Top 20 Denial Codes in U.S. Medical Billing (2026 Guide)
You deal with denial codes every day, and each one results in delayed payments, additional rework, and pressure from stakeholders who expect faster reimbursement outcomes. What should be a simple claim resolution process often turns into repeated follow-ups, payer confusion, and time spent correcting issues that should never occur.
Data shows this problem is widespread, not isolated to one specialty or payer type across the healthcare system. According to HealthCare.gov, insurers denied nearly one out of every five in-network claims and 37 percent of out-of-network claims during 2023.
In this blog, we'll explore the most common denial codes, explain why they occur, outline how to handle them by category, and share steps to reduce future denials.
Key Takeaways:
- Denial codes like CO-16, CO-18, and CO-29 often signal preventable data, duplicate, or filing deadline issues.
- Codes such as CO-4, CO-11, and CO-97 point to coding, modifier, or bundling problems that require closer review.
- Authorization-related denials, including CO-197 and CO-198, reflect gaps in preapproval tracking and limit monitoring.
- Coverage-based denials like CO-27, CO-50, and CO-109 highlight eligibility and insurance verification gaps.
- Using denial patterns from codes like CO-45 and CO-167 helps teams adjust billing workflows and reduce repeat denials.
How Payers Communicate Claim Denials: CARCs and RARCs
When a claim gets denied or reduced, payers rely on standardized codes to explain payment decisions across remittance documents you review daily. These codes appear on explanation of benefits and electronic remittance advice files, giving structured reasons for nonpayment or partial payment outcomes.
Here are the two code types you see most often and how each one supports denial analysis:
1. Claim Adjustment Reason Codes (CARCs)
CARCs explain why a claim line was denied, reduced, or adjusted based on coverage rules, coding issues, or payer policies.
They describe the primary payment decision, such as missing information, non-covered services, authorization failures, or billing errors tied to the claim.
2. Remittance Advice Remark Codes (RARCs)
RARCs give extra detail that clarifies the CARC message and points to specific payer instructions or documentation requirements. They often explain what correction is needed, what policy applies, or why an appeal may or may not succeed.
How CARCs and RARCs Work Together
CARCs provide the main denial reason, while RARCs supply context that helps billing teams decide next steps. Reading both codes together prevents misinterpretation and reduces time wasted on incorrect resubmissions or unnecessary appeals.
After learning how payers communicate denials, examining the most common denial codes shows where billing teams spend the most effort.
Also Read: A Comprehensive Guide on Medical Coding: Here is What You Need to Know
20 Most Common Denial Codes in U.S. Medical Billing
Denial codes represent specific payment decisions that point to process gaps, documentation errors, or payer rule mismatches affecting reimbursement timelines. When you understand each code in detail, you can respond with targeted corrections instead of repeating submission mistakes.
Here are the most common denial codes you encounter, explained with causes, impact, and corrective direction for stronger claim outcomes:
1. CO-4: Missing or Incorrect Modifier
This denial occurs when required modifiers are missing, invalid, or inconsistent with the reported procedure and billed circumstances. Review payer modifier rules, confirm procedural distinctions, and validate documentation supports modifier usage before resubmitting the claim.
2. CO-11: Diagnosis Inconsistent With Procedure
Payers apply this code when diagnosis codes fail to justify medical necessity for the billed service under policy guidelines. Confirm diagnosis selection supports the procedure, aligns with payer policies, and matches provider documentation before correction or appeal.
3. CO-16: Missing or Incorrect Information
This code signals incomplete claim data, often involving demographics, provider identifiers, service dates, or required supporting fields. Perform a full claim audit, correct missing fields, and confirm data accuracy prior to resubmission to prevent repeat denials.
4. CO-18: Duplicate Claim or Service
This denial indicates that the payer system identifies the claim or service line as having been previously submitted or already processed. Check remittance history, confirm prior adjudication, and avoid unnecessary resubmissions that create duplicate billing flags.
5. CO-22: Coordination of Benefits Information Missing
Payers issue this code when primary or secondary insurance information is missing, outdated, or entered incorrectly. Verify coverage order, update insurance details, and submit required explanation of benefits from the primary payer when applicable.
6. CO-27: Patient Coverage Terminated
This denial appears when insurance coverage was inactive on the service date, regardless of prior eligibility checks. Review eligibility verification timing, confirm termination dates, and determine patient responsibility or alternative coverage options.
