Denial AI: Predicting and Preventing Claim Rejections in 2026

Denials are becoming more costly for hospitals and physician groups. A 2025 analysis of payer audits across more than 1.2 million providers and 4,500 facilities showed that the average dollar amount of denied inpatient claims increased by 12 percent, and denied outpatient claims rose by 14 percent compared to prior periods.
This rise in financial impact reflects issues highlighted across leading denial-management research: documentation gaps that affect coding accuracy, authorization errors that occur late in the workflow, and rapidly changing payer rules. These factors make it difficult for teams to detect risk before a claim is submitted.
AI helps address these upstream challenges by reviewing documentation, coding patterns, and payer policies in real time. This gives RCM teams earlier insight into high-risk claims and reduces preventable denials that drive avoidable revenue loss. Healthcare organizations are now turning to AI for denial management to identify documentation gaps, coding risks, and policy mismatches before claims are ever submitted.
Key Takeaways
- Denials are rising due to documentation gaps, coding variability, late authorizations, and shifting payer rules.
- Denial AI predicts high-risk claims by analyzing documentation completeness, code accuracy, and payer policy alignment.
- Machine learning detects patterns linked to common denials; NLP identifies missing clinical elements that impact specificity or medical necessity.
- AI supports denial prevention across eligibility checks, coding, scrubbing, and follow-up prioritization.
- Strong implementation requires clean data, EHR integration, and well-aligned workflows.
- AI tools like RapidClaims automates denial prevention with real-time risk scoring, payer-rule intelligence, and coding/documentation validation.
Table of Contents:
- Root Causes of Claim Denials and Operational Risk Factors
- How Denial AI Identifies High-Risk Claims Upstream
- Denial Prevention Across the Revenue Cycle Using AI
- How to Implement Denial AI Within Existing RCM Workflows
- Benefits of Denial AI for Healthcare Revenue Cycle Teams
- Compliance and Data Quality Requirements for Denial AI
- How RapidClaims Prevents Denials with Real-Time AI
- Conclusion & Next Steps for Denial Prevention
- FAQs
Root Causes of Claim Denials and Operational Risk Factors
Despite steady improvements in documentation workflows and billing oversight, denials continue to arise from issues that are preventable. For most provider organizations, three operational pressures make denials difficult to control at scale.
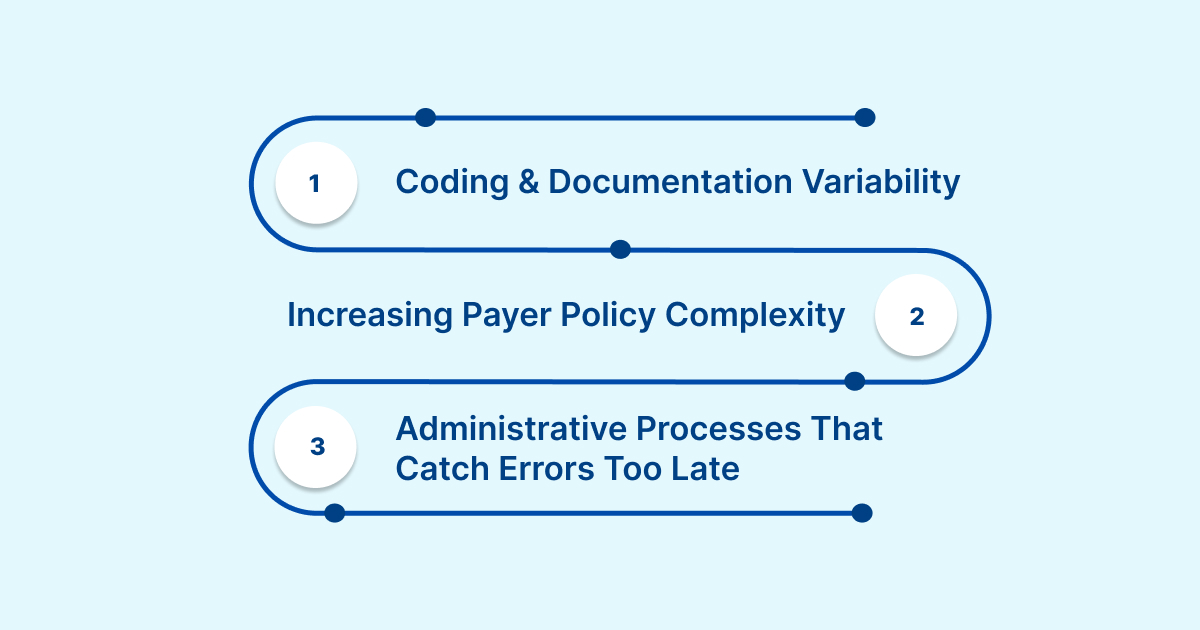
Coding and Documentation Variability
High visit volumes, specialty-specific requirements, and ongoing updates to ICD-10, CPT, and HCC guidelines contribute to inconsistent coding. Even small discrepancies in clinical detail or code selection can trigger a denial. These inconsistencies create downstream rework for coding and QA teams and increase the risk of delayed payment.
