Practice Management System vs EMR: Key Differences, Workflows, and 2026 Guide
Healthcare organizations are experiencing greater pressure in 2026 as patient volume rises, documentation requirements expand, and payers increase scrutiny. HFMA reported that claim denials remain more than 20 percent higher than pre pandemic levels, which shows how system design and data accuracy directly affect reimbursement.
For operational and RCM leaders, the key issue is not choosing between a Practice Management System and an Electronic Medical Record. The real challenge is understanding how each system supports specific steps in the encounter lifecycle and how misalignment disrupts coding accuracy, documentation integrity, and payment timelines. Many practices still use these systems independently, which leads to data mismatches, avoidable rework, and slower claim resolution.
This article clarifies the distinct roles of PMS and EMR platforms and explains how proper alignment strengthens scheduling, documentation capture, coding precision, and claim submission. It also highlights how integrated data prepares organizations to use AI supported tools that help reduce denials, improve documentation quality, and support financial stability in 2026.
Key Takeaways
- PMS and EMR systems support different parts of the encounter lifecycle, and both are required for accurate scheduling, documentation, coding, and billing.
- PMS platforms manage administrative and financial workflows that strongly influence clean claim rates and denial prevention.
- EMR systems capture the clinical detail needed to support medical necessity, coding accuracy, and audit readiness.
- Integration between PMS and EMR reduces data mismatches, speeds up claim processing, and provides the foundation for automation and AI.
- AI supported RCM tools such as RapidClaims strengthen coding, documentation quality, and claim validation once PMS and EMR data are aligned.
- Practices that evaluate workflows, improve data standards, and adopt integrated technology gain greater efficiency and stronger financial performance in 2026.
Table of Contents:
- What Is a Practice Management System (PMS)
- What Is an Electronic Medical Record (EMR) System
- PMS vs EMR: Core Differences That Matter to RCM, Coding, and Compliance Teams
- Strengths and Limitations of PMS and EMR Systems
- Why Integration Matters: PMS + EMR Working Together
- How AI Enabled RCM and Coding Automation Add Value
- Implementation Guidance for Healthcare Leaders
- Future Trends for PMS, EMR, and RCM in 2026 and Beyond
- Conclusion
- FAQs
What Is a Practice Management System (PMS)
A Practice Management System manages the administrative and financial workflows that support each patient encounter. In 2026, PMS platforms function as coordinated workflow hubs that control how information moves from intake to billing. Their design influences data accuracy, clean claim rates, and overall revenue performance.
PMS systems rely on structured data and payer rules to give teams a consistent way to manage front end tasks that directly affect reimbursement.
Core PMS functions that matter to RCM
- Verifying demographics and insurance coverage
- Coordinating scheduling and authorization workflows
- Establishing charge entry and encounter setup
- Generating and submitting claims
- Posting payments and reconciling balances
- Producing operational and financial report
These functions determine how dependable the administrative side of the revenue cycle is. Errors such as outdated insurance information or incomplete encounter setup can create preventable denials and unnecessary rework.
Modern PMS platforms also focus on interoperability. They use standards such as FHIR and HL7 to exchange data with EMRs, clearinghouses, and automation tools. This connectivity ensures that administrative data aligns with clinical content, which is necessary for coding accuracy and claim validation.
A strong PMS supports more than front office tasks. It provides the operational stability that coding teams, RCM analysts, and compliance leaders need to maintain predictable workflows and reduce avoidable revenue loss.
What Is an Electronic Medical Record (EMR) System
An Electronic Medical Record system captures and organizes the clinical details of each patient encounter. In 2026, EMRs focus on documenting the information that supports coding accuracy, medical necessity, and audit readiness. They form the clinical source of truth that coders and compliance teams rely on.
Key EMR functions
- Document patient history and current conditions
- Capture assessments, diagnoses, and encounter details
- Manage medications, orders, and treatment plans
- Display lab and imaging results
- Provide templates that standardize provider documentation
- Maintain audit trails for clinical review
These capabilities shape how complete and defensible the clinical record is. Clear documentation reduces coding uncertainty and supports correct ICD 10, CPT and HCC assignment.
Modern EMRs also emphasize data integrity through structured templates, integrated results, and decision support. With interoperability standards such as FHIR, clinical data can move directly into coding, documentation review, and quality reporting workflows.
A strong EMR strengthens the clinical side of the revenue cycle by ensuring reliable documentation that supports accurate coding and reduces compliance risk.
Strengthen documentation and coding accuracy with AI assisted review. Test RapidCode on sample charts.
PMS vs EMR
Although both systems are essential, they serve very different roles in the encounter to claim workflow. For RCM and coding leaders, the most important differences relate to how each platform contributes to financial accuracy, documentation clarity, and compliance. Understanding these distinctions helps organizations identify where gaps occur and how to design more predictable processes.
