.webp)
What Is An Additional Diagnosis In Medical Coding And Why It Matters For Reimbursement?

Accurate medical coding forms the cornerstone of effective medical billing systems. One minor but important aspect in medical coding, which is often overlooked, is Additional Diagnosis – secondary conditions that accompany the primary diagnosis. When these conditions are captured and coded accurately, it can lead to fewer claim denials, facilitate better resource allocation and patient care, and timely reimbursements. For modern era healthcare personnel like medical coders, leaders and billing teams, it is crucial to learn and understand their role in streamlining several aspects of the billing and coding process.
In this article, we discuss what an additional diagnosis is, how it affects medical reimbursements, and how critical it is to conduct risk assessments, clinical decision-making, and enhance patient care, and most importantly, ensuring timely reimbursements.
What Is Additional Diagnosis In Medical Coding?
An additional diagnosis is any medical condition apart from the primary diagnosis of a patient. These conditions can be defined as any:
- Pre-existing medical conditions.
- A complication developed along the course of treatment.
- Chronic conditions that affect medical care.
At the time of admission, hospitals record the primary diagnosis – the main condition for which a patient approaches them, as well as any additional diagnosis. This is important to ensure accurate patient care and resource allocation, and most importantly, justified reimbursements marking a successful claim process.
In medical coding, additional diagnosis must not just be mentioned in the documents but must also meet coding criteria, so healthcare establishments can process accurate bills and receive reimbursements that justify the medical care and assistance administered. For this, revenue cycle management systems must be updated with the latest ICD-10 codes for additional diagnoses and hospitals must have proper coding protocols in place to avoid complications in their claim process.
In medical coding, additional diagnoses can be documented accurately if they meet coding criteria, instead of just being mentioned in medical documents.
Why Do Additional Diagnoses Exist in Medical Coding?
A primary reason why medical codes depicting additional diagnosis are relevant is that they help caregivers determine patient complexity and severity of illness while ensuring these conditions are accounted for by their billing teams. This information enables them to allocate the right resources and medication, and declaring them while filing claims eases administrative complications, leading to successful claim cycles. Additional diagnosis in medical coding directly affects a healthcare establishment’s revenue cycle, making it a very crucial aspect to be studied by caregivers and administrators alike. Entering and recording accurate codes during billing is crucial, as healthcare payers don’t reimburse based on symptoms alone, but based on:
- Comorbidities – conditions present before admission.
- Complexities – health issues that arise during the course of treatment.
- Risk adjustment
- Medical necessity
The medical codes for additional diagnosis accurately represent the above, making it easy for caregivers and administrators to record and submit while filing claims, and for the payers to assess the genuineness of the claims, making the process hassle-free and transparent.
Without additional diagnosis, the clinical picture looks incomplete, directly affecting reimbursements and the overall revenue cycle, in turn.
Types Of Additional Diagnosis In Medical Coding
Additional diagnosis involves a plethora of conditions, which, if left unsegmented, could be mistaken for primary diagnosis, causing utter chaos in the billing process. Hence, regulatory bodies clearly distinguish additional diagnosis in the following manner:
- Comorbidities(CC)
Comorbidities are conditions present in a patient before they are admitted for any major condition. Notable examples are diabetes, obesity, hypertension, chronic kidney disease, etc. The Cleveland Clinic describes comorbidities as any medical conditions that coexist alongside a primary diagnosis that can affect a patient’s health and ultimately influence the treatment outcome.
With respect to billing, comorbidities must be accounted for, as these conditions have a direct impact on the treatment outcome and any future course of treatment.
- Complications (MCC/CC)
The ICD-10 defines complications as medical conditions that occur during the course of treatment. These include hospital-acquired infections, post-operative complications, acute kidney injury, etc. Since complications arise once a patient enters the system, hospitals must take the responsibility to document and enter accurate corresponding medical code while filing reimbursement claims. This contributes to transparent funding policies.
- Chronic Conditions Affecting Care
Chronic diseases are a modern crisis that need immediate attention. These are prevalent medical health conditions that patients have had for a long duration, even before the primary diagnosis was made. While it can be difficult to distinguish comorbidities and chronic conditions, the ICD-10 coding system has bifurcated both. Modern-day healthcare billing systems must be programmed to categorize and segregate both, contributing to transparent billing procedures. Chronic conditions must be mentioned, especially if they need constant monitoring or regular medication.
