Future of Healthcare Revenue Cycle Management in 2026: Key Trends

72% of healthcare executives say their top priority for the next year is investing in technology like automation and AI. Revenue cycle leaders, including compliance officers and billing leads, face rising claim denials, inconsistent reimbursements, and heavy administrative pressure that threaten financial stability across their organizations.
If you’re part of an RCM team, whether at a healthcare IT & digital transformation leadership role or within a medical billing company, you know the daily strain of managing billing accuracy. Every missed claim or delay feels like a setback, and finding reliable ways to reduce friction has become an urgent goal.
In this blog, we’ll explore key RCM trends for 2026, including AI-driven automation, predictive analytics, patient-focused billing, and connected systems improving financial and operational outcomes.
TL;DR
- AI in RCM: Automates tasks like coding, validation, and appeals.
- Unified Systems: Consolidates data to improve communication.
- Ambulatory Care: RCM systems support faster payment cycles for outpatient services.
- Predictive Analytics: Anticipates payment issues and claim trends.
- Patient-Centered Billing: Improves clarity and patient control over billing.
Table of Contents:
Introduction
Emerging Trends in Healthcare RCM
RCM Challenges Facing Healthcare Organizations
Stay Future-Ready with RapidClaims
6 Key Trends Shaping the Future of Healthcare RCM
Healthcare revenue cycle management is shifting as organizations, including physician group administrators and revenue cycle professionals, adopt automation, predictive tools, and patient-centered systems. These changes aim to reduce administrative burden, improve accuracy, and enhance financial outcomes.
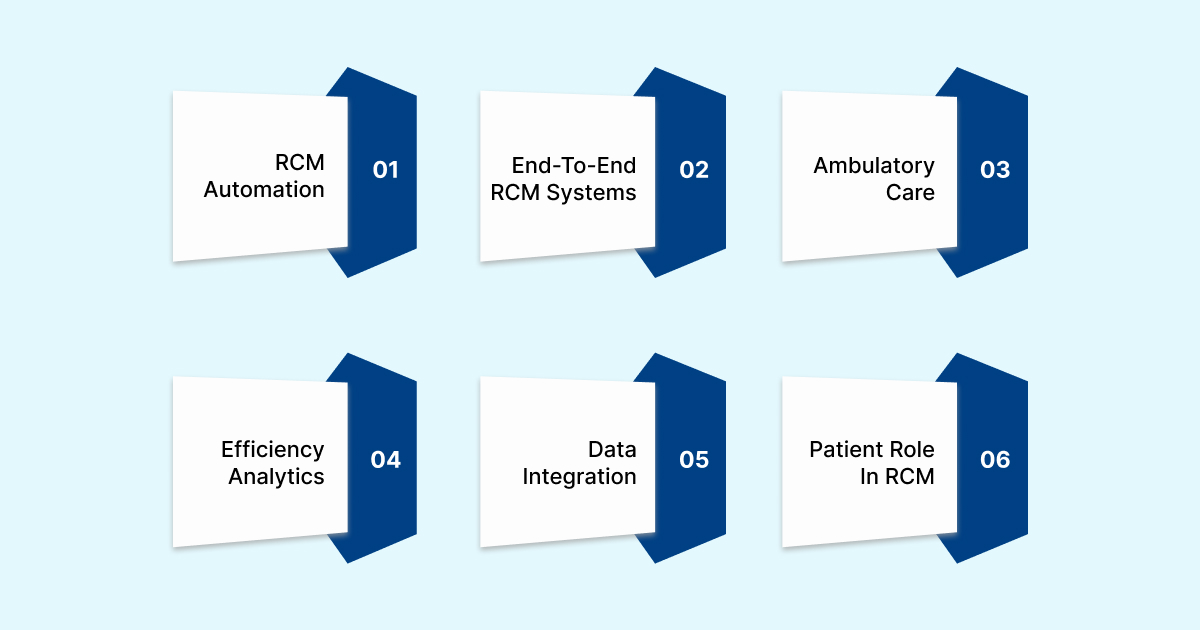
The following trends highlight how technology is reshaping the revenue cycle.
