My Journey Before and After AI in Medical Coding
If you’ve ever worked in medical coding, you know the rhythm of it, chart after chart, code after code, and the pressure of getting each one right. Every number represents care delivered, time spent, and dollars reimbursed. Yet for years, much of that work depended on sheer focus and endurance.
When I look back on how far this field has come, it feels like two different careers. Before AI, coding was manual, repetitive, and mentally draining.
Today, it’s strategic, data-driven, and faster than I ever imagined. This is my journey, how AI changed not just how I code, but how I think about my work.
TL;DR
- AI in medical coding improves accuracy and consistency across complex charts.
- Coders now act as reviewers, auditors, and data collaborators, not just processors.
- Manual rework and denials drop as AI automates compliance checks.
- AI empowers coders to focus on strategy, quality, and continuous improvement.
Table of Contents:
- Before AI: The Manual Coding Era
- Early Automation: The Digital Transition Begins
- The Turning Point: My First Encounter with AI in Coding
- After AI: A New Way of Working
- The Human in the Loop: Why Medical Coders Still Matter
- Lessons from the Transition
- The Future of Medical Coding
- How AI Changed My Perspective
- Reflections for Fellow Coders
- Conclusion: Coders + AI = Smarter Healthcare
- FAQs
Before AI: The Manual Coding Era
When I began coding, everything was paper-based. Physicians wrote notes by hand, and coders like me sifted through scanned PDFs or image files, hunting for details line by line. My desk was covered in codebooks: CPT, ICD-10, and HCPCS, each essential, each updated annually.
We memorized thousands of codes and still cross-checked every one manually. The process was slow and error-prone. One missed modifier or incorrect sequence could delay a claim for weeks.
Consistency was the hardest part; two experienced coders might assign different codes to the same procedure simply because of interpretation differences.
Everyday Challenges in Manual Coding
- Endless reading and manual data entry
- Fatigue that increased the chance of small but costly errors
- Frequent payer audits and rework loops
- Pressure to meet daily productivity quotas without sacrificing accuracy.
Accuracy wasn’t just a performance metric; it was survival. A single mistake could trigger a denial, retraction, or compliance issue. Every chart demanded full attention, and by the end of the day, it felt like running a mental marathon.
Also Read: Impact of Clinical Documentation Improvement (CDI) in Healthcare
Early Automation: The Digital Transition Begins
When electronic health records (EHRs) became standard, coders felt hopeful. Digital access meant no more paper charts, no more endless filing cabinets. Early platforms like 3M, Coderyte, and Cerner made searching easier. I could type a keyword instead of flipping pages in codebooks.
But despite these improvements, coding was still entirely human. Software tools helped us find the right code faster, but they didn’t decide for us.
Every diagnosis and procedure still required interpretation and verification. We were the final word, and the workload didn’t shrink much.
The technology was new, but the process was the same. Coders still needed to interpret physicians’ notes, cross-reference payer rules, and manually input each result. It was better, but not yet transformational.
The Turning Point: My First Encounter with AI in Coding
Six months before joining RapidClaims, I had heard plenty about artificial intelligence, but I wasn’t sure what it meant for medical coding.
- Would AI really understand complex documentation, abbreviations, and handwritten notes?
- Could a system catch the nuances that experienced coders noticed instantly?
When I joined the RapidClaims team, I finally saw how AI fits into our world. The platform uses Natural Language Processing (NLP) to read clinical documentation and extract relevant information automatically. The system doesn’t guess, it learns from examples that coders like me review and refine.
At first, I was cautious. I compared its results against my own, chart by chart. What surprised me wasn’t just its accuracy but its consistency. It didn’t tire, miss context, or forget modifiers after a long day.
