.webp)
5 Ways AI Can Simplify Coding for Healthcare Providers


Claim denials are a common headache for U.S. healthcare providers. Around 41% of providers now report a denial rate of 10% or higher, often due to missing or inaccurate claim data, prior authorization problems, incorrect patient registration, and coding errors. These denials slow payments, tie up staff in corrections, and create frustration across billing teams.
Keeping up with frequent CPT and ICD updates, while ensuring every claim is accurate, can be overwhelming. Even experienced coders can make mistakes, and those mistakes can be costly. This is where AI for healthcare coding can be beneficial.
By handling routine coding tasks, checking for errors in real-time, and flagging potential issues before claims are sent out, AI can reduce denials, expedite reimbursements, and streamline the billing process. In this blog, we’ll explore five ways AI enhances healthcare coding, demonstrating how it enables providers to work more efficiently and maintain accurate claims.
Key Takeaways:
- Reducing Errors and Denials: AI analyzes documentation, suggests correct codes, and flags gaps before submission, reducing coding errors and claim denials.
- Streamlining Workflows: Automated coding and pre-submission reviews enable coders to focus on complex cases, thereby improving overall accuracy.
- Maximizing Reimbursements: Clinical documentation improvement and risk adjustment capture ensure claims reflect patient complexity and support appropriate reimbursement.
- Real-Time Compliance: Continuous AI updates and real-time error detection keep coding aligned with evolving CPT, ICD, HCC, and payer rules.
- Implementation Challenges: Staff adaptation, data integration, and workflow alignment can be addressed through training, standardized templates, and AI integration strategies.
- Future Trends: Predictive analytics, telehealth coding, value-based care alignment, cross-specialty optimization, and global standard harmonization are shaping the next phase of coding efficiency and compliance.
Table of Contents:
- Understanding AI in Healthcare Coding
- 5 Ways AI Enhances Coding Accuracy & Reduces Denials
- Overcoming Challenges in AI Implementation
- Future Trends in AI-Driven Medical Coding
- Conclusion
- Frequently Asked Questions (FAQs)
Understanding AI in Healthcare Coding
Healthcare coding goes beyond simply assigning codes to diagnoses and procedures; it’s about ensuring claims are complete, accurate, and submitted on time. In the U.S., nearly $265 billion in claims are denied each year, with coding errors accounting for over 40% of denials and delayed submissions responsible for another 35%. Errors in eligibility, prior authorizations, and documentation further complicate the process, making timely and precise coding a constant challenge for healthcare providers.
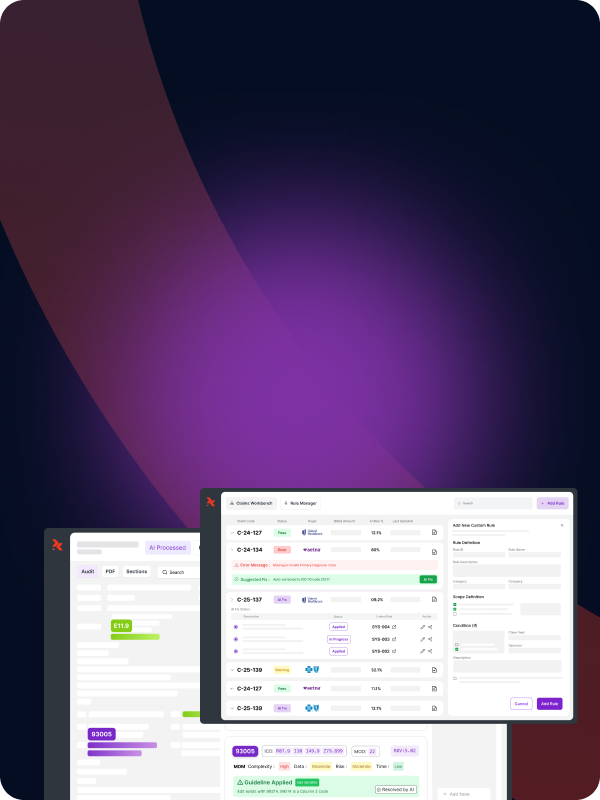
Case Study: How RapidClaims Uses AI to Streamline Coding
Some healthcare organizations utilize AI-driven platforms, such as RapidClaims, to address the $250 billion in U.S. claim denials resulting from coding errors. The AI analyzes patient records, flags missing or inconsistent documentation, and suggests the correct ICD and CPT codes.