1. AI-Driven Automation in RCM
AI-driven automation is changing how RCM teams handle repetitive and time-consuming processes such as coding, billing, and claim follow-ups. The global AI in the medical coding market is projected to grow from USD 2.4 billion in 2023 to more than triple by 2033.
Below are key areas where AI is driving measurable
- AI Assistance in Coding and Claims: AI automates coding, claim validation, and documentation, increasing accuracy and freeing up staff for more complex tasks.
- Real-Time Payer Rule Compliance: AI ensures claims meet payer-specific rules instantly, reducing denials and enhancing reimbursement rates.
- Automated Appeals: AI identifies denial trends and auto-generates appeals, speeding up claim recovery and improving success rates.
- Continuous Policy Updates: Machine learning systems update payer rules automatically, helping teams maintain compliance without manual intervention.
2. End-to-End RCM Systems
Many organizations are transitioning from fragmented processes to fully connected RCM platforms that unify patient access, billing, and collections. Here are key benefits driving this shift:
- Unified Data Access: Integrated platforms link clinical and financial data, creating a single source of truth across departments.
- Consistent Operations: Centralized workflows eliminate duplication and foster better communication between teams.
- Scalability and Cost Efficiency: These systems help organizations manage growth while reducing operational costs.
3. Focus on Ambulatory Care
The healthcare industry’s shift toward outpatient and ambulatory services demands RCM models that can handle higher volumes and faster payment cycles. Here are the main priorities for this growing sector.
- Tailored Workflows: Systems designed for outpatient coding and documentation ensure accurate charge capture and billing.
- Improved Billing Accuracy: Automation reduces missed charges, speeding up the billing process and improving accuracy.
- Enhanced Patient Access: Digital tools simplify scheduling, payments, and communication, fostering better patient relationships.
4. Predictive Analytics for Efficiency
Predictive analytics gives healthcare teams better foresight into revenue patterns, claim trends, and payment timelines. Here are key ways these tools are improving decision-making.
- Payment Forecasting: Predictive tools help forecast delays and cash flow issues, enabling early intervention.
- Denial Prevention: Analytics identify high-risk claims, reducing the likelihood of denials before submission.
- Improved Performance Monitoring: Data insights highlight process bottlenecks, enabling teams to make informed adjustments.
5. Data Integration and Interoperability
Data sharing remains a persistent challenge in RCM, with many systems still operating in isolation. Below are the core benefits of achieving better data connectivity
- Connected Data Flow: Integrated systems link clinical and financial data, improving visibility and decision-making.
- Faster Approvals: Real-time access to data accelerates approvals and reduces billing delays.
- Improved Compliance: Standardized data exchange helps ensure accurate reporting and audit readiness.
6. The Evolving Role of the Patient in RCM
Patients now expect greater clarity, convenience, and control in their financial interactions with healthcare providers. Here are the main trends driving a more patient-centered approach.
- Patients as Consumers: RCM strategies now treat patients as active participants in their financial processes.
- Transparent Billing: Clearer billing statements and digital payment options reduce confusion and improve the patient experience.
- Proactive Patient Education: Automated reminders and educational tools encourage timely payments and enhance patient satisfaction.
These trends illustrate how automation, AI, and a focus on patient needs are shaping the future of healthcare RCM, making it more efficient and patient-friendly.
Learn how RapidClaims helps groups improve chart review, reduce delays, and support staff with AI assistance. Schedule a demo for a closer look.
What’s Holding Back Healthcare RCM? Key Challenges in 2026
While technology offers significant potential to improve RCM, many organizations still face critical challenges that slow progress. These obstacles include resource limitations, complex payer requirements, and cybersecurity concerns.

Below are the main challenges that healthcare providers must address to ensure their RCM processes run smoothly.
- Staffing and Resource Allocation
The increasing demands on RCM teams make it difficult to maintain the necessary staffing levels and skillsets. Key points include:
- Staffing Shortages: Many organizations face difficulties in recruiting and retaining skilled staff, leading to increased workload and potential burnout.