7. CO-29: Timely Filing Limit Exceeded
This code applies when claims are submitted outside payer-defined filing deadlines, eliminating payment eligibility. Track payer-specific timelines closely and escalate delayed claims early to avoid irreversible revenue loss.
8. CO-45: Charges Exceed Fee Schedule
Payers assign this code when billed charges exceed contracted or allowable reimbursement limits. Review contract terms, adjust charge expectations, and confirm allowed amounts during posting and reconciliation processes.
9. CO-50: Medical Necessity
This denial indicates the payer does not deem the service medically necessary based on the diagnosis or clinical data provided. Review clinical notes against payer coverage policies, ensure the diagnosis code accurately reflects the patient's condition, and appeal with supporting records if the service was clinically justified.
10. CO-96: Non-covered Charges
This code indicates specific charge lines are excluded under payer rules, even when other services on the same claim remain payable. Distinct from CO-109 (claim not covered by this payer), CO-96 applies at the line-item level. Review line-level coverage rules and adjust billing practices to prevent recurring non-covered charge submissions.
11. CO-97: Service Included in Another Procedure
Payers use this code when billed services are bundled into another reimbursable procedure. Confirm bundling rules, apply correct modifiers when allowed, and avoid separate billing for inclusive services.
12. CO-109: Claim Not Covered by This Payer
This denial appears when the submitted payer is not financially responsible for the claim. Verify insurance selection accuracy and redirect claims to the correct payer based on coverage coordination.
13. CO-119: Benefit Maximum Reached
This code applies when patients exhaust plan benefits for specific services within a defined coverage period. Proactively track benefit usage and inform patients about coverage limits before scheduling additional services.
14. CO-125: Submission Exceeds Allowed Units
Payers issue this code when billed units exceed frequency or quantity limits defined by policy. Review utilization limits, validate units billed, and confirm documentation supports exceptions when permitted.
15. CO-167: Service Not Covered for This Diagnosis
This denial reflects diagnosis-specific exclusions, even though the service may be covered for other conditions. Confirm diagnosis compatibility with coverage policies and update coding selections when documentation supports alternatives.
16. CO-170: Payment Denied Based on Provider Type
This denial occurs when the billing provider is not eligible to be reimbursed for the specific service rendered due to credentialing or scope-of-practice issues. Verify that the provider is credentialed with the payer and that the service code billed is permitted for their specific provider specialty.
17. CO-197: Precertification or Authorization Required
Payers apply this denial when required authorization was never obtained before service delivery. Strengthen front-end authorization workflows to prevent services from rendering without required approvals.
18. CO-198: Precertification or Authorization Exceeded
This code reflects services exceeding authorized limits, including visits, units, or approved service periods. Monitor authorization usage closely and request extensions when additional services become clinically necessary.
19. CO-200: Expenses Incurred During Lapse in Coverage
This code signals that the patient had a gap in insurance coverage, specifically on the date of service, even if they had coverage before or after. Re-verify the patient's specific enrollment dates and determine if the patient is financially responsible for the visit.
20. CO-204: Service Not Covered Under Current Policy
Payers use this code when updated policies exclude services previously reimbursed under older guidelines. Stay informed on payer policy changes and adjust billing practices to align with current coverage rules.
Seeing individual denial codes is helpful, yet grouping them by cause helps you respond more consistently across similar billing issues.
How to Handle Denial Codes by Category
Not all denial codes require the same response, and treating them identically often leads to wasted effort and missed reimbursement opportunities. Grouping denial codes by category helps you identify root causes faster and apply consistent corrective actions across billing, coding, and front-end workflows.
Here are the most common denial code categories, along with their causes and recommended handling approach:
Handling denial codes by category creates consistency across teams and reduces confusion during follow-up activities. This approach also helps billing leaders spot recurring breakdowns that require workflow corrections rather than repeated claim-level fixes.
Once you identify the category behind a denial, clear post-denial steps help ensure timely and appropriate follow-up actions.
Also Read: Intro to Commonly Used Medical CPT/HCPCS Codes List
What to Do After a Claim Denial?
Once a denial appears, your response timing and accuracy directly affect the potential for reimbursement and the downstream workload for billing and follow-up teams. A structured post-denial process helps you avoid repeat errors, missed appeal windows, and unnecessary resubmissions that drain staff time.