For example, if a visit includes both a preventive check-up and a diagnostic test, RapidClaims identifies all relevant services, ensures proper coding, and highlights gaps that could trigger denials. Coders then focus on complex cases while routine tasks run automatically, reducing errors and administrative workload.
This approach demonstrates how AI enhances coding accuracy, streamlines reimbursements, and enables healthcare teams to focus on patient care rather than administrative tasks.
Also Read: Claim Denials: Common Reasons and How to Effectively Resolve Them
With this context in mind, let’s explore five ways AI enhances coding accuracy and reduces denials, showing how technology can transform everyday coding operations.
5 Ways AI Enhances Coding Accuracy & Reduces Denials
A recent study by Bain & Company and KLAS found that 80% of U.S. healthcare providers are increasing investment in IT and software, with AI technologies taking priority. With revenue cycle transformation and automation at the forefront, healthcare teams are exploring how AI can help reduce coding errors, prevent denials, and streamline claims processing.

This sets the stage to see the practical ways AI is improving coding accuracy and efficiency:
1. Automated Code Assignment for Accuracy
Automated code assignment uses AI to read clinical documentation and assign the correct ICD and CPT codes without manual intervention. By analyzing patient records, lab results, and provider notes, the system identifies services and diagnoses that require coding and ensures they align with current guidelines.
Benefits:
- Reduces human errors and inconsistencies in coding.
- Ensures claims are complete and compliant before submission.
- Speeds up the coding process, allowing coders to focus on complex cases.
How to use it:
Healthcare providers can integrate AI-powered coding tools into their EHR or billing systems. Coders review AI-suggested codes, make necessary adjustments, and submit claims with confidence that each code accurately reflects the documented care. Over time, the AI “learns” from adjustments, improving accuracy across future claims.
With RapidCode, AI-driven code assignment doesn’t just save time; it reduces claim denials, boosts productivity by 1.7x, and saves your team 2 hours a day. You can process 1000+ charts per minute while cutting operational costs by 30%, ensuring every claim is accurate and submitted efficiently.
2. Pre-Submission Claim Review
Pre-submission claim review is an AI-driven process that checks medical claims for errors or missing information before they are sent to payers. It examines codes, patient details, and documentation to ensure each claim meets compliance requirements and payer rules.
Benefits:
- Reduces claim denials by catching errors early.
- Speeds up reimbursements by submitting cleaner claims.
- Saves staff time spent on corrections and resubmissions.
- Improves overall revenue cycle efficiency and accuracy.
How to use it:
AI integrates with your billing system to automatically review claims as they are prepared. It flags inconsistencies, missing codes, or documentation gaps, suggesting corrections for coders to approve. Over time, the system learns from coder decisions, becoming more accurate and reducing repetitive errors.
Catch errors before claims are sent with RapidScrub. Its AI-driven pre-submission review helps reduce claim denials by 70%, speeds up A/R recovery by 5 days, processes 1,000+ charts per minute, and cuts operational costs by 30%.
3. Improving Clinical Documentation
Improving clinical documentation involves utilizing AI to analyze patient charts and notes, ensuring they accurately and comprehensively reflect the care provided to patients. The system identifies gaps, missing details, or ambiguous entries that could affect coding, billing, and risk adjustment.
Benefits:
- Enhances the clarity and completeness of medical records.
- Supports accurate coding and proper reimbursement.
- Helps identify high-risk or chronic conditions for better patient management.
- Reduces audit exposure by ensuring documentation meets compliance standards.
How to use it:
AI scans clinical notes and highlights areas that need additional detail or clarification. Healthcare providers or coders can review suggestions, add necessary information, and finalize records. Over time, the AI learns which documentation patterns are most effective, helping maintain consistent and precise records across all patient encounters.
Enhance documentation and RAF accuracy with RapidCDI. Physicians save 30 minutes/day, quality measures improve by 15%, and automated coding protocols deliver $2.2M in optimized reimbursements.
4. Real-Time Error Detection and Streamlined Workflows
AI now allows healthcare organizations to manage claim accuracy and coder efficiency simultaneously. Through real-time error detection and automated workflow management, AI continuously reviews claims as they’re created, analyzing codes, documentation, and patient data to identify inconsistencies or missing details before submission.
At the same time, it automates repetitive tasks and manages pre-submission checks in the background, freeing coders to focus on complex or high-priority cases.
Benefits:
- Catches and corrects coding errors before submission, reducing denials and rework.
