Top Billing Workflows Improved by Healthcare Workflow Automation

U.S. healthcare billing teams are under constant pressure to reduce denials and accelerate reimbursement while managing complex payer rules and limited staff. Yet many billing delays stem from preventable process failures rather than clinical issues. The HHS Office of Inspector General reports that nearly 75 percent of appealed Medicare Advantage denials are overturned, highlighting how often errors occur earlier in the billing workflow.
Healthcare workflow automation directly addresses these breakdowns by standardizing billing processes like eligibility checks, documentation validation, and claim readiness. By automating key steps, teams can reduce manual errors, improve accuracy, and accelerate cash flow. This article explores where workflow automation generates the greatest impact.
Key Takeaways
- Healthcare workflow automation streamlines billing by coordinating tasks such as eligibility checks, documentation validation, coding support, claim edits, submission and denial routing.
- Automating high-friction workflows reduces preventable errors, shortens reimbursement timelines and lowers administrative workload.
- The most valuable automation targets include eligibility verification, coding accuracy checks, claim readiness validation, submission tracking, denial routing and payment posting.
- Successful implementation requires mapping real workflow behavior, defining accurate rules, integrating with EHR and billing systems and building strong exception handling.
- Measuring clean claim rate, automation pass-through rate, denial patterns and payment posting lag helps verify ROI and refine workflows.
- Future automation trends involve AI-driven documentation alignment, predictive denial analytics, dynamic payer rule updates and automated audit preparation.
Table of Contents:
- Top Billing Workflows Improved by Healthcare Workflow Automation
- What Healthcare Workflow Automation Means for Billing and Revenue Cycle Teams
- Key Benefits of Healthcare Workflow Automation for Billing Performance
- How to Implement Healthcare Workflow Automation Across the Revenue Cycle
- Essential Metrics to Measure the Impact of Healthcare Workflow Automation
- Common Challenges When Adopting Healthcare Workflow Automation and How to Address Them
- Future Trends in Healthcare Workflow Automation for Billing Operations
- Why RapidClaims Is the Right Partner for Billing and RCM Workflow Automation
- Conclusion
- FAQs
What Healthcare Workflow Automation Means for Billing and Revenue Cycle Teams
Healthcare workflow automation refers to technology that organizes billing tasks, data inputs and decision points into a consistent, rules-driven sequence that operates with minimal manual effort. In the revenue cycle, this approach replaces fragmented steps with coordinated digital pathways that reflect payer policies, CMS guidance and internal compliance standards. As a result, teams reduce rework, avoid timing delays and move claims through the billing process with far greater reliability.
In revenue cycle operations, automation supports key stages such as:
- Eligibility and benefit verification
- Documentation capture and validation
- Coding support and coding accuracy checks
- Claim creation, editing and readiness validation
- Submission to payers and tracking of acknowledgments
- Denial routing and appeal preparation
- Payment posting and reconciliation
- Audit preparation and documentation assembly
While front-office automation can improve scheduling, intake and registration, the largest financial impact comes from automating back-office billing workflows. These are the steps that determine whether claims are complete, compliant and ready for submission; long before a payer evaluates medical necessity, coding accuracy or benefit structure.
When applied effectively, healthcare workflow automation reduces preventable errors, increases clean claim rates and helps revenue cycle teams maintain stable performance even during staffing shortages or volume spikes.
Key Benefits of Healthcare Workflow Automation for Billing Performance
Revenue cycle teams manage growing chart volumes, shifting payer rules and rising documentation demands. Manual workflows make these pressures more difficult to absorb, especially when accuracy and turnaround time determine reimbursement. Healthcare workflow automation helps stabilize billing operations by removing preventable errors, reducing rework and advancing claims through the cycle without unnecessary delays.
Cleaner Claims With Fewer Avoidable Errors
Automated workflows apply standardized rules during eligibility checks, documentation validation and coding review. This ensures key elements such as coverage details, required modifiers, supporting documentation and demographic data are complete before a claim reaches the payer. As a result, teams submit cleaner claims and reduce downstream edits.
Faster Progression From Coding to Payment
Once documentation or coding is completed, automation moves claims forward immediately instead of waiting in manual queues. This shortens the time between chart completion, claim assembly and payer submission and improves overall cycle efficiency.
Reduced Operational Load on Billing Teams
Tasks such as routing claims, checking for required elements or initiating status checks can run automatically based on predefined rules. Staff focus on higher-value activities including complex claims, follow-up work, appeals and quality improvement rather than repetitive administrative steps.