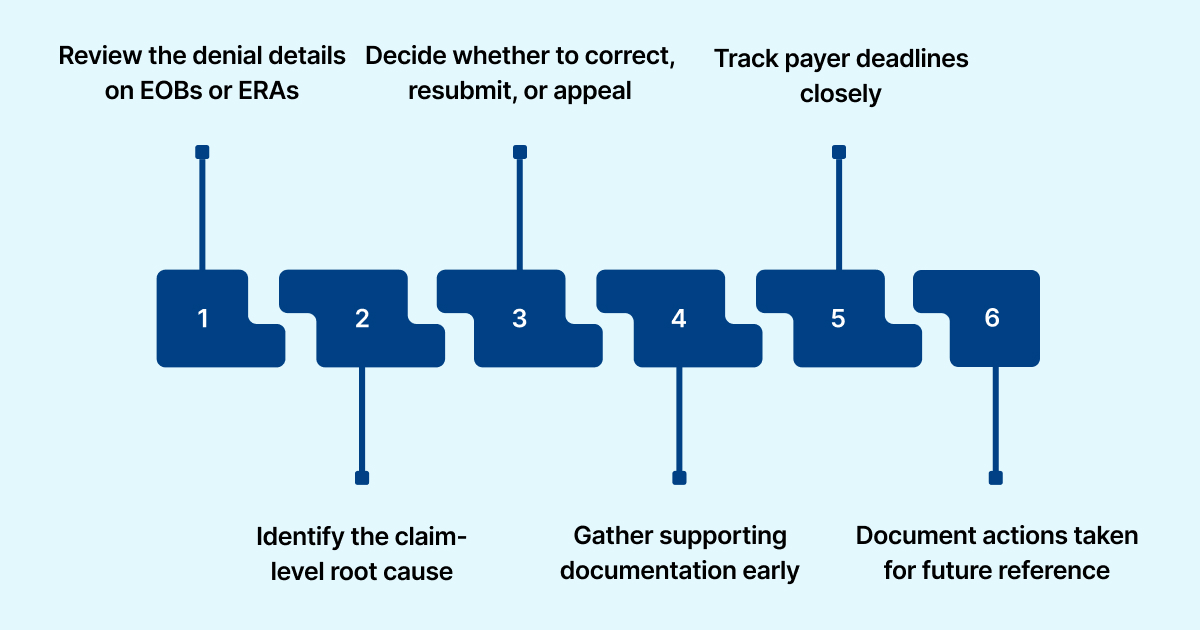
Here are the key steps you should follow after receiving a claim denial:
- Review the denial details on EOBs or ERAs: Start by reviewing the denial code, adjustment reason, and remark codes listed on the explanation of benefits or electronic remittance advice.
- Identify the claim-level root cause: Determine whether the denial stems from eligibility, authorization, coding, timely filing, or medical necessity before taking corrective action.
- Decide whether to correct, resubmit, or appeal: Choose the next step based on payer rules, denial type, and whether documentation supports reconsideration or correction.
- Gather supporting documentation early: Collect clinical notes, authorization records, referrals, and policy references required to support corrected claims or appeal submissions.
- Track payer deadlines closely: Monitor appeal and resubmission timelines to prevent lost reimbursement due to missed filing or reconsideration limits.
- Document actions taken for future reference: Record denial outcomes and corrective steps to support reporting, compliance reviews, and trend analysis across denial categories.
Handling individual denials matters, yet long-term improvement depends on practices that reduce repeat issues across your billing operation.
Also Read: Common Medical Billing and Coding Errors and How to Protect Your Practice
Best Practices That Reduce Claim Denials
Long-term denial reduction depends on consistent processes supported by data visibility across coding, documentation, and claim submission activities. Teams relying only on manual reviews often miss patterns that signal deeper workflow issues affecting reimbursement outcomes.
Here are practical actions that help control current denials while reducing future claim rejections at scale:
- Assign Clear Ownership For Denial Follow-Up: Each denial category should have a defined responsibility, so issues receive timely review and consistent corrective handling.
- Track Denials Using Centralized Analytics: Systems that consolidate denial data across payers and services help identify repeat failure points faster than manual logs.
- Use Pre-Submission Checks Beyond Basic Edits: Advanced claim reviews that assess coding accuracy, coverage rules, and authorization alignment reduce preventable denials before submission.
- Connect Documentation Review With Billing Outcomes: Linking clinical documentation feedback to denial trends helps reduce medical necessity and diagnosis-related rejections.
- Prioritize High-Risk Claims Before Submission: Predictive indicators allow teams to focus attention on claims most likely to face payer rejection.
- Apply Feedback Loops From Denials To Front-End Teams: Denial outcomes should inform registration, clinical, and coding teams through structured reporting and targeted education.