Increasing Payer Policy Complexity
Payers introduce new rules for medical necessity, coverage limits, authorization, and bundling throughout the year. Keeping internal teams aligned to these rule changes is challenging, especially when multiple payers update criteria at different times. Missed rules or outdated edits often become denial reasons that could have been flagged earlier.
Administrative Processes That Catch Errors Too Late
Traditional workflows detect errors only after a claim moves through coding, billing, and submission. By that point, gaps related to documentation, eligibility, or authorization are already embedded in the claim. Teams must then correct the issue, resubmit the claim, and repeat follow-up, increasing cost to collect.
Together, these challenges explain why denials continue to increase in financial impact and operational burden. The following section outlines how AI identifies these risks earlier in the cycle and supports more reliable claim outcomes.
How Denial AI Identifies High-Risk Claims Upstream
AI brings forward visibility into claim accuracy by analyzing the factors that commonly lead to denials. Instead of waiting for a payer response, AI evaluates each claim during coding and claim preparation and pinpoints issues that increase rejection risk.
Machine Learning Models Identify Denial Patterns
AI models learn from historical claims, payment outcomes, and payer behavior. These models detect patterns linked to common denial categories such as coding errors, missing documentation, noncovered services, or invalid authorizations. The output is a risk profile that highlights claims likely to be rejected if submitted.
Claim-Level Risk Scoring With Real-Time Alerts
Each claim is assigned a risk score that reflects its likelihood of denial. When specific risk thresholds are met, AI generates alerts for coding or billing teams. This allows staff to review claims with the highest financial impact first and correct errors before submission.
NLP Reviews Documentation for Accuracy and Completeness
Natural language processing analyzes encounter notes to confirm the presence of required clinical details and validate code selection. It can identify missing elements such as laterality, specificity, chronic condition status, or procedure details. Early detection of documentation gaps reduces downstream coding errors.
Automated Payer Policy Intelligence
AI systems ingest payer policies such as LCDs, NCDs, prior authorization criteria, bundling rules, and periodic updates. This helps the system identify mismatches between documentation and payer expectations. Teams can correct these issues before the claim moves into the billing queue.
By combining predictive modeling, documentation analysis, and policy intelligence, AI provides a reliable method for identifying high-risk claims earlier in the process. The next section explains how these capabilities support denial prevention across each stage of the revenue cycle.
RapidScrub delivers real-time denial-risk scoring, payer-rule alignment, and automated edit detection; cutting preventable denials by up to 70%. Request a claim-risk assessment and see your top denial drivers instantly.
Denial Prevention Across the Revenue Cycle Using AI
AI improves denial prevention when it is applied across multiple points in the revenue cycle, not only during coding or claim preparation. Each stage contains different risk factors, and targeted AI support helps prevent errors before they accumulate.