Better Denial Prevention and Follow-Up
Automation enforces payer requirements early in the process and flags issues before submission. When a denial occurs, workflows route it to the appropriate specialist with the needed context already attached, which reduces turnaround time for appeals.
Improved Compliance and Documentation Traceability
Every automated step produces a clear record of the actions taken on a claim. This supports internal compliance programs, aligns with CMS and payer audit expectations and helps organizations respond quickly to documentation or policy reviews.
Scalability Without Additional Staffing Pressure
Automated workflows can handle increased volumes caused by growth, seasonal spikes or staffing gaps. This allows organizations to maintain performance without expanding their labor footprint or overburdening existing teams.
How to Implement Healthcare Workflow Automation Across the Revenue Cycle
Successful automation begins with a clear understanding of how work actually moves through the revenue cycle. Many billing challenges come from undocumented dependencies, inconsistent routing and payer rules that staff manage informally. A strong implementation plan examines these realities, then builds automation that reflects the true flow of information, not the ideal version written in policy guides.
1. Map Real Workflow Behavior, Not the Policy Version
- Observe how coders, billers and follow-up teams actually complete tasks
- Track where claims wait for information, signatures or system updates
- Capture payer-specific behaviors that staff already compensate for manually
- Identify steps performed “off the system” in spreadsheets or email threads
2. Prioritize Workflows With the Highest Operational Friction
- Look for steps with recurring clarification requests or data mismatches
- Identify processes where payer rules frequently change or vary by plan
- Target areas where staff spend the most time reworking or revalidating claims
- Select workflows with long tail impact on cleaning claims or reducing write-offs
3. Translate Tribal Knowledge Into Machine-Readable Rules
- Document conditional logic staff use instinctively (for example, plan-specific authorization thresholds or modifier requirements)
- Standardize how exceptions are identified so automation can detect them
- Capture cross-department dependencies such as coding-to-billing handoff checks
4. Integrate Automation at Points Where Data Reliability Drops
- Connect to EHR and billing systems to pull structured data before staff modify it
- Use automation to validate documentation against coding and payer rules
- Ensure integration supports real-time updates so claims are not built on stale data
5. Design Exception Handling to Match Organizational Roles
- Route clinical documentation issues to coding, not to billing
- Send payer-policy denials directly to the denial or appeals specialist
- Flag documentation gaps immediately to the originating team, not downstream
6. Instrument Workflows With Metrics That Expose Hidden Failure Points
- Monitor where claims stall after automation is deployed
- Track which payers or service lines trigger the most exceptions
- Measure the percentage of claims that move through the workflow without manual intervention
- Use these insights to refine rules and eliminate friction points
7. Scale Automation Only After Proving Stability at Each Step
- Add new automated workflows only after error patterns stabilize
- Apply lessons from the first wave to specialty-specific or payer-specific workflows
- Expand to financial close, payment reconciliation or audit packet generation once upstream processes are reliable
If your billing team is managing rising denials or inconsistent workflow handoffs, RapidClaims can analyze a representative set of encounters to identify where workflow automation will create the highest operational value.
Essential Metrics to Measure the Impact of Healthcare Workflow Automation
Automation delivers value only when its results can be measured. The most useful indicators focus on how reliably claims move through the billing cycle, how often human intervention is still required and where payer friction continues to create delays. These metrics help revenue cycle leaders confirm whether automation is reducing administrative waste or shifting the burden to another part of the process.