- Speeds up claim processing and accelerates reimbursements.
- Reduces administrative workload and manual data entry.
- Ensures consistent accuracy across all claims, even at higher volumes.
- Improves coder productivity without increasing headcount.
How to use it:
AI integrates directly into EHR and billing systems, reviewing claims in real time and flagging discrepancies or incomplete data. Coders can approve or adjust corrections while the system continuously learns from each decision.
Over time, this creates a smoother, more efficient workflow; minimizing bottlenecks, ensuring clean claims, and maintaining high accuracy across every stage of the revenue cycle.
5. HCC and Risk Adjustment Capture
HCC (Hierarchical Condition Category) and risk adjustment capture uses AI to identify chronic conditions, comorbidities, and other patient risk factors from clinical documentation. The system ensures that all relevant diagnoses are coded accurately for proper risk-adjusted reimbursement.
Benefits:
- Improves the accuracy of risk scores and RAF (Risk Adjustment Factor)
- Ensures providers are reimbursed appropriately for patient complexity
- Supports compliance with CMS guidelines
- Reduces missed revenue opportunities due to incomplete documentation
How to use it:
AI scans clinical notes, lab results, and prior encounters to detect conditions that may be under-coded. Coders review flagged entries and confirm or update codes. Over time, the system learns patterns for more accurate predictive capture, helping to maintain consistent RAF scores across patient populations.
AI can enhance coding accuracy and efficiency, but integrating it into existing systems presents challenges, including data compatibility, staff adaptation, and ensuring compliance alignment. Knowing these hurdles helps ensure a smoother implementation.
Overcoming Challenges in AI Implementation
Even with the use of AI, claim rejections and delays continue to be a concern. In 2025, rejection or delay rates are estimated at 10‑20%, often stemming from incomplete documentation, policy misalignment, or coding inconsistencies. While AI can flag potential errors, healthcare organizations still face hurdles in adapting workflows, training staff, and ensuring data quality.
Understanding these challenges is crucial to the effective adoption of AI. Below, we outline common obstacles and practical strategies to address them:
Ready to turn AI implementation into measurable results? With RapidClaims, healthcare teams can achieve a 98% clean claim rate, go live and realize value in just 6 weeks, maintain 100% audit compliance, and save 2 hours daily!
With implementation challenges addressed, the focus shifts to the future. AI is poised to automate more tasks, adapt to new regulations in real-time, and provide predictive insights to enhance coding accuracy and revenue performance.
Future Trends in AI-Driven Medical Coding
AI is increasingly embedded in healthcare coding, going beyond basic accuracy checks to anticipate issues and enhance overall claim quality. In 2025, predictive analytics in fraud detection improved by approximately 28%, enabling insurers to identify and prevent fraudulent life insurance claims.
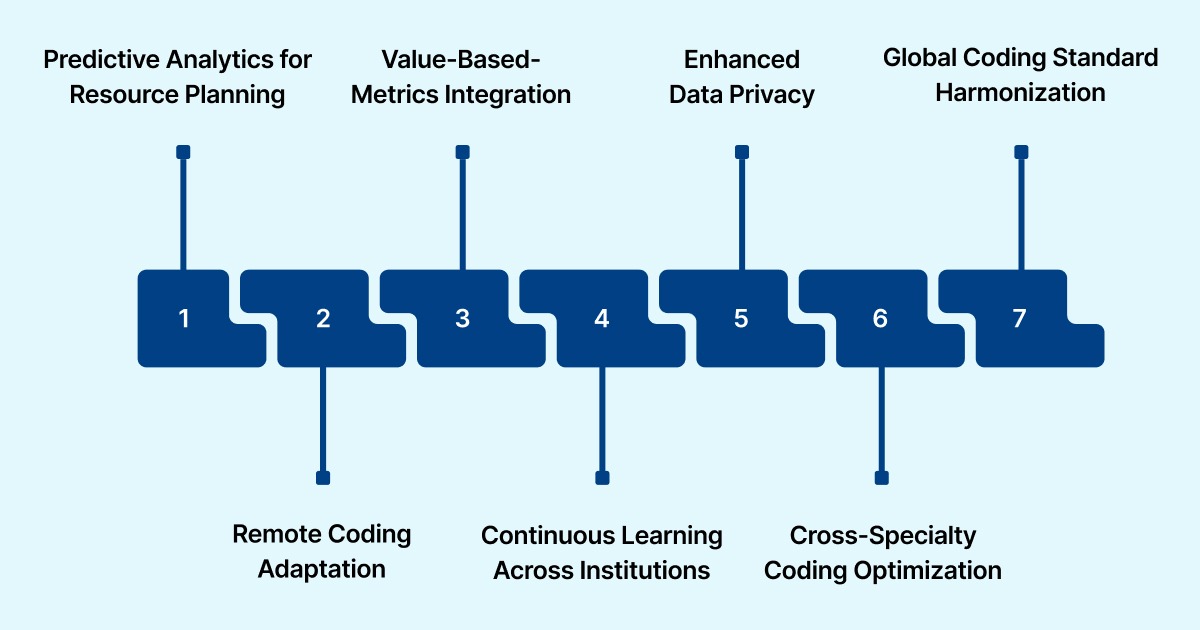
Alt text:Future Trends in AI-Driven Medical Coding
Similar AI capabilities are now being applied to medical coding, allowing organizations to catch anomalies, ensure compliance, and streamline claim validation before submission.