- Skill Gaps: As RCM processes become more complex, the need for specialized skills increases. Training staff for these changes can be time-consuming and expensive.
- Overburdened Teams: With limited resources, teams often struggle to keep up with the growing volume of claims and administrative tasks, leading to delays and inefficiencies.
- Proactive Denial Management
Denials continue to be a major challenge in healthcare revenue cycles, often creating significant delays in payment and operational disruption. Here’s why proactive claim denial management is crucial:
- High Denial Rates: Many claims are rejected due to missing information, coding errors, or misinterpretation of payer requirements.
- Reactive vs. Proactive: Organizations often address denials only after they occur, which results in longer resolution times and lost revenue.
- Manual Appeal Processes: The time spent on appeals can be draining, especially when manual processes are involved and result in inconsistent outcomes.
- Cybersecurity Risks
With increasing reliance on digital tools and systems, protecting sensitive patient and financial data is a critical challenge. Below are key concerns related to cybersecurity in RCM:
- Data Breaches: Cyberattacks and data breaches expose sensitive information, leading to financial losses, legal penalties, and damaged reputations.
- Compliance Issues: Healthcare organizations must maintain compliance with data protection regulations like HIPAA, requiring constant vigilance and upgrades to security systems.
- Rising Threats: The growing sophistication of cyber threats means organizations must continuously update and monitor their security systems to protect against new vulnerabilities.
These challenges require careful attention and investment to overcome, particularly as organizations look to adopt new technologies. Addressing these concerns will help healthcare providers maximize the benefits of their RCM systems and maintain smooth financial operations.
Stay Future-Ready with RapidClaims RCM
RapidClaim is an AI-powered B2B, enterprise-grade SaaS platform designed to address common challenges in revenue cycle management, including claim denials, coding errors, and operational inefficiencies.
Here’s how it supports revenue cycle operations:
- RapidCode: AI-driven medical coding that processes up to 1,000 charts per minute with 96% accuracy, improving productivity by 170%.
- RapidScrub: Identifies and resolves claim issues before submission, reducing denials by 40% and cutting A/R recovery time by 5 days.
- RapidCDI: Enhances HCC capture by 24%, increases appropriate E&M levels by 18%, and generates an additional $2.2M in revenue annually.
- RapidRules Engine: Applies complex payer rules in real-time, ensuring compliance and optimizing reimbursement with continuous updates.
- RapidAgents: AI assistants automate coding, monitoring, and appeals, saving 2+ hours per day for each team member.
- Eligibility Verification & Prior Authorization: Cuts scheduling time by 70% and achieves 98% first-pass authorization approval.
- Measurable Results: Achieves 98% clean claim rates and 100% audit compliance within 6 weeks, boosting productivity by 1.7x.
RapidClaims helps healthcare organizations address key revenue cycle challenges with AI-powered solutions that reduce manual tasks, improve accuracy, and boost financial performance.
It provides assistance, from coding and denial prevention to documentation, ensuring compliance while driving measurable results.
Book a demo today to see how RapidClaims can improve your revenue cycle management and deliver results in just weeks.
FAQs
1. What are the main benefits of using AI in revenue cycle management?
AI helps reduce the time spent on repetitive tasks, boosts accuracy in coding and claims, and minimizes manual errors that can lead to denials.
2. How does predictive analytics improve RCM?
Predictive analytics helps identify potential payment delays and claim issues early, allowing teams to take preventive actions.
3. Why are patient-centered billing practices becoming more common?
Patients want clearer billing statements and more control over their financial interactions with healthcare providers, which enhances satisfaction.
4. What challenges do healthcare organizations face with RCM automation?
Challenges include staffing shortages, the complexity of payer rules, and the need for continuous updates to automated systems.
5. How can healthcare organizations handle cybersecurity concerns in RCM?
Organizations must continuously update their security measures to protect sensitive patient data and maintain compliance with regulations.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