With a significant percentage of today’s population being diagnosed with lifestyle diseases like diabetes and hypertension, identifying and segmenting additional diagnoses is the need of the hour. This activity helps healthcare institutions and hospitals streamline their billing process and limit revenue leakage significantly.
How Additional Diagnosis Impact Reimbursement?
Medicare Severity Diagnosis-Related Groups, or MS-DRGs, are integral to the healthcare billing industry. MS-DRGs ensure hospitals and other healthcare institutions get timely reimbursements. Hence, they have a major influence on several important payment and billing policies taken by healthcare providers. Similarly, additional diagnosis also affects risk assessments, evaluation and management (E/M) coding settings.
Influence On DRG Assignment & Payment Levels
The MS-DRG classification system helps standardise healthcare costs, thereby ensuring fair and timely reimbursement. Additional diagnosis, when captured accurately and assigned the correct severity level, can be encashed, enabling stable revenue flow. DRGs are used to segment hospital cases based on clinical similarity and expected resource consumption.
Accurate MS-DRG grouping can help hospitals save money and ensure quality patient care, contributing to the overall financial well-being.
For example, a patient with pneumonia may fall under the lower-paying category, however, if the patient has additional diagnosis like acute respiratory failure or sepsis, which, when accurately identified, captured, coded and documented, can improve their chances of getting better clinical care and the hospital is reimbursed for the same.
Risk Adjustment & Value Based Reimbursement
Additional diagnoses are integral to risk adjustment models used in medicare advantage and other value-based care programs. In this system, patients are assigned a risk factor or a risk score based on their primary and additional diagnoses. Hence, capturing additional diagnoses plays an important role in determining a patient’s risk score. When they are captured and coded accurately, hospital administrations can assign appropriate codes, ensuring appropriate care to the patient and timely reimbursements to the hospitals.