With these advancements, several emerging trends are shaping the next phase of AI in healthcare coding:
1. Predictive Analytics for Resource Planning
AI will not just prevent denials but forecast staffing and resource needs, helping organizations allocate coders where demand is highest.
2. Telehealth and Remote Coding Adaptation
With telemedicine expanding, AI systems are evolving to accurately code virtual visits and remote patient encounters, which often involve unique documentation nuances.
3. Integration with Value-Based Care Metrics
Beyond coding accuracy, AI will increasingly assist in aligning coding practices with quality reporting and outcomes-based reimbursement models.
4. Continuous Learning Across Institutions
AI platforms will leverage aggregated, anonymized data from multiple providers to enhance coding suggestions, ensuring they stay current with emerging treatments and procedures.
5. Enhanced Data Privacy and Compliance Monitoring
AI will play a bigger role in ensuring HIPAA compliance and detecting potential data breaches or unauthorized access in coding workflows.
6. Cross-Specialty Coding Optimization
AI will specialize in complex fields such as oncology, mental health, and chronic disease management, ensuring that nuanced codes are accurately applied across diverse medical specialties.
7. Global Coding Standard Harmonization
As the adoption of ICD-11 grows internationally, AI tools will help U.S. providers align with global coding practices, facilitating smoother cross-border care and reporting.
Also Read: From Chaos to Clarity: How AI in Medical Coding Enhances Accuracy
Conclusion
AI is no longer just a tool for efficiency; it’s becoming a cornerstone for accurate, timely, and compliant healthcare coding. By addressing common pain points such as coding errors, delayed submissions, and incomplete documentation, AI helps providers reduce claim denials, expedite reimbursements, and alleviate the administrative burden on coding teams.
Platforms like RapidClaims demonstrate how AI can seamlessly integrate into the revenue cycle, handling routine coding tasks while allowing coders to focus on complex cases. With ready-to-use AI, rapid deployment, and continuous updates to stay aligned with payer policies, providers can achieve measurable improvements in both accuracy and workflow efficiency.
For healthcare organizations looking to enhance coding precision, optimize reimbursements, and maintain full compliance, exploring AI solutions is no longer optional; it’s essential.
Request a free demo today and see how a complete AI-powered revenue cycle platform can transform your claims process while keeping your team in control.
Frequently Asked Questions (FAQs)
1. What is AI for healthcare coding, and how does it work?
AI for healthcare coding utilizes machine learning and natural language processing to read clinical documentation, assign accurate ICD and CPT codes, and flag potential errors before claims are submitted, thereby helping to reduce denials and improve reimbursement speed.
2. How can AI reduce claim denials?
AI checks for coding errors, missing documentation, and inconsistencies in real-time. By catching these issues before submission, it minimizes the risk of claim rejections, ensuring faster approvals and fewer resubmissions.
3. Will AI replace human coders?
No. AI handles routine coding tasks and error detection, allowing coders to focus on complex or nuanced cases. Human oversight ensures that claims remain accurate, compliant, and contextually appropriate.
4. How quickly can healthcare organizations see results from AI coding platforms?
With ready-to-use AI platforms like RapidClaims, organizations can achieve measurable improvements in coding accuracy, claim turnaround, and operational efficiency within the first month of deployment.
5. Is AI for healthcare coding compliant with current regulations?
Yes. AI platforms are regularly updated to align with CPT, ICD, HCC, and payer-specific coding rules, ensuring compliance while maintaining accurate coding and documentation for all claims.
%201.png)