RPA in Healthcare Claims Processing: Benefits and Use Cases

Healthcare organizations are experiencing increasing administrative pressure as claim volumes rise and payer requirements become more complex. This strain is especially evident in claims processing, where manual tasks, inconsistent documentation, and variable workflows slow reimbursement and create financial risk. In fiscal year 2024, the Medicare Fee-for-Service estimated improper payment rate was 7.66 percent, representing $31.70 billion in improper payments, highlighting how documentation and billing errors contribute to inaccuracy and rework across high-volume claims workflows.
This environment creates a strong need for technology that reduces manual work and prevents errors before claims reach the payer. Robotic Process Automation, or RPA, offers a practical path forward by streamlining repetitive administrative steps, improving consistency, and supporting cleaner claims at the start of the cycle. As margins tighten and staffing remains constrained, RPA is becoming an essential tool for more reliable reimbursement and stronger financial performance.
Key Takeaways
- Rising denial rates and expanding payer requirements are increasing pressure on revenue cycle teams, which makes automation a strategic priority for health systems.
- RPA reduces manual effort in claims processing by handling routine, rules based tasks such as data collection, claim assembly, configuration checks, and queue management.
- Upstream RPA activities, including document retrieval, referral validation, and financial clearance support, strengthen the information foundation that claims depend on.
- RPA improves claim accuracy and speed by preparing complete claim files, attaching required documents, verifying configuration details, and organizing claims for review.
- AI complements RPA by interpreting clinical documentation, identifying coding needs, validating completeness, and flagging potential claim risks before submission.
- Effective RPA programs require stable workflows, defined bot access, clear exception ownership, regular script reviews, and performance tracking to maintain reliability.
- A phased implementation approach helps organizations introduce automation in a controlled manner and expand it across related claim tasks without disrupting operations.
- AI tools like RapidClaims enhances RPA by adding AI driven coding intelligence, documentation analysis, risk adjustment support, and workflow orchestration, which leads to stronger and more compliant claims.
Why Healthcare Revenue Cycle Teams Are Adopting RPA
Revenue cycle teams complete many detailed steps for each claim. These steps often involve repetitive data entry, movement across several systems, and manual checks that must be completed before coding and submission. Although essential, these tasks take time and introduce opportunities for error.

- Manual Workload and Fragmented Systems: Billing and coding staff work across EHRs, clearinghouses, payer portals, scanned documents, and spreadsheets. Moving between these systems increases the chance of inconsistencies and makes it difficult to maintain standardized workflows across departments.
- High Error Rates and Financial Impact: Small inaccuracies, such as incomplete insurance information or incorrect patient data, can trigger immediate rejections. These issues often arise before coding and require repeated manual correction, which slows reimbursement and adds administrative cost.
- Growing Compliance Pressure: Payer programs continue to expand their requirements for documentation, coding accuracy, and medical necessity. Manual workflows make it difficult to apply these rules consistently, especially when regulations shift or when organizations manage multiple payer types.
- Workforce Strain and Productivity Gaps: Labor shortages limit the ability of teams to keep pace with rising claim volumes. This results in backlogs and slower claim progression. RPA helps maintain throughput by handling routine activity so staff can focus on tasks that require review and decision making.
This environment creates a strong need for technology that supports accuracy, speed, and consistency. RPA addresses this need by automating rule based tasks and allowing teams to focus on coding quality, denial prevention, and financial performance.
How RPA Works in Healthcare Claims and Billing Workflows
RPA uses software bots to complete routine digital tasks that follow clear, predefined rules. These bots perform actions such as entering data, retrieving information, and navigating applications. In claims processing, this allows many structured steps to be handled automatically instead of relying on manual effort.
RPA follows consistent logic across systems, which makes it effective in environments with multiple platforms. Bots can move through payer portals, capture information from EHR screens, fill required fields, and transfer data without needing system integration changes.