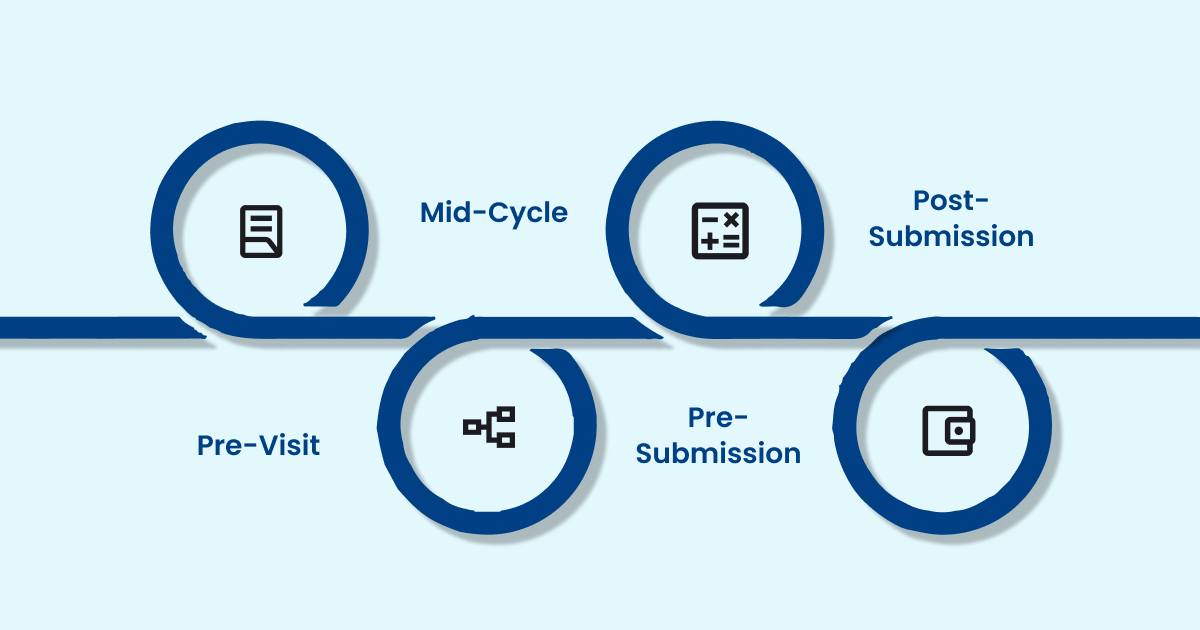
Pre-Visit: Eligibility, Benefits, and Authorization Validation
Eligibility and authorization issues remain among the most common causes of preventable denials. AI can check benefit details, coverage limits, referral requirements, and authorization status against payer data sources. Identifying mismatches before the visit helps prevent claims that would otherwise be rejected for incorrect or incomplete information.
Mid-Cycle: Coding Support and Documentation Quality Checks
During the coding stage, AI can compare encounter documentation with specialty-specific code expectations. It identifies missing clinical elements that affect code validity and surfaces inconsistencies that could lead to medical necessity or specificity denials. These insights support coders without replacing their expertise.
Pre-Submission: Intelligent Claim Scrubbing and Edit Management
Before a claim enters the billing queue, AI can review payer-specific edits, bundling rules, frequency limits, and local and national coverage criteria. This ensures the claim aligns with the most recent payer rules and reduces the chance of denials linked to outdated edits or overlooked coverage requirements.
Post-Submission: Predictive Follow-Up Prioritization
Once a claim is submitted, AI can forecast which claims are most likely to require follow-up based on historical payer behavior and denial patterns. Billing teams can prioritize actions on claims that have a higher probability of delay, shortening resolution time and improving cash flow.
Across each step, AI supports a consistent goal: preventing denials before they occur by identifying risk where it naturally appears in the workflow. The next section outlines how organizations can implement these capabilities within existing RCM operations.