Support For Medical Necessity & Claim Validation
The presence of additional diagnosis codes helps payers determine the reason behind:
- Why were extra tests ordered?
- Why is a patient’s hospital stay extended?
- Why were higher levels of care required?
These factors affect how payers determine the need for medical necessity. Additional diagnosis codes help them to understand the same, and this contributes to an uncomplicated reimbursement process. Without the accurate codes, claims may seem inaccurate or unsupported, thus causing hard or soft denials. In this context, additional diagnosis codes act as clinical evidence, supporting the intensity of care and assistance provided.
Effect On Evaluation & Management
Evaluation/Management (E/M) codes ensure correct selection of the care procedures, ensuring accurate billing and reimbursement. The complexity of medical decision-making directly influences E/M code selection. These decisions are influenced by:
- Patient complexity and the number of conditions addressed.
- Severity of the conditions.
- Risk associated with patient management for such conditions.
When additional diagnoses are captured accurately in outpatient medical coding, they significantly influence evaluation and management codes, helping payers clearly understand the need for additional medical procedures and resulting in a higher percentage of claim approvals.
How RCM Helps Prevent Revenue Leakages & Improves Claim Denial Rates
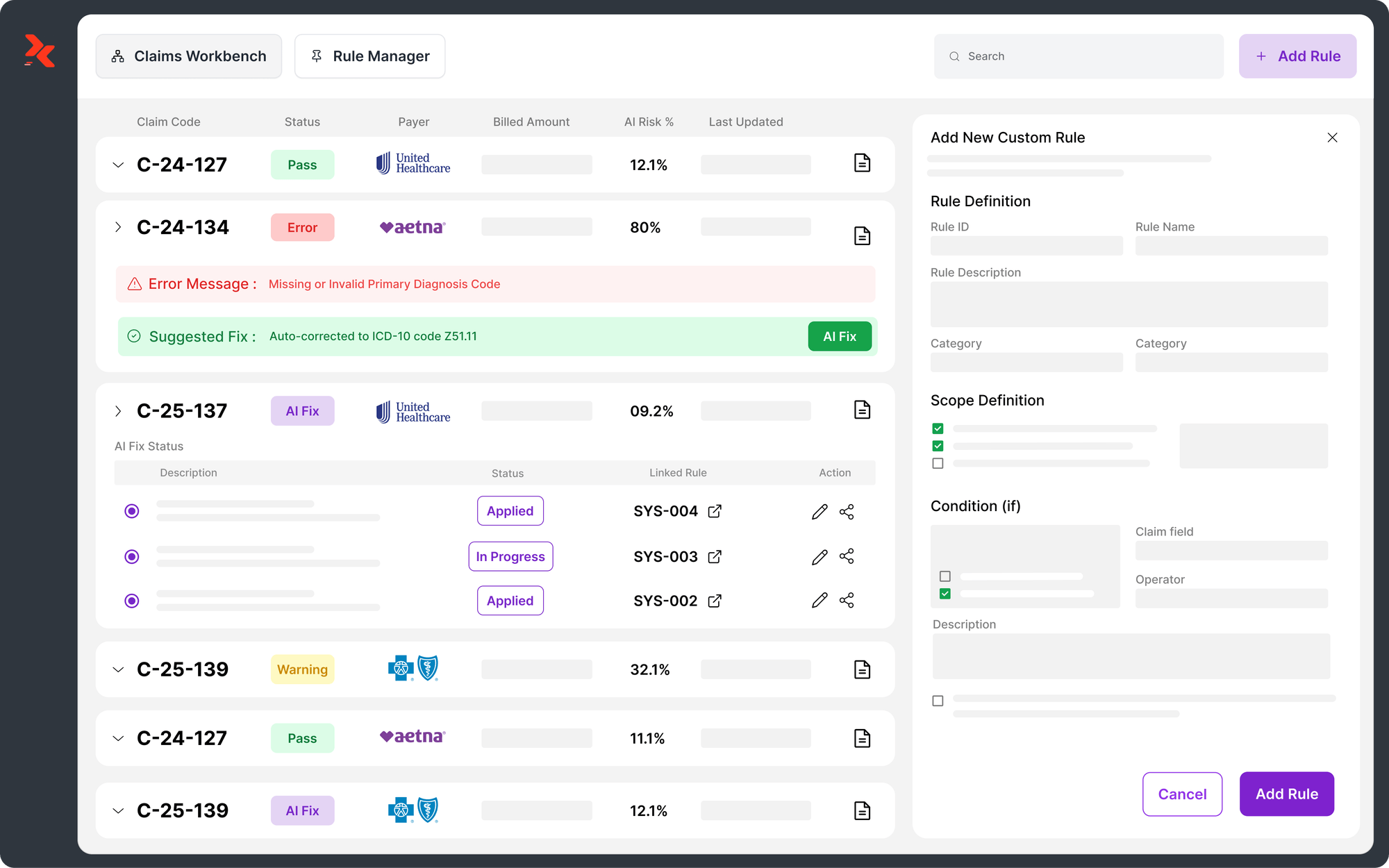
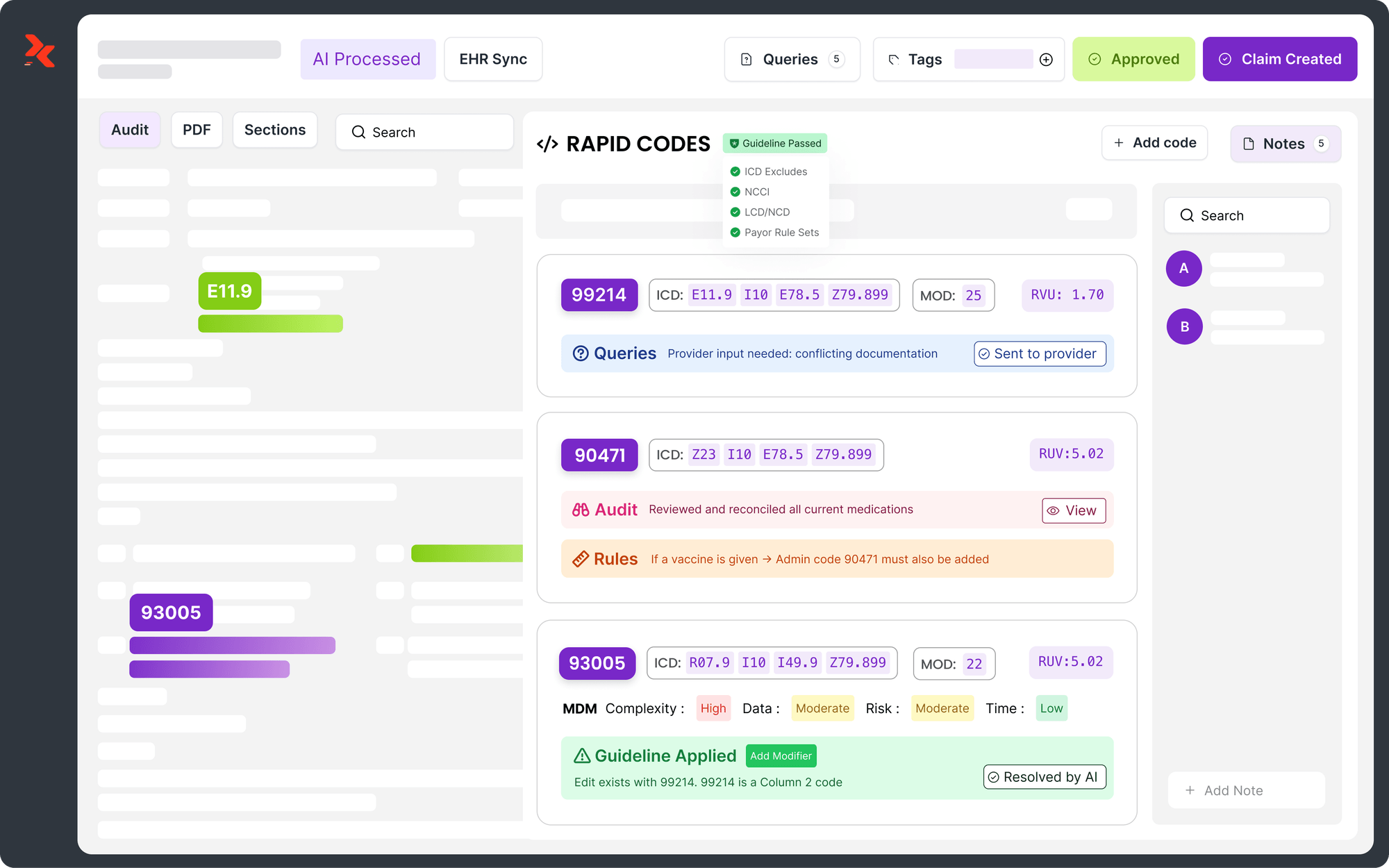
Additional diagnosis codes are integral to the medical system, ensuring that a patient’s primary and secondary health conditions are accurately captured. An RCM system that can automatically capture these details can work wonders. AI-powered RCM systems intuitively go through a patient’s profile and capture primary diagnosis codes and additional codes, parse them into appropriate E/M codes and fill the necessary information that convinces insurance companies about additional clinical and medical actions. This can greatly influence how hospitals get paid.