In practice, RPA supports claims teams by:
- Logging into systems to collect or confirm information
- Entering claim details into required forms
- Gathering fields needed for billing and documentation review
- Checking claim progress across payer websites
- Routing items to the correct work queues
When combined with AI tools that interpret clinical documentation and support coding accuracy, RPA becomes part of a connected workflow that improves claim readiness and reduces manual touchpoints before submission.
Interested in reducing manual claim-preparation work across your RCM team? Explore how AI and RPA can work together to improve accuracy, strengthen compliance, and reduce avoidable denials.
Benefits of RPA for Healthcare Claims Processing
RPA delivers targeted improvements across the claims lifecycle, especially in areas where accuracy, timing, and payer compliance influence reimbursement.
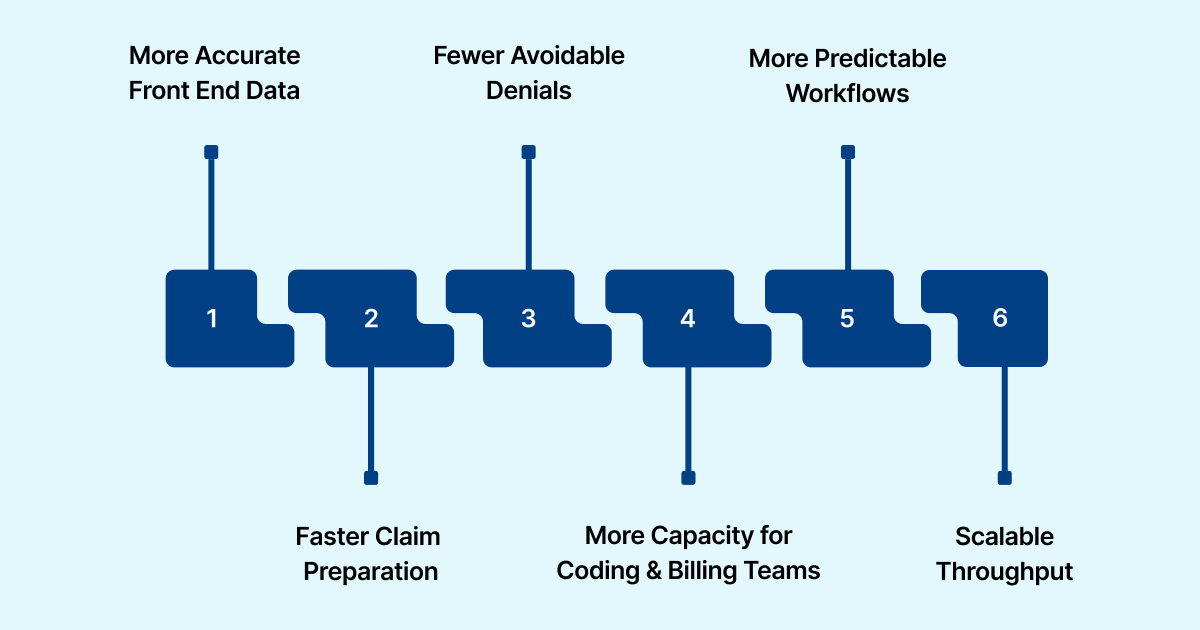
- More Accurate Front End Data: RPA verifies coverage details, patient identifiers, and required fields before a claim reaches coding or billing. This prevents avoidable rejections linked to eligibility and demographic errors.
- Faster Claim Preparation: Bots collect information from the EHR, payer portals, and registration systems, which shortens the time it takes to assemble a complete claim file. This is particularly useful for high volume specialties and multi-site environments.
- Fewer Avoidable Denials: RPA helps ensure required data is present before submission. Examples include confirming active coverage, confirming referring provider details, and validating that required attachments or notes are included. These steps support higher first pass acceptance.
- More Capacity for Coding and Billing Teams: RPA removes repetitive tasks such as data copying, field checks, and routine portal lookups. Teams can focus on reviewing documentation, coding accuracy, and complex claim scenarios that need human judgment.
- More Predictable Workflows: RPA executes the same steps every time, which supports consistent claim preparation. This helps organizations maintain compliance with payer rules and reduces the variation that often leads to inconsistent outcomes.