How to Implement Denial AI Within Existing RCM Workflows
Adopting AI for denial prevention requires more than adding a new tool. Provider organizations need clear workflows, clean data inputs, and coordinated collaboration across coding, billing, and IT teams. A structured approach ensures that AI strengthens existing processes without disrupting daily operations.
Integration With EHR and Billing Systems
AI performs best when connected directly to source systems that house clinical, coding, and claim data. Integrations using HL7, FHIR, and X12 allow the AI platform to receive encounter notes, charge data, and claim drafts in real time. This ensures that risk insights appear within the same workflows coders and billers already use.
Data Preparedness for Accurate AI Insights
Reliable prediction depends on high-quality documentation, coding history, and complete claim records. Organizations benefit from reviewing data flows for gaps such as inconsistent note templates, missing code details, or incomplete denial reason codes. Cleaner inputs lead to more accurate risk signals.
Workflow Alignment for Coding, QA, and Billing Teams
AI-driven alerts require defined routing rules. Coding teams may review documentation or specificity issues, while billing teams address authorization or eligibility problems. Establishing clear handoffs prevents delays and ensures that each risk category is resolved by the appropriate role.
Staff Enablement and Adoption
Teams need clarity on how AI supports their work. Training should explain the meaning of risk scores, how to review flagged claims, and when to escalate issues. Organizations that combine AI insights with existing expertise see the strongest improvements in clean-claim rate.
With the right foundation, AI becomes an operational asset rather than a separate process. The next section outlines the measurable benefits RCM and coding teams experience when AI is embedded into daily claim workflows.
Benefits of Denial AI for Healthcare Revenue Cycle Teams
AI strengthens revenue cycle performance by improving accuracy, reducing rework, and giving teams earlier visibility into issues that impact reimbursement. These gains are most evident in organizations managing high claim volume or multiple specialties.
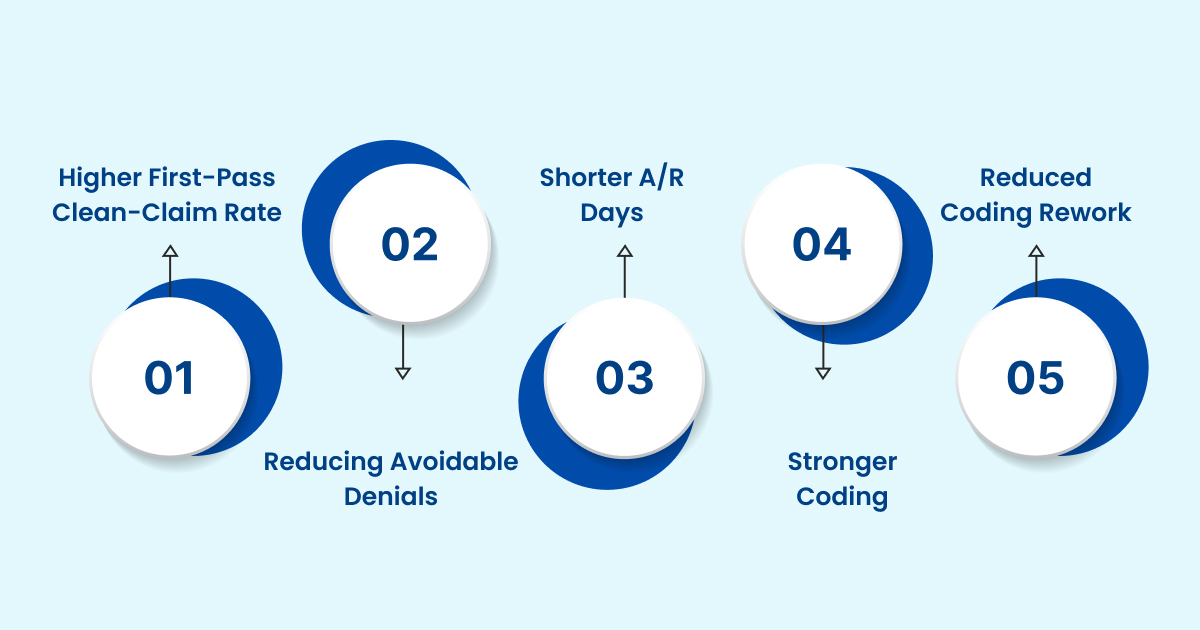
Higher First-Pass Clean-Claim Rate
AI identifies the specific elements that prevent a claim from clearing payer edits on the first attempt. This includes missing chronic condition indicators for HCC-related diagnoses, incorrect modifiers in orthopedic encounters, or insufficient specificity in cardiology and surgical documentation. Addressing these items before submission raises the clean-claim rate and reduces the need for reprocessing.