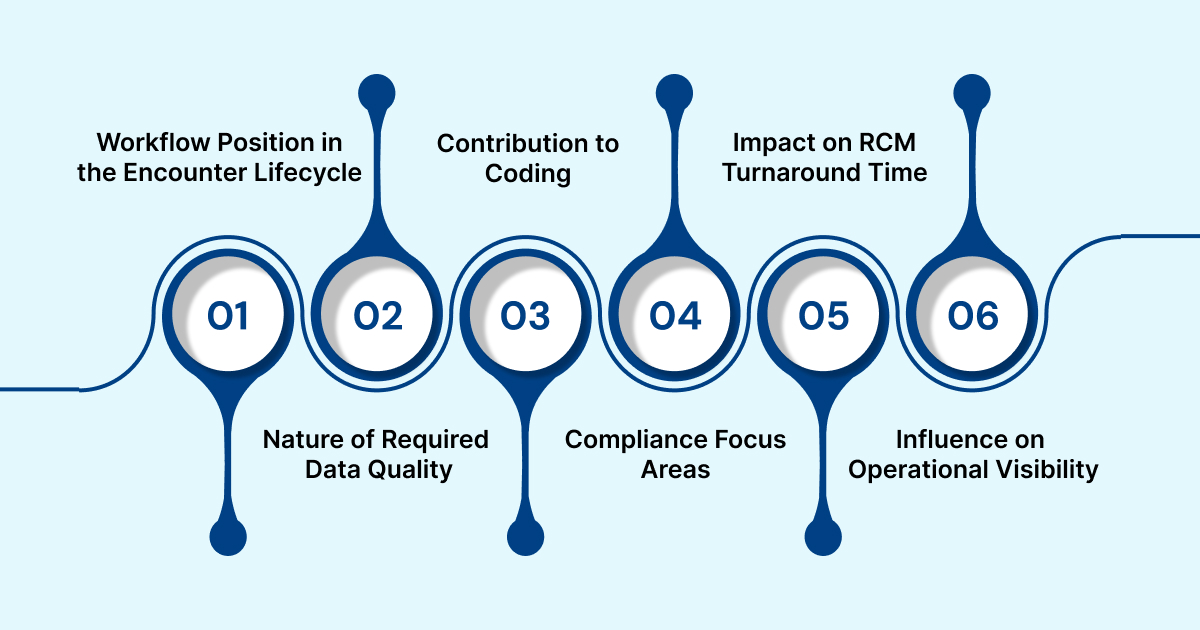
1. Workflow Position in the Encounter Lifecycle
- PMS supports the beginning and end of the encounter. It manages intake, insurance validation, charge setup, claim creation, and payment posting.
- EMR supports the middle of the encounter. It manages clinical data capture, assessment details, documentation, and medical decision making.
This separation determines the sequence in which information moves from a visit to a billable claim.
2. Nature of Required Data Quality
- PMS requires accurate demographic, insurance, and service data to prevent denials or delays.
- EMR requires complete and clinically valid documentation to support medical necessity and coding integrity.
Both types of accuracy impact reimbursement, but they originate from different parts of the workflow.
3. Contribution to Coding
- PMS provides structural inputs such as encounter type, payer rules, and charge data.
- EMR provides clinical content such as conditions, procedures, and provider notes.
Coders rely on both sources to assign correct ICD 10, CPT, and HCC codes.
4. Compliance Focus Areas
- PMS centers on payer requirements, claim formats, and financial record accuracy.
- EMR centers on documentation standards, audit readiness, and clinical justification.
Each platform must meet regulatory expectations, but they support different compliance domains.
5. Impact on RCM Turnaround Time
- PMS affects how quickly claims are created and submitted.
- EMR affects how soon documentation is ready for coding and how often clarifications are required.
Together, they shape the overall speed of the revenue cycle.
6. Influence on Operational Visibility
- PMS provides financial and operational analytics that show cash flow, productivity, and denial trends.
- EMR provides clinical analytics that show documentation habits, provider performance, and care quality indicators.
Leadership relies on insights from both systems to understand full practice performance.
PMS platforms drive the administrative steps that move encounters toward billing. EMR systems capture the clinical detail that supports coding accuracy and compliance. When these roles are clearly understood, teams can design workflows that reduce rework, eliminate gaps, and support automation with high quality data.
Unify PMS and EMR data for faster, cleaner claims. Schedule a RapidClaims integration review.
Strengths and Limitations of PMS and EMR Systems
The table below highlights how PMS and EMR platforms differ in capabilities, constraints, and impact on RCM, coding, and compliance functions.
Why Integration Matters: PMS + EMR Working Together
Integration between PMS and EMR systems creates a continuous flow of information from intake to billing. When these systems operate separately, teams face mismatched data, manual corrections, and delays that weaken RCM performance. Integrated platforms allow practices to move from documentation to coding to claims with fewer interruptions.