- Scalable Throughput: RPA keeps claim preparation stable during periods of higher patient volume or reduced staffing. Bots continue to process queues in the background, which helps maintain timely submission.
RPA Use Cases Across the End-to-End Claims Lifecycle
RPA supports specific steps within the claims lifecycle that require accuracy, timing, and consistent application of payer requirements. These use cases focus on tasks that directly influence whether a claim is complete, properly assembled, and ready for submission.

- Claim File Assembly: RPA can combine information from clinical, financial, and scheduling systems to create a complete claim package. This includes retrieving encounter details, pulling charge data, and confirming that required fields are populated before the claim enters billing review.
- Attachment Collection and Upload: Some payers require supplemental documents such as operative notes, imaging reports, or progress summaries. Bots can retrieve these files and upload them to payer portals or clearinghouse systems as needed. This reduces delays that occur when attachments are missing.
- Verification of Claim Configuration: Many claims require specific payer or service level configurations, such as modifiers, place of service indicators, or billing provider details. RPA can check these values against internal rules and flag mismatches for staff review.
- Secondary and Tertiary Claim Preparation: Bots can assist in creating secondary or tertiary claims by pulling payment information from primary payers, applying the correct coordination of benefits logic, and preparing the subsequent claim for submission.
- Encounter to Claim Alignment: RPA can compare documented services with those included on the claim and route exceptions to coding or billing teams. This helps prevent underbilling, missing services, or inconsistencies between documentation and billed items.
- Claims Queue Management: Bots can organize claims into work queues based on payer type, service category, or urgency. This helps teams focus on claims that need immediate attention and improves overall throughput.
These targeted use cases help organizations maintain a consistent claims workflow. They ensure that claims move through each step with the required information already in place, reducing the number of items that need correction before submission.
How AI Enhances RPA for Smarter Claims Automation
RPA handles structured, rules based tasks, but many steps in the claims lifecycle require interpretation of clinical information or evaluation of payer requirements. AI addresses these areas by analyzing documentation, identifying coding needs, and highlighting issues that RPA alone cannot detect.
- Interpreting Clinical Documentation: AI tools can read provider notes, diagnostic reports, and procedure summaries to identify relevant clinical details. This supports accurate coding and ensures that claim information is aligned with the documented services.
- Identifying Missing or Incomplete Information: AI can detect gaps that affect coding or billing, such as missing elements in a visit note or incomplete descriptions of procedures. This prompts timely follow up and helps prevent issues that would otherwise require post submission correction.
- Coding and Classification Support: AI can recommend ICD, CPT, or HCC codes based on documentation content. This gives coding teams a more complete starting point and improves the accuracy of claims that require clinical interpretation.
- Predicting Claim Risk: AI can analyze patterns in historical claims and highlight items that are more likely to encounter payer scrutiny. This allows teams to address potential issues before submission.
- Coordinating With RPA: When AI identifies what needs to be corrected or added, RPA can perform the related system actions. Examples include updating fields, routing claims to reviewers, or placing items into specific queues. Together, the two tools create a continuous workflow that supports cleaner claims across all service lines.
AI enhances RPA by expanding automation into areas that require understanding, decision support, or interpretation. This combination provides health systems with a more complete approach to improving claim readiness.
Challenges of Implementing RPA in Healthcare Revenue Cycle
Introducing RPA into claims processing can improve efficiency, but organizations often encounter practical obstacles during planning and deployment. These challenges relate to infrastructure, workflow stability, and long term management of automated processes.