Reduction in Avoidable Denials
Many denials repeat because the underlying patterns are consistent within each specialty. AI highlights gaps that commonly lead to rejections, such as incomplete medical necessity detail in imaging, missing time documentation in behavioral health visits, or diagnosis-to-procedure inconsistencies in urgent care settings. Preventing these issues lowers the avoidable denial burden that occupies substantial coding and billing time.
Shorter A/R Days
AI predicts which claims are likely to encounter delays based on payer history and encounter characteristics. When teams focus on correcting these claims before submission, adjudication cycles shorten and payment becomes more predictable. This is particularly valuable for payers with variable processing timelines.
Stronger Coding and Documentation Compliance
AI examines documentation to confirm that it supports the assigned codes. It identifies gaps such as missing laterality, incomplete E/M detail, or insufficient postoperative notes. These checks strengthen audit readiness and reduce the likelihood of post-payment recoupments or compliance-related denials.
Reduced Manual Rework for Coding and Billing Teams
With fewer claims requiring correction or appeal, coders and billers spend less time revisiting encounters and more time on complex or higher-value work. This reduces staff fatigue and supports scale without adding new full-time resources.
These operational improvements drive long-term RCM performance. The following section explains the compliance and data-quality requirements that keep denial AI accurate and audit-ready.
Compliance and Data Quality Requirements for Denial AI
Effective AI-driven denial prevention depends on strong operational foundations. As organizations scale AI across coding and billing workflows, several factors influence reliability, compliance, and long-term sustainability.
Federal and Payer Requirements
AI must operate within the boundaries of HIPAA, CMS regulations, and specialty-specific documentation rules. Systems should maintain clear audit trails that show how predictions were generated and which data elements informed each risk indicator. This transparency helps coding and compliance teams validate decisions during audits and payer reviews without losing trust in automated recommendations.
Maintaining Data Quality for Consistent AI Performance
Over time, shifts in documentation patterns, coding practices, or EHR templates can weaken model accuracy. Regular data quality reviews help prevent issues such as missing encounter metadata, inconsistent provider documentation styles, or outdated diagnosis lists from reducing model precision. Continuous monitoring ensures the AI reflects current clinical and billing workflows.
Managing Model Updates as Payer Rules Evolve
Payer requirements change frequently. AI systems must be updated in cadence with revised coverage rules, procedure edits, and medical necessity criteria. A structured update process ensures the AI reflects new policies without disrupting daily operations. This keeps the system aligned with real-time payer expectations and prevents sudden drops in prediction accuracy.
Establishing Secure and Reliable EHR Integration
Strong integration with EHR, PMS, and billing platforms ensures the AI can read encounter data and return insights without duplication or manual import steps. Organizations benefit from integrations that support HL7, FHIR, and X12 standards, enabling the AI to pull structured and unstructured data securely and consistently across clinical and billing environments.
Monitoring Performance Drift Over Time
As care patterns change or new service lines are added, prediction models may drift from their original accuracy. Ongoing performance checks ensure the AI continues to identify denial risk reliably and adapts to clinical and operational shifts. This oversight protects long-term value and reduces the risk of false positives or missed denials.
These considerations help ensure that AI strengthens denial prevention while meeting compliance, technical, and operational expectations.