Workflow Improvements from Integration
- Administrative details pass directly into the clinical record, reducing data conflicts.
- Documentation becomes available for coding as soon as providers complete the note.
- Charges link more accurately to documented services, lowering the chance of missing items.
- Billing requirements can be applied consistently across both systems.
Benefits for Coding and RCM
- Coders receive aligned clinical and administrative data, reducing clarification cycles.
- Billing teams can release claims faster because required elements are available sooner.
- Denial patterns are easier to evaluate when both systems support uniform data.
- Compliance teams gain clearer visibility into how services were documented and billed.
Role of Interoperability Standards
Modern integration relies on standards such as HL7, FHIR, and structured data formats that allow systems to exchange information consistently. These standards support automation, reduce interface maintenance, and help organizations scale as documentation and billing processes evolve.
Why Integration Matters for Future Automation
AI supported tools depend on clean, connected data. An integrated PMS and EMR environment provides the structured input that automation engines use to verify claims, identify documentation gaps, or support coding decisions. Without integration, these tools cannot operate at their full potential.
Integrated systems create a foundation where clinical accuracy and financial accuracy reinforce one another. This alignment is essential for organizations that want to reduce rework, strengthen compliance, and accelerate revenue cycles in 2026.
How AI Enabled RCM and Coding Automation Add Value
With PMS and EMR data aligned, AI tools can strengthen accuracy and reduce manual work across the revenue cycle. Integrated systems give automation engines the consistent data they need to evaluate documentation, coding, and claim readiness.
Where AI Improves RCM
- Highlights the correct ICD 10, CPT, and HCC codes.
- Identifies missing or unclear documentation.
- Detects mismatches between charges and clinical notes.
- Flags potential risk adjustment opportunities.
- Reviews claims for quality before submission.
Benefits for Teams
- Coders receive clearer, more complete inputs.
- Billing teams spend less time correcting preventable errors.
- Leaders gain insights into documentation patterns.
- Compliance teams benefit from more consistent validation steps.
How RapidClaims Supports These Improvements
- RapidCode improves coding accuracy.
- RapidScrub reduces denial risk.
- RapidRecovery supports denial recovery and appeal prioritization.
- RapidCDI strengthens documentation quality.
Together, these tools use integrated PMS and EMR data to shorten cycle times and support more reliable reimbursement.
Boost coding productivity and cut denials with AI. Start a RapidClaims demo session.
Implementation Guidance for Healthcare Leaders
Successful adoption of PMS, EMR, and automation tools requires a structured approach. Leaders need clear steps to evaluate current workflows, identify gaps, and prepare teams for new processes. The goal is to create a reliable environment where administrative, clinical, and coding activities support each other.
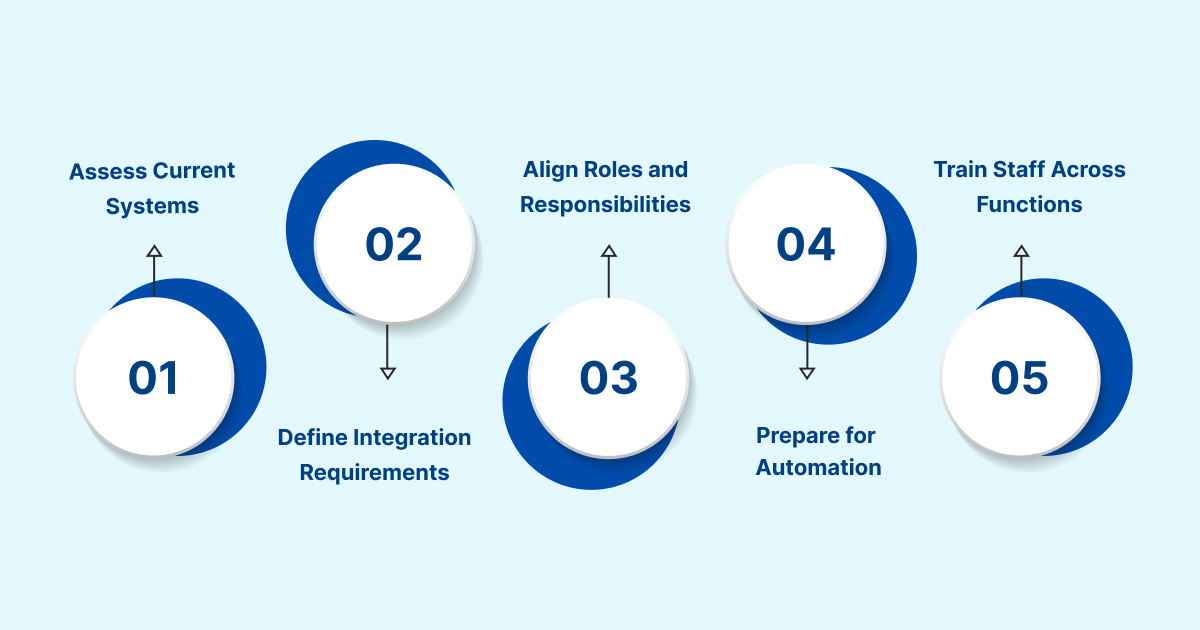
1. Assess Current Systems and Workflow Maturity
- Map how patient information moves from intake to billing.