- Support Follow-Up Teams With Guided Workflows: Worklists driven by denial reasons and payer rules help staff act faster and more consistently across large claim volumes.
Many of these practices rely on visibility and consistency, which becomes harder to maintain without technology support across the claim lifecycle.
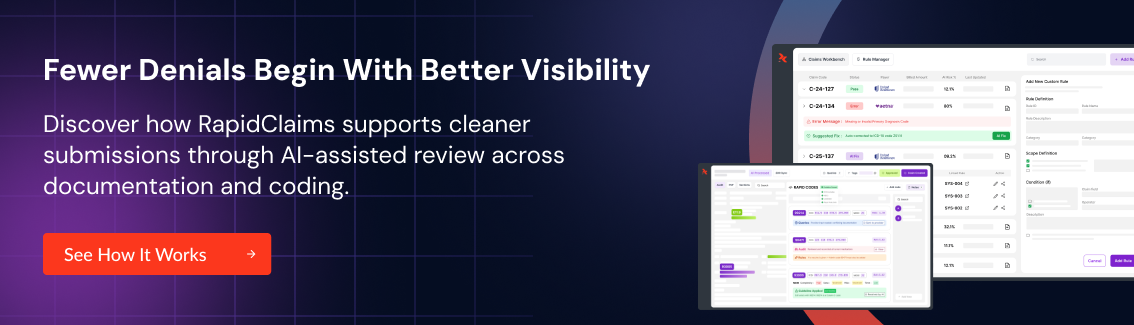
How RapidClaims Supports Denial Prevention and Recovery
Many denial issues stem from disconnected workflows, inconsistent payer rules, and limited visibility across coding, documentation, and follow-up activities. Technology that connects these functions can reduce avoidable denials while giving billing teams clearer direction on corrective actions.
Here are the core RapidClaims capabilities that align with denial management needs discussed throughout this blog:
RapidCode™: Autonomous Medical Coding Support
RapidCode reviews clinical documentation and assigns ICD-10, CPT, and E/M codes at scale with consistent accuracy across specialties. By reducing coding variation and manual rework, this capability helps limit downstream denials tied to diagnosis mismatches, modifiers, and bundling rules.
RapidCDI™: Clinical Documentation Integrity Support
RapidCDI analyzes encounter documentation and highlights risk adjustment, quality, and documentation gaps before claims move forward. This support reduces medical necessity denials and improves diagnosis support without increasing physician documentation burden.
RapidScrub™: Denial Prevention Before Submission
RapidScrub applies payer-specific edits, eligibility checks, and authorization validation before claims reach the clearinghouse. By identifying high-risk claims early, billing teams can correct issues that commonly trigger eligibility, authorization, and policy-based denials.
Together, these capabilities support a more controlled approach to coding accuracy, documentation quality, denial prevention, and recovery follow-up. This structure helps organizations reduce repeat denials while improving visibility into where revenue loss occurs across the claim lifecycle.
Conclusion
Denial codes offer clear signals when claims fail, and consistent interpretation helps teams respond faster while reducing repeated billing breakdowns. By combining code knowledge, category-based handling, and structured follow-up, organizations gain better control over reimbursement outcomes.
If your team needs support in reducing denials and improving visibility across coding, documentation, and recovery, RapidClaims can help.
Contact us today to discuss your denial challenges and request a personalized walkthrough of our revenue cycle intelligence platform.
FAQs
1. How do payer edits affect coding-related denial codes?
Payer edits apply diagnosis, modifier, and bundling logic that may differ from general coding guidelines. Coders should review payer bulletins regularly to avoid mismatches that trigger avoidable denials.
2. Should coders review denied claims after submission?
Yes, reviewing denials helps coders identify recurring documentation or code-selection issues. This feedback improves future claim accuracy and reduces repeat denials tied to similar services.
3. Which denial codes should be prioritized for follow-up first?
Denials with appeal potential, high dollar value, or frequent recurrence should receive early attention. Prioritization helps teams focus effort where reimbursement recovery remains realistic.
4. How can denial data support staffing and workload planning?
Denial trends reveal where breakdowns occur and which teams face repeated rework. Managers can use this insight to adjust workflows, assign ownership, and justify resource allocation.
5. Can repeated denial codes indicate compliance risk?
Yes, recurring denials tied to medical necessity, documentation gaps, or authorization issues may signal compliance exposure. Monitoring these patterns supports corrective action before payer audits or regulatory reviews occur.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