By leveraging automation and analytics, modern RCM platforms reduce dependence on manual code entry, enhancing the accuracy of patient information. Hospital administrations have the opportunity to make accurate use of this information to ensure that reimbursements are made timely and justify the cost of patient treatment.
Conclusion
An additional diagnosis refers to a secondary medical condition that exists alongside a patient’s primary diagnosis. Often, healthcare billing teams may overlook this critical information and document only the primary diagnosis, leading to inaccurate claims and disrupted revenue flow. An AI Tool for Medical Coding helps ensure that additional conditions are accurately captured and documented in the patient record so that appropriate codes are assigned.
These codes directly influence patient treatment plans, length of stay, and the level of care provided. From an administrative perspective, additional diagnosis codes impact DRG assignments as well as evaluation and management codes, providing insurers with the detailed information needed to approve or deny claims. When additional diagnoses are correctly captured and coded, medical coding accuracy improves—resulting in stronger revenue flow and enhanced patient experiences.
FAQs
How Does Rapid Claims RCM Capture Additional Diagnosis Codes?
Rapid Claims leverages AI to automate code analysis and capture appropriate codes for primary and additional diagnoses. The algorithm is designed to detect additional diagnosis codes. This ensures accuracy, elevated patient care and streamlined billing process.
Do Additional Diagnoses Affect Outpatient & Physician Billing?
Yes, additional diagnosis codes are instrumental in determining a patient’s disease severity which affects the level of care administered. In billing, these codes are used by teams to determine evaluation and management codes, resulting in justified payments to physicians or hospitals.
Can Missing Additional Diagnoses Cause Claim Denials?
Yes, when a patient’s severity level is captured inaccurately, insurance payers may not be fully convinced about treatment durations and additional tests. This may lead to hard denials.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
Related Post
Top Products
%201.png)