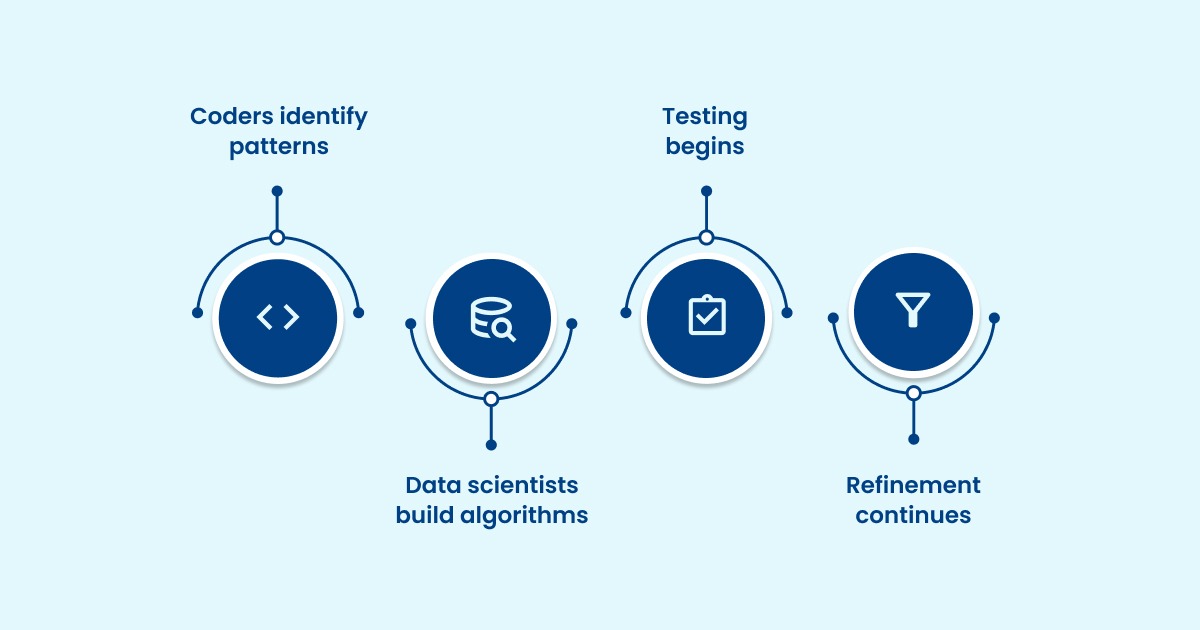
How AI Learns from Coders
The process behind the scenes is methodical and collaborative:
Alt text:How AI Learns from Coders
- Coders identify patterns and mark where critical data lives within charts.
- Data scientists build algorithms based on that feedback.
- Testing begins, comparing AI outputs against hundreds of manually coded examples.
- Refinement continues until accuracy consistently exceeds 98% before going live.
This partnership between coders and technology creates a feedback loop; each round of review makes the system smarter. Instead of fearing AI, I started to see it as my digital assistant, one that handled volume while I focused on quality.
Also Read: AI-Powered Automation in Medical Coding
After AI: A New Way of Working
Once AI became part of my daily workflow, everything changed. Tasks that used to take hours now took minutes.
The system could process hundreds of charts simultaneously while flagging only uncertain cases for my review.
It didn’t replace my judgment; it elevated it. I now spend less time searching for codes and more time validating, auditing, and improving compliance. I went from data entry to decision support.
The benefits ripple through the entire revenue cycle. Denials drop because coding accuracy improves. Claims move faster because fewer touchpoints exist. Financial leaders gain visibility through analytics dashboards that show patterns and outliers in real time.
Key Outcomes I’ve Seen

Alt text:Key Outcomes I’ve Seen
- Speed: Bulk chart processing with near-instant results
- Accuracy: Stable 98–99% coding precision across chart types
- Consistency: Standardized outcomes across coders and departments
- Cost Savings: Lower overhead with less manual rework
- Compliance: Built-in payer and CMS rule sets
These results don’t just make my work easier; they make the entire system more reliable. I trust the results because I helped train the process that delivers them.
