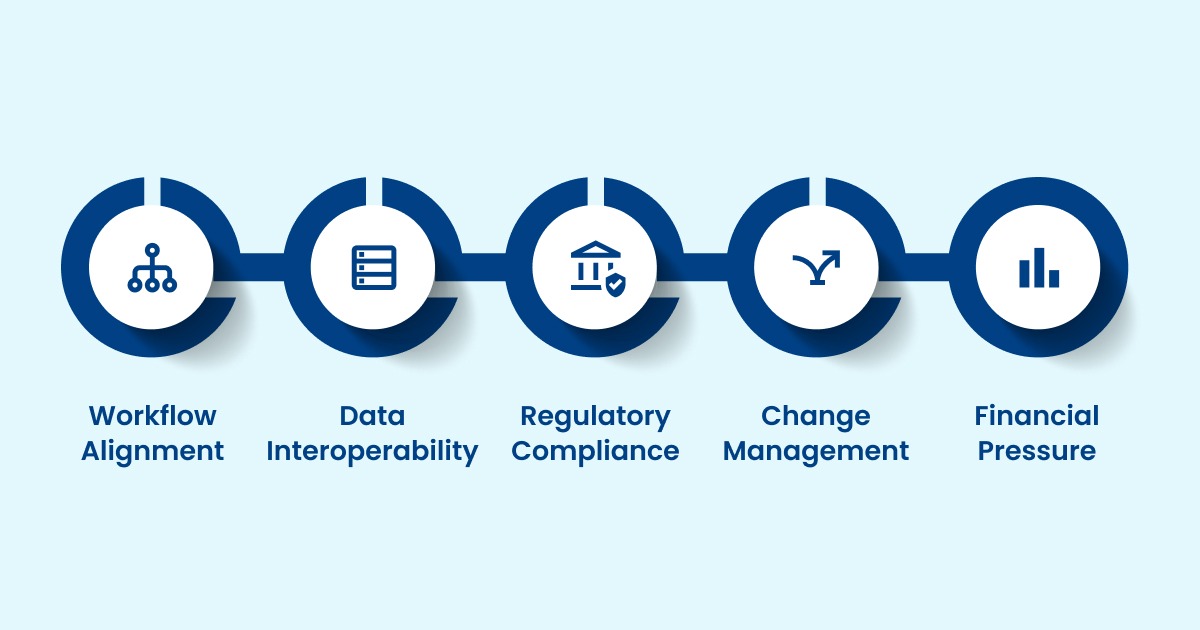
Alt text:Challenges in Integrated Healthcare Management
1. Workflow Alignment: Coordinating clinical, administrative, and financial processes across multiple departments can be complex.
Example: A patient undergoing surgery may require coordination among the pre-operative, surgical, billing, and post-operative care teams. Misaligned workflows can delay billing and care delivery.
2. Data Interoperability: Disparate EHRs, medical coding systems, and RCM platforms can create data silos, increase errors, and slow operations.
Example: Lab results entered in one system may not sync with the billing system, causing incorrect claims or repeat testing.
3. Regulatory Compliance: Ensuring adherence to HIPAA, CMS, and local regulations requires dedicated resources, audits, and training.
Example: Failure to update documentation standards for telemedicine visits can result in compliance violations or claims being denied.
4. Change Management: Transitioning to integrated systems demands staff training, workflow adjustments, and stakeholder buy-in.
Example: Nurses and coders may resist adopting a new EHR interface, slowing implementation and causing temporary data entry errors.
5. Financial Pressure: Integration projects require upfront investments in technology and training, which can be a barrier for smaller organizations.
Example: Small clinics may struggle to fund a centralized RCM and EHR system, delaying integration and continuing inefficiencies.
To address these integration challenges, healthcare organizations can utilize RapidClaims, an AI-powered revenue cycle platform. It achieves a 98% clean-claim rate, a 170% increase in coder productivity, and a 40% reduction in denials. RapidClaims automates medical coding, clinical documentation, and denial management, accelerating revenue cycles while ensuring compliance.
Best Practices for Effective Integrated Healthcare Management
Successfully implementing integrated healthcare management requires a structured approach that combines technology, standardized processes, and staff engagement. To achieve seamless operations, improved compliance, and better patient outcomes, organizations should focus on several key best practices:
- Standardize Clinical and Administrative Processes: Define uniform documentation standards, coding protocols, and data entry procedures across all departments to minimize errors, reduce variability, and maintain consistent quality of care.