- Identify bottlenecks such as repeated entry, unclear documentation, or delayed coding.
- Review data quality issues that affect claim accuracy.
2. Define Integration Requirements
- Confirm which data must flow between PMS and EMR systems.
- Ensure compatibility with interoperability standards such as HL7 and FHIR.
- Validate how payer rules and clinical content will be shared.
3. Align Roles and Responsibilities
- Clarify what administrative teams handle versus what clinical teams capture.
- Set expectations for timely documentation and charge review.
- Establish coding review processes that fit the new workflow.
4. Prepare for Automation
- Identify tasks that create the most rework or delays.
- Determine which automation tools can support coding, documentation checks, or denial prevention.
- Verify that data sources provide the structured inputs needed for AI tools.
5. Train Staff Across Functions
- Provide onboarding that explains how integrated workflows reduce errors.
- Offer role based training to ensure consistent documentation and charge entry.
- Reinforce compliance standards associated with ICD 10, CPT, and HCC coding.
A thoughtful implementation process helps organizations achieve smoother workflows, more predictable claims, and better financial performance as they modernize their systems in 2026.
Future Trends for PMS, EMR, and RCM in 2026 and Beyond
Healthcare technology is shifting toward more connected and intelligent systems. As practices look ahead, several trends will influence how PMS, EMR, and RCM teams operate. These trends focus on greater data consistency, stronger analytics, and increased support for value based care.
1. Growth of Unified Platforms
More vendors are consolidating PMS and EMR features into unified ecosystems. These platforms provide a single environment for scheduling, documentation, coding, and billing, which reduces fragmentation and simplifies oversight.
2. Expansion of AI in Clinical and Financial Workflows
AI tools are becoming more common in documentation review, coding assistance, claim validation, and risk adjustment support. Organizations are beginning to rely on automation for early detection of issues that affect payment.
3. Increased Emphasis on Data Quality
Payers and regulators are raising expectations for accuracy across clinical and administrative data. High quality inputs are necessary for coding precision, audit readiness, and population health reporting.
4. Rising Need for Interoperability
HL7, FHIR, and API based integrations are becoming standard as practices coordinate with external partners, specialty networks, and ancillary services. Better connectivity will support cleaner coding and faster claim workflows.
5. Stronger Alignment with Value Based Care
As reimbursement models continue to shift, practices need systems that support accurate documentation of chronic conditions, performance measures, and risk factors. This requires tight coordination between clinical detail and financial reporting.
These trends point toward an environment where well integrated systems and automation tools work together to improve efficiency, reduce rework, and support more stable revenue cycles.
Future proof your coding and RCM workflows. Explore RapidClaims automation options.
Conclusion
PMS and EMR systems play different but equally important roles in the encounter to claim lifecycle. PMS platforms support the administrative steps that drive accurate billing, while EMRs capture the clinical detail needed for correct coding and compliance. When these systems work together, organizations gain clearer documentation, stronger coding accuracy, fewer delays, and a more predictable revenue cycle.
Integrated workflows also create the foundation for AI supported tools that help teams identify documentation gaps, prevent denials, and maintain coding integrity across ICD 10, CPT, and HCC requirements. Practices that invest in aligned systems are better positioned to improve efficiency, reduce rework, and support financial stability in 2026.
If your organization is exploring how automation can strengthen documentation, coding accuracy, and claim quality, request a RapidClaims demo to see how AI can support your RCM team at every step of the workflow.
FAQs
Q: What is a practice management system?
A: A practice management system handles the administrative and financial operations of a healthcare organization. It manages registration, scheduling, insurance checks, charge entry, claims, and payments to support a stable revenue cycle.
Q: What is the main difference between EHR and EMR?
A: An EMR stores clinical documentation for a single practice, while an EHR is designed to share clinical information across multiple providers and care settings. EHRs support broader care coordination and interoperability.
Q: What is the difference between EMR and practice management system?
A: An EMR captures clinical details such as history, diagnoses, and treatment plans. A practice management system handles scheduling, insurance tasks, and billing activities that support claim accuracy and reimbursement.
Q: What is an EHR or practice management system?
A: An EHR stores and organizes clinical information used for care decisions. A practice management system manages the business processes that support scheduling, billing, and reimbursement.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