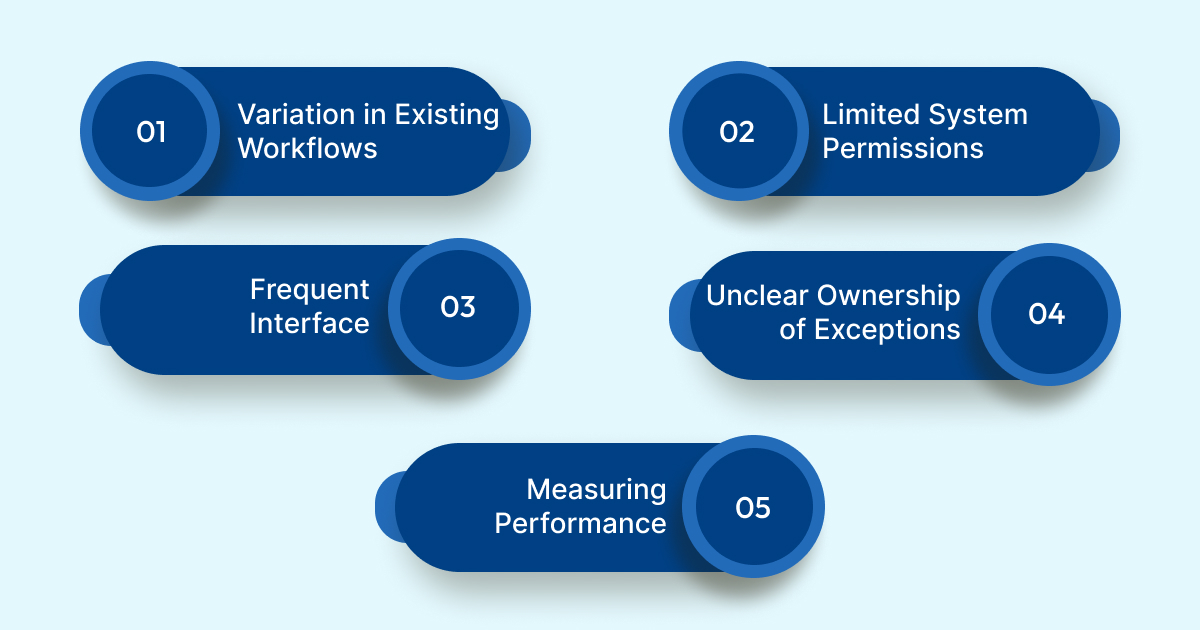
- Variation in Existing Workflows: Claims processes differ across departments, service lines, and staffing models. If workflows are not aligned, bots may behave inconsistently. Successful organizations start by mapping a single standardized process before building automation on top of it.
- Limited System Permissions or Access Controls: Bots need access to the same screens and data that staff use. Some systems restrict automated activity or require additional permissions. Many organizations resolve this by creating dedicated bot accounts with clearly defined access and audit controls.
- Frequent Interface or System Updates: EHR and payer portals often receive updates that change button locations, field labels, or navigation paths. These changes can interrupt automation if they are not monitored. Strong bot governance programs include scheduled reviews and quick update cycles to keep scripts current.
- Unclear Ownership of Exceptions: Bots can identify issues that require human intervention, but teams need a clear structure for handling these exceptions. Organizations that succeed with RPA define roles for reviewing flagged claims, tracking resolution, and updating workflows when patterns emerge.
- Measuring Performance and Value: RPA programs are most effective when they have clear targets. Without defined metrics, teams may struggle to understand the impact on claim readiness or reimbursement. Enterprises that scale RPA successfully track indicators such as cycle times, exception rates, and improvement in clean claim performance.
By addressing these operational factors early, health systems create a stable foundation that supports reliable automation across the claims lifecycle.
How to Implement RPA in Revenue Cycle and Claims Workflows
A structured approach helps organizations introduce RPA into claims processing with predictable results. The following steps outline how revenue cycle teams can plan, deploy, and expand automation across the claims lifecycle.
Step 1: Confirm Process Stability
Before automation begins, teams review the claim related steps to ensure they follow a consistent pattern. This includes verifying task order, identifying dependencies, and confirming that required inputs are available at the right time.
Step 2: Select Processes With Clear Rules
RPA performs best in environments where decisions are based on defined criteria. RCM leaders choose tasks that follow consistent logic and require minimal interpretation. Examples include structured checks, repetitive navigation, and routine data movement.
Step 3: Build a Small Initial Workflow
Teams create a narrow workflow that focuses on a single task group such as preparing claim files or assembling attachments. This helps validate the automation approach and gives staff time to become familiar with the new operating model.