- Utilize Advanced Technology: Implement AI-driven solutions, such as RapidClaims, to aggregate clinical and RCM data, provide predictive insights, and automate workflows. This ensures real-time operational visibility, seamless data exchange across EHR and billing systems, and streamlined decision-making, supporting a fully integrated healthcare management system.
- Ongoing Staff Training and Communication: Provide continuous education on updated regulations, system features, and process changes while fostering cross-department collaboration to maintain operational consistency and compliance.
- Patient-Centered Focus: Structure integrated workflows around patient needs, ensuring seamless care coordination, improved satisfaction, and measurable outcomes while aligning workflow efficiency with clinical priorities.
- Regular Audits and Feedback Loops: Implement continuous monitoring, performance tracking, and structured feedback mechanisms to identify inefficiencies, proactively address gaps, and drive iterative improvements in both clinical and administrative processes.
Also Read: How to Choose the Right Practice Management System for Medical and Legal Workflows
Applying these best practices equips healthcare organizations to operate efficiently, maintain regulatory adherence, and deliver high-quality, patient-centered care.
Looking Ahead: The Future of Integrated Healthcare
The future of integrated healthcare management is shaped by rapid technological advancements and increasing demands for seamless, patient-centered care. To stay ahead, healthcare organizations are focusing on key emerging trends that drive efficiency, compliance, and improved outcomes:
Alt text:Looking Ahead: The Future of Integrated Healthcare
- Artificial Intelligence (AI): AI-driven analytics and decision-support tools enable predictive insights, early risk detection, and optimized care pathways across clinical and administrative processes.
- Telemedicine: Remote care solutions are becoming fully integrated with EHRs and RCM systems, ensuring continuity of care, improving access, and reducing operational bottlenecks.
- Blockchain: Secure, decentralized data sharing across providers and patients enhances interoperability, protects sensitive information, and strengthens audit and compliance capabilities.
- Data-Driven Population Health Management: Utilizing aggregated patient data enables the identification of trends, effective management of chronic conditions, and optimized resource allocation across healthcare networks.
Also Read: Top Vendors for Revenue Cycle Management in Healthcare
As the healthcare ecosystem continues to change, staying proactive, adaptable, and technology-enabled will be essential for professionals managing integrated healthcare systems.
Final Thoughts
Fragmented workflows and manual processes continue to slow reimbursements, increase errors, and create compliance risks. Integrated Healthcare Management addresses these issues by connecting clinical, financial, and compliance systems into a single, data-driven framework. The result is improved coding accuracy, faster revenue cycles, and stronger audit readiness.
For organizations seeking to achieve this level of integration, RapidClaims offers AI-driven automation that unifies coding, billing, and audit processes. This improves claim accuracy, accelerates revenue cycles, and ensures regulatory compliance across all workflows.
Don’t let disconnected systems hold back your operations. Visit RapidClaims to explore how intelligent integration can transform your workflows. Request a free demo today!
Frequently Asked Questions (FAQs)
1. How do I begin integrating legacy systems into a unified healthcare management platform?
A. Start with a complete audit of all existing systems and data flows. Use APIs or middleware to connect EHR, billing, and scheduling tools. Standardize data using formats like HL7 or FHIR. Test integration in one area before expanding across departments.
2. What metrics should I track to measure success after implementing integration?
A. Monitor key metrics such as claims denial rates, coding accuracy, and days in accounts receivable. Compare pre- and post-integration data for measurable improvements. Include patient metrics such as treatment turnaround times and satisfaction rates. Continuous monitoring ensures ROI and efficiency gains.
3. How can I ensure data security when centralizing clinical and financial workflows?
A. Apply encryption for stored and transmitted data, along with strict role-based access controls. Maintain detailed audit logs and monitor systems for anomalies. Conduct regular vulnerability tests and staff security training. Consistent policy enforcement helps prevent data breaches.
4. What challenges might I face when scaling integrated healthcare across multiple facilities or regions?
A. Different IT systems and compliance rules across locations create integration complexity. Maintaining data consistency and governance can be challenging. Staff adoption and workflow alignment also pose challenges. A phased rollout with centralized oversight improves scalability.
5. Can I use integrated systems to support value-based care and alternative payment models?
A. Yes. Integrated systems consolidate patient data for performance and cost tracking. They enable risk stratification, population health monitoring, and outcome measurement. These insights support value-based reimbursements. Accurate, real-time data strengthens compliance and financial performance.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
Top Products

%201.png)