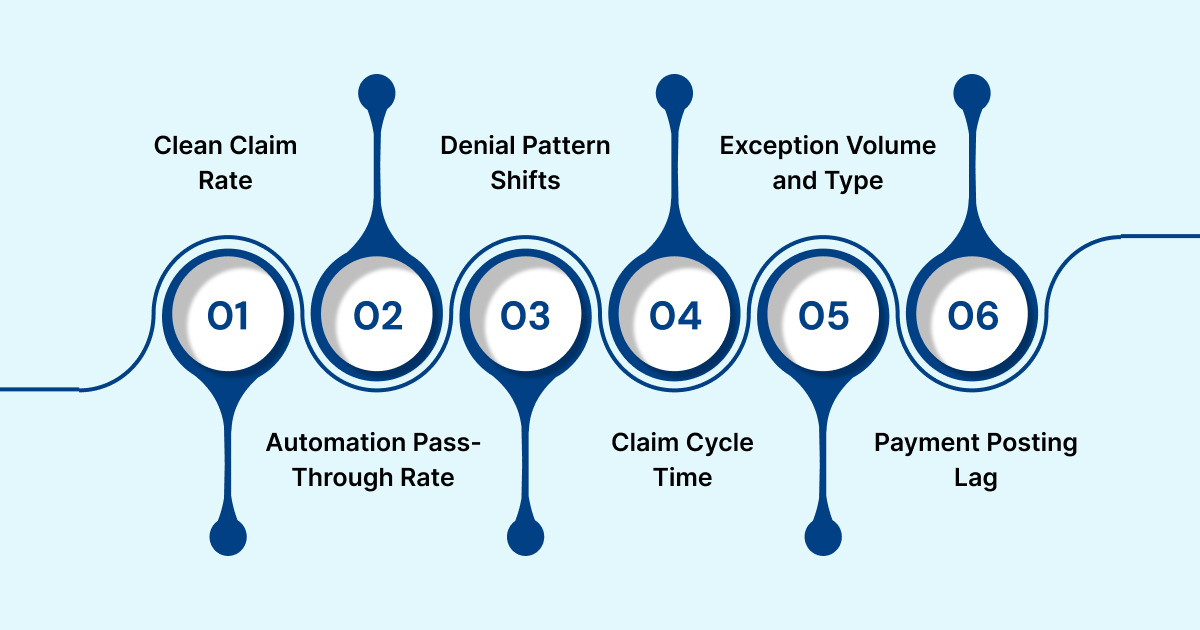
Clean Claim Rate
- Measures the percentage of claims accepted by payers without edits
- Reflects the accuracy of eligibility checks, documentation validation and claim assembly
- Signals whether upstream automation is preventing avoidable errors
Automation Pass-Through Rate
- Tracks how many claims move from coding to submission with no manual intervention
- Confirms whether rules, validations and data capture steps are functioning as intended
- Helps identify workflows that still require staff involvement
Denial Pattern Shifts
- Monitors changes in denial categories over time
- Shows whether denials are moving away from preventable reasons and toward unavoidable payer determinations
- Guides teams to refine rules where upstream gaps remain
Claim Cycle Time
- Measures the time from documentation completion to payer submission
- Highlights the impact of automated routing and real-time validation
- Helps organizations compare automated workflows with manual queues
Exception Volume and Type
- Identifies which issues still require review by staff
- Reveals where documentation gaps, coding inconsistencies or policy variations occur
- Provides direction for refining automation rules
Payment Posting Lag
- Tracks the time between receipt of payer remittances and completed payment posting
- Indicates whether automation is removing reconciliation delays
- Helps evaluate the stability of downstream billing processes
Common Challenges When Adopting Healthcare Workflow Automation and How to Address Them
Automation fails in revenue cycle operations when the underlying billing realities are oversimplified. Most breakdowns come from gaps in data, rules or operational alignment rather than from the technology itself. Addressing these pitfalls early helps automation run reliably and prevents new bottlenecks from forming.
Overlooking Hidden Dependencies in Billing Workflows
- Many billing steps rely on data or approvals that are not visible in system logs.
- Avoid this by mapping how information actually flows between coding, billing, clinical teams and EHR modules.
- Capture informal workarounds staff use, since automation must replace them, not disrupt them.
Automating Steps With Unstable or Incomplete Data
- Claims often fail when automation depends on documentation that arrives late or inconsistently.
- Protect workflows by validating data readiness before automation triggers and setting alerts for missing or incomplete elements.
Applying Rules That Do Not Reflect Payer Variation
- A rule set built from one payer does not translate to others.
- Build payer-specific logic to avoid overgeneralization, especially for plans with unique authorization, modifier or bundling requirements.
Routing Exceptions to the Wrong Teams
- When exceptions go to the wrong workqueue, claims stall again and automation loses credibility.
- Route documentation issues to coding, coverage issues to eligibility staff and payer-policy issues to denial specialists.
Ignoring the Need for Real-Time Monitoring
- Automation can mask problems if exceptions are not tracked.
- Monitoring dashboards should surface where claims stall, which payers generate the most stops and which rules need refinement.
Expanding Too Quickly Before Stabilizing Early Workflows
- Scaling automation before upstream issues are resolved multiplies errors.
- Lock in stable performance on a few workflows before adding more, and apply lessons learned to new areas.
Ready to build more predictable, error-resistant billing workflows? Request a personalized RapidClaims demo to see how automation and integrated validation improve claim accuracy, reduce rework, and accelerate reimbursement.