Also Read: Choosing the Right Encoder for Medical Coding
The Human in the Loop: Why Medical Coders Still Matter
The most important thing I’ve learned is that AI doesn’t work without human guidance. Its accuracy depends on the quality and diversity of the data we feed it. The coder’s role has evolved from executor to collaborator.
We provide the context that algorithms can’t infer on their own, the “why” behind a diagnosis or procedure. AI handles volume, but coders provide oversight, judgment, and compliance understanding.
Today, my team focuses on validating exceptions, improving accuracy thresholds, and identifying cases that require physician queries. In short, AI helps us do more of the meaningful work and less of the repetitive kind.
The Modern Coder’s Skillset
- Analytical thinking and pattern recognition
- Deep understanding of coding standards and payer rules
- Quality assurance and data auditing
- Cross-functional collaboration with technical teams
Instead of fearing technology, coders are now learning to guide it. We’ve become essential partners in shaping how AI performs across healthcare operations.
Also Read: Basics of Medical Coding: A Beginner's Guide
Lessons from the Transition
Trusting AI wasn’t immediate. I compared its results against mine for weeks. But once I saw consistent accuracy, I realized how much time it saved, and how many errors it prevented.
AI also revealed inefficiencies we never noticed. It highlighted missing documentation and recurring claim errors, helping us fix root causes, not symptoms.
Today, our team talks less about speed and more about outcomes: fewer denials, higher accuracy, stronger compliance.
The Future of Medical Coding
AI is quickly becoming part of the workflow itself. Soon, EHRs will generate coding suggestions instantly, reducing turnaround times from hours to seconds.
Future coders will focus on high-value reviews and analytics, overseeing systems that learn continuously from payer feedback.
What’s next:
- Real-time coding within EHRs
- Autonomous coding for routine cases
- Predictive denial prevention
- Deeper compliance analytics
How AI Changed My Perspective
I entered coding to ensure accuracy. Today, I help systems achieve it at scale. The shift from manual work to intelligent collaboration made my job more meaningful.
AI freed time for problem-solving, analysis, and quality improvement. It turned coding from a repetitive task into a strategic function that supports revenue and patient care.
Coders remain essential; their insight is what makes AI better with every iteration.
Reflections for Fellow Coders
If you’re a medical coder wondering where you fit in this new landscape, here’s what I’ve learned:

Alt text:Reflections for Fellow Coders
- Stay curious. Every new system or workflow is an opportunity to grow.
- Collaborate actively. Your expertise shapes how AI performs; your feedback matters.
- Embrace change early. The sooner you adapt, the faster you’ll see results.
- Focus on quality, not volume. AI handles the volume; you ensure the quality.
AI gives you the bandwidth to do what humans do best: think critically, solve problems, and bring context to data.
Also Read: Becoming a Medical Coding and Billing Specialist: Steps to Get Certified
Conclusion: Coders + AI = Smarter Healthcare
AI hasn’t replaced coders; it’s elevated us. It’s given us tools to work faster, more accurately, and with greater confidence.
What this means for you:
- Less manual effort
- Stronger compliance
- Faster reimbursements
- Better use of coder expertise
AI doesn’t remove the human touch; it amplifies it.
If you’re ready to see how AI can enhance your team’s performance, explore how RapidClaims helps coders and healthcare organizations build the next generation of efficient, compliant medical coding.
FAQs
Q1. How does AI help in medical coding?
AI reads documentation, suggests accurate codes, and applies payer rules automatically to improve efficiency.
Q2. Will AI replace medical coders?
No. AI supports coders by handling repetitive tasks while humans ensure quality, compliance, and decision accuracy.
Q3. What skills do coders need in the AI era?
Coders need analytical thinking, compliance knowledge, and collaboration skills to train and validate AI systems.
Q4. How accurate is AI-assisted coding?
Modern platforms like RapidClaims achieve 98–99% accuracy after validation and continuous learning cycles.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
Top Products

%201.png)