Step 4: Establish a Review Cycle
After the initial workflow is active, teams monitor how often exceptions occur, where delays surface, and how well bots are interacting with different systems. Scheduled reviews allow teams to refine rules and update scripts.
Step 5: Expand Automation to Connected Tasks
Once the initial workflow is stable, RCM leaders extend automation to related steps such as claim configuration checks, secondary claim creation, or encounter alignment. This builds incremental efficiency without disrupting operations.
Step 6: Define Long Term Management
Organizations that scale RPA successfully assign clear responsibilities for bot oversight, rule updates, and performance tracking. This ensures that automation remains reliable as payer programs, internal systems, and documentation patterns evolve.
This roadmap helps teams introduce RPA in a phased and controlled manner, which supports adoption and maintains continuity across billing and coding operations.
How RapidClaims Enhances RPA with AI-Driven Claims Intelligence
RPA improves the consistency of claim preparation, but many key steps still rely on interpreting clinical details, validating documentation, and applying coding rules. RapidClaims strengthens these areas by combining automation with AI driven clinical and coding intelligence.
- AI Supported Coding Accuracy: RapidCode reviews clinical text, identifies relevant clinical concepts, and recommends ICD, CPT, and HCC codes. This helps ensure that claims entering billing contain accurate coding information without requiring manual interpretation.
- Documentation Quality Checks: RapidAssist analyzes provider notes and clinical reports to identify missing elements or unclear descriptions that may affect claim completeness. These checks support stronger claim files before submission.
- Workflow Coordination With RPA: RapidClaims integrates with existing RPA tools, allowing bots to move information, trigger reviews, and route claims based on insights identified by AI. This creates a linked process that improves readiness for submission.
- Integration With EHR and Billing Systems: RapidClaims connects to clinical and financial systems through secure interfaces. This ensures that coding, documentation, and claim preparation activities are supported by accurate data at each step.
Together, these capabilities help organizations produce more complete and compliant claims while maintaining efficient workflows across the revenue cycle.
Ready to streamline claim assembly, coding accuracy, and denial prevention with intelligent automation? Request a RapidClaims demo to see how AI-driven insights can enhance your existing RPA workflows.
Conclusion and Next Steps for RPA-Driven Claims Automation
RPA gives revenue cycle teams a more reliable foundation for preparing claims, but its impact becomes significantly stronger when paired with tools that understand clinical documentation and coding requirements. By combining structured task automation with AI driven insights, organizations can create claims that are complete, accurate, and prepared for payer review with fewer manual steps.
RapidClaims supports this approach by applying clinical intelligence, coding expertise, and documentation analysis to the information that RPA moves through the workflow. This creates a claims process that is more consistent, more scalable, and better aligned with evolving payer expectations.
If your organization is evaluating how to strengthen claim preparation, coding accuracy, or documentation reliability, RapidClaims can help you build a more efficient and compliant workflow.
Request a demo to see how RapidClaims supports end to end claims automation and improves performance across your revenue cycle.
FAQs
Q: How is RPA used in healthcare?
A: RPA supports tasks that rely on consistent, rules based steps. In healthcare, this includes retrieving clinical documents, validating registration details, checking payer requirements, organizing work queues, and preparing information needed for coding and billing. It increases accuracy and reduces the time spent on administrative activity.
Q: What is RPA in medical billing?
A: In medical billing, RPA performs structured actions such as assembling claim files, applying billing rules, verifying required elements, attaching supplemental documents, and preparing claims for submission. These steps help billing teams maintain timely workflows and reduce avoidable errors.
Q: How to automate claims processing?
A: Claims processing can be automated by identifying steps that follow predictable rules, such as data collection, claim assembly, configuration checks, and secondary claim creation. RPA handles these activities, while AI tools interpret documentation and support coding decisions. Together they create a more complete and efficient claim workflow.
Q: What does RPA stand for in healthcare?
A: RPA stands for Robotic Process Automation. It refers to software bots that complete structured digital tasks, helping healthcare organizations reduce manual work and maintain consistent administrative processes.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