Future Trends in Healthcare Workflow Automation for Billing Operations
Revenue cycle automation is shifting from rule-based task management to intelligence-driven workflows that anticipate issues before they slow reimbursement. The next phase focuses on improving documentation quality, adapting to payer behavior and reducing the operational effort required to keep pace with policy changes. These advancements support a more predictable and efficient billing environment.
- AI-Supported Documentation Alignment: AI can identify missing or inconsistent details in the medical record before coding begins. This helps ensure documentation meets CMS and payer requirements, prevents downstream edits and reduces delays during claim assembly.
- Predictive Denial Scoring: Machine learning models can estimate the likelihood of denial based on documentation patterns, historical payer behavior and service-level characteristics. Claims with higher risk scores can be routed through enhanced review before submission.
- Dynamic Payer Rule Updates: Emerging systems can incorporate policy changes from payers and CMS into claim edits and validation logic in near real time. This helps billing teams keep rules accurate without manual updates and reduces errors caused by outdated guidance.
- Real-Time Payer Interaction: Faster access to eligibility data, acknowledgments and remittances supports more consistent claim progression. Real-time communication reduces waiting periods and supports more accurate follow-up efforts.
- Automated Audit and Appeal Packet Creation: Automation can assemble documentation from the EHR, billing system and communication logs into a complete packet for payer audits or appeals. This reduces administrative burden and shortens response times.
- Cross-Workflow Orchestration: The next generation of automation connects documentation, coding, claim creation and denial management within a single coordinated sequence. This creates continuity across the revenue cycle and reduces the risk of work shifting between teams without visibility.
Why RapidClaims Is the Right Partner for Billing and RCM Workflow Automation
RapidClaims is built specifically for the technical demands of U.S. healthcare billing, where automation must interpret payer rules, validate documentation and coordinate coding, edits and submission across multiple systems. The platform uses a structured rules engine and data validation logic that reflect real RCM operations instead of generic workflow templates.
Why RapidClaims stands out:
- Purpose-built rules for payer policies, modifiers, medical necessity and CMS guidance
- Automated validation of documentation and coding inputs before claim assembly
- Clean integration with EHR, PMS and clearinghouse systems for synchronized data flow
- Intelligent routing of denials and exceptions based on operational roles
- Full audit trail of every automated action for compliance and transparency
- Scalable architecture that adapts to new specialties, payer mixes and policy changes
See how RapidClaims streamlines billing workflows with precision and reliability. Request a demo to experience the platform in action.
Conclusion
Billing automation is ultimately about creating a revenue cycle that can adapt as fast as the environment around it. Payer rules evolve, documentation demands shift and staffing capacity changes month to month. Manual workflows are not built for that level of variability, but automated ones can absorb it, adjust to it and keep operations stable. When the revenue cycle runs on predictable, logic-driven workflows, teams gain the headroom to focus on improvement rather than firefighting.
The organizations that move early toward automation are positioning themselves for a billing landscape that will only grow more complex. The ones that wait risk building revenue operations on processes that cannot scale or respond to the next wave of regulatory or payer-driven change.
Ready to explore a more resilient billing workflow? Contact RapidClaims to request a demo and see what smart automation can unlock for your revenue cycle.
FAQs
Q: What is workflow automation in healthcare billing?
A: Workflow automation in billing uses technology to manage tasks, data and decisions across the claim lifecycle with minimal manual work. It organizes steps such as eligibility checks, coding review, claim creation, edits and submission into a consistent digital process.
Q: Which billing workflows benefit most from automation?
A: The highest value areas include eligibility and benefits verification, coding support, claim editing, submission and tracking, denial handling, payment posting and audit preparation.
Q: Does workflow automation replace billing and coding staff?
A: No. Automation manages routine and rules-based activities so staff can spend more time on complex claims, payer follow up, appeals and quality improvement.
Q: How does automation reduce denials?
A: Automated workflows apply payer rules, validate documentation and check coding accuracy before a claim is submitted. This prevents common errors that often trigger denials.
Q: What challenges do organizations face when automating billing workflows?
A: Typical challenges include inaccurate or incomplete rules, inconsistent data from the EHR, unclear exception routing and limited visibility into where claims stall.
Q: How does automation support compliance and audits?
A: Automated workflows create a complete record of each action taken on a claim. This provides clear traceability and makes it easier to support payer audits and internal compliance reviews.
Q: What should organizations look for in a billing automation platform?
A: Key features to look for include payer-specific rule support, reliable integrations with EHR and billing systems, real-time monitoring, strong exception handling and audit-ready reporting.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