How RapidClaims Prevents Denials with Real-Time AI
RapidClaims applies AI directly within coding and claim-preparation workflows to prevent denials before they occur. The platform analyzes encounter documentation, code selection, payer rules, and historical claim outcomes in real time. This allows the system to identify the specific elements that place a claim at risk before the claim leaves the door.
- Real-Time Denial Risk Visibility: RapidScrub™ generates claim-level risk indicators as coders and billers work. Teams can see exactly which documentation gaps, code mismatches, or missing elements could trigger a payer rejection. This visibility helps staff correct high-risk claims early in the workflow.
- Documentation and Coding Quality Checks: RapidCode evaluates clinical notes for completeness and specificity. It verifies that ICD-10, CPT, HCPCS, and HCC codes are fully supported by the provider’s documentation. The system identifies missing laterality, incomplete time documentation, and insufficient medical necessity detail to reduce downstream denials.
- Continuous Payer-Rule Alignment: RapidScrub updates its rules engine with the latest payer coverage policies, LCDs, NCDs, bundling rules, frequency edits, and prior-authorization criteria. This ensures claims remain aligned with current payer expectations without relying on manual rule tracking.
- AI-Powered Edit Detection and Smart Scrubbing: RapidScrub applies more than 119 million machine-learned and rules-based edits. These include eligibility checks, coverage validation, and contract-level reimbursement rules. The engine identifies risks that traditional scrubbers overlook, including specialty-specific documentation mismatches, missing HCC context, and diagnosis-to-procedure inconsistencies.
- Seamless Integration With Existing Systems: RapidClaims connects to EHRs, PM systems, and clearinghouses using SMART-on-FHIR, HL7, and X12 integrations. Risk signals and documentation alerts appear inside the workflows coding and billing teams already use, which avoids additional steps or operational disruption.
With these capabilities, RapidClaims helps organizations strengthen clean-claim rates and reduce preventable denials at the point where they originate.
See how RapidClaims delivers 98% clean-claim rates with AI-powered coding, CDI, and denial prevention. Request your personalized demo to see real-time denial-risk scoring.
Conclusion & Next Steps for Denial Prevention
Rising denial costs and increasing payer requirements make early risk identification essential for revenue cycle performance. AI gives organizations the ability to catch issues at the point of documentation or coding rather than after a denial has already occurred. With stronger visibility, fewer errors reach billing, reimbursement becomes more predictable, and teams spend less time on rework.
By applying AI where denial risk first appears, healthcare organizations can protect revenue, support compliance, and strengthen operational stability across the revenue cycle.
Interested in seeing how AI can support your organization’s denial-prevention strategy? Request a short demo of RapidClaims to explore real-time coding and claim-risk insights.
FAQs
Q: What is denial AI in healthcare?
A: Denial AI refers to the use of artificial intelligence to predict, prevent, and analyze medical claim denials. It reviews documentation, code selection, and payer rules to identify issues that may lead to a rejection before a claim is submitted.
Q: How does denial AI help reduce medical claim denials?
A: Denial AI analyzes clinical notes, coding patterns, and payer policies in real time. It flags missing details, mismatched codes, outdated authorization information, and other risk factors so teams can resolve issues early. This lowers preventable denials and improves first-pass clean-claim rates.
Q: Why is denial AI important for revenue cycle management?
A: Denial AI gives RCM teams earlier visibility into errors that typically surface only after payer submission. By detecting denial risk at the documentation and coding stage, organizations reduce rework, shorten A/R days, and create more predictable reimbursement cycles.
Q: Is denial AI accurate?
A: When trained on high-quality data and integrated directly with EHR and billing systems, denial AI can reliably detect patterns associated with rejections. Its accuracy depends on regular updates to payer rules, documentation consistency, and monitoring for performance drift.
Q: How do organizations get started with denial AI?
A: Most organizations begin by integrating denial AI with their EHR or billing system, reviewing data quality, and aligning workflows for coding, QA, and billing teams. Once deployed, the system delivers real-time alerts and risk visibility during claim creation.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